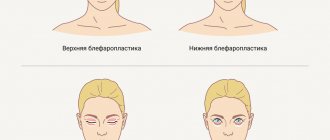
Age-related changes, congenital imperfections, fat deposits in the upper eyelids make the look tired and expressionless. Cosmetic imperfections often become the cause of self-doubt, complexes, and dissatisfaction with appearance. Blepharoplasty is a surgical operation that allows you to restore a youthful and open look, change the shape and shape of the eyes, correct asymmetry, congenital defects and solve other personal problems.
Methods for correction of the periorbital zone
Modern aesthetic medicine offers various techniques for solving individual problems or complex rejuvenation and correction of the eye area. Depending on individual indications, anatomical features and wishes of the patient, Damas Clinic doctors recommend effective and safe techniques.
- Classic blepharoplasty is aimed at aesthetic rejuvenation.
Indicated for excess thinning skin, fatty hernias, and age-related ptosis of the upper eyelids. During the procedure, access is formed at the border of the moving and fixed zones. As a result, the scar is completely hidden in a natural skin fold and is completely invisible. The doctor performs resection of fatty hernias and excess skin, returning the original eye contour and youthful look.
- Complex surgery allows you to simultaneously eliminate age-related changes and correct asymmetry caused by congenital pathologies, injuries, surgical interventions or other factors.
The doctor eliminates the reasons that disturb the harmony of the face and makes the look attractive.
- Europeanization of Asian upper eyelids involves the formation or strengthening of a natural fold, eliminating excess volume in the periorbital area.
During the operation, the doctor excises a spindle-shaped flap of skin and a strip of muscle 2-3 mm wide, modeling the desired incision and shape of the eyes.
- Canthopexy can be performed separately or in combination with classical rejuvenation surgery.
The procedure is aimed at changing the shape and shape of the eyes from Oriental to European or vice versa by tightening the outer and inner corners.
Surgery and rehabilitation period
Surgical eyelid correction can be performed under either local or general anesthesia. The duration of the operation is from 30 minutes to 1 hour.
The recovery period after blepharoplasty is quite short. There is virtually no pain during the rehabilitation period. On the third day after the operation, the sutures are removed, and after two weeks the bruises and swelling disappear without a trace. A week after the operation, you can already apply makeup.
The combination of blepharoplasty with a check-lift (an operation that eliminates sagging skin and shifts the muscle complex of the cheeks upward) allows you to get excellent results with minimal surgical intervention. Both operations are performed through a neat incision under the eyelash edge, which heals almost without a trace.
In most cases, the scarring process in the area of incisions performed during eyelid surgery occurs without complications and does not require additional measures to improve the quality of the scars. Sometimes, in order to speed up rehabilitation, a course of physiotherapeutic treatment is prescribed.
Who is the procedure suitable for?
Indications for intervention include age-related changes and congenital pathologies of the upper eyelid:
- loose overhanging skin;
- wrinkles, creases and folds;
- fatty hernias;
- overhanging soft tissues, provoking the effect of a sad and tired look;
- congenital or acquired asymmetry;
- hypertrophy of the circular muscles in the periorbital zone;
- swelling;
- turning of the eyelids.
In some cases, cosmetic imperfections cause both psychological and physical discomfort. Over time, upper eyelid ptosis can lead to blurred vision, drooping eyelashes, and eye irritation. The constant need to strain the facial muscles to keep the eyes open leads to the formation of wrinkles on the forehead, in the area of the nasolabial folds and other areas.
Contraindications:
- pregnancy and lactation;
- increased intracranial or intraocular pressure;
- myopathy;
- corneal infections;
- impaired blood clotting;
- oncological pathologies;
- exacerbation of chronic diseases and infections;
- rehabilitation after ophthalmological interventions.
| Facial plastic surgery – Dr. Amjad Al-Yousef | |
| Upper blepharoplasty (eyelid surgery) | 95,000 rub. |
| Eyelid surgery with canthopexy | RUB 105,000 |
| Upper eyelid surgery with asymmetry correction | RUB 105,000 |
| Facial plastic surgery - Anna Petrovna Pershukova | |
| Upper blepharoplasty (eyelid surgery) | 55,000 rub. |
| Upper eyelid surgery with asymmetry correction | 60,000 rub. |
| Facial plastic surgery - Dr. Youssef Bassanovich Dergam Prices include a promotion with a 50% discount with permission to publish the results of photos and videos | |
| Upper blepharoplasty (eyelid surgery) | 40,000 rubles instead of 80,000 rubles |
| Upper eyelid surgery with asymmetry correction | 45,000 rubles instead of 90,000 rubles |
| Facial plastic surgery - Dr. Ivan Pavlovich Chesalin Prices include a promotion with a 50% discount with permission to publish the results of photos and videos | |
| Upper blepharoplasty (eyelid surgery) | 40,000 rubles instead of 80,000 rubles |
| Upper eyelid surgery with asymmetry correction | 45,000 rubles instead of 90,000 rubles |
results
The effectiveness of intrapalpebral injection.
All 37 patients (40 eyes) of group 1 had lagophthalmos (non-closure of the palpebral fissure) of varying severity (from 1 to 8 mm), exposure keratopathy in the lower third of the cornea of varying severity, or superficial peripheral opacities of the cornea that did not affect visual acuity In 7 cases, corneal erosion was observed, and in 1 case, a corneal ulcer was observed. In addition, all patients complained of pain, discomfort, a feeling of sand, burning in the eye on the affected side, hyperemia and lacrimation.
Depending on the etiology of lagophthalmos, patients were divided into 3 clinical subgroups.
Subgroup 1A included 10 people (10 eyes) with lagophthalmos caused by acute paralysis of the facial nerve. The average age of the patients was 59.4 years (from 31 to 72 years), the average duration of paralysis was 1.7 months (from 1 to 3 months), the average volume of injected filler was 0.32 ml (0.1-0.5 ml).
Subgroup 1B consisted of 20 patients (20 eyes) with chronic paralytic lagophthalmos. In 14 of them, lagophthalmos was a consequence of removal of an acoustic neuroma, in 3 it was a result of traumatic injury, in 2 it was a result of acute cerebrovascular accident, and in 1 it was a complication of diabetes mellitus. The average age of the patients was 68.3 years (from 31 to 72 years), the average duration of paralysis was 36.7 months (from 4 to 78 months), the average volume of injected filler was 0.36 ml (0.1-1.2 ml).
Subgroup 1 B included 7 patients (10 eyes) with lagophthalmos due to endocrine ophthalmopathy (EOP) with a disease duration of more than 2 years in the inactive stage, of which 3 patients (3 eyes) had previously undergone bone-fatty decompression of the orbit and surgical correction of retraction century The average age of patients was 56.5 years (from 42 to 78 years), the average volume of injected filler was 0.17 (0.1-0.4 ml).
In subgroup 1A, immediately after injection of the drug and throughout the entire period of long-term follow-up, all patients showed a statistically significant decrease in the value of lagophthalmos and MRD1. At the end of the long-term follow-up period, the MRD1 value did not reach the initial value, however, without the development of clinically significant ptosis. When assessing the mobility of the upper eyelid in this subgroup, a significant increase was noted immediately after filler injection. After 2 months, a decrease in the excursion value was noted, but by the 12th month, pre-injection values were not achieved (Fig. 2).
Rice. Fig. 2. Dynamics of changes in lagophthalmos (a), MRD1 (b) and upper eyelid excursion (c) before and after GHA injection in patients with acute facial paralysis. Here and in Fig. 3: * — p<0.05; ** — p<0.001.
Contrary to the results obtained, it is quite difficult to assess the long-term effect of filler injection for the correction of lagophthalmos in acute facial paralysis due to the gradual restoration of the function of the orbicularis oculi muscle in all patients in this subgroup. However, in the acute stage of the disease, the effectiveness of the injection is undeniable.
In subgroup 1B, a statistically significant decrease in the severity of lagophthalmos and MRD1 was also recorded throughout the entire period of long-term follow-up. The excursion of the upper eyelid in this subgroup significantly increased after injection of the drug (Fig. 3).
Rice. 3. Dynamics of changes in lagophthalmos (a), MRD1 (b) and upper eyelid excursion (c) before and after GHA injection in patients with chronic paralytic lagophthalmos. * — p<0.05; ** — p<0.001. The average duration of effect of one injection of HGA was 9.05 months. A gradual decrease in the effect in all patients was observed from the 6th month of observation. Thus, by the 6th month the indicators reached pre-injection values in 10 patients, by the 9th month - in 13 patients, by the 12th - in 14 patients. The residual effect of the injection in 6 (30%) patients persisted for over 12 months.
At 4 and 6 months after filler injection, 2 (10%) patients with chronic lagophthalmos were excluded from the study due to surgical correction of lagophthalmos using a permanent gold weighting implant. In these cases, during surgery, a biopsy of a fragment of eyelid tissue from the area of GGC injection was sent for histological examination. According to the morphological results, the filler was located in a cellular depot, delimited by collagen septa of varying thickness, which correlated with the data of our previously published experimental study (Fig. 4)
Rice. 4. Histological picture of the upper eyelid biopsy. GHA depot 6 months after injection. Asterisks indicate HHA particles in the thickness of the depot, surrounded by connective tissue partitions (indicated by an arrow). [8].
In subgroup 1B, a statistically significant decrease in the magnitude of lagophthalmos and MRD1 was noted throughout the entire period of long-term follow-up. The median value of lagophthalmos returned to baseline values 12 months after injection, however, 2 (28%) patients (4 eyelids) still had complete correction of lagophthalmos even one year after injection. From the anamnesis of these patients, it is known that 5 years before the development of image intensification, they underwent upper and lower blepharoplasty for cosmetic reasons (Fig. 6).
Rice. Fig. 6. View of patient L., 48 years old, with image intensifier, lagophthalmos and retraction of the upper eyelids of both eyes before (a) and 6 months after (b) injection of GG. All patients also showed a statistically significant increase in the mobility of the upper eyelid after the injection, which, however, was less pronounced compared to the same indicator in patients from the subgroup with chronic paralytic lagophthalmos (Fig. 5).
Rice. 5. Dynamics of changes in lagophthalmos (a), MRD1 (b) and upper eyelid excursion (c) before and after GHA injection in patients with endocrine ophthalmopathy. * — p=0.05. In the subgroup of patients with EOP, the average duration of the effect of one injection was 10.67 months.
According to the correlation analysis, a statistically significant correlation was registered between the volume of the administered drug and the magnitude of lagophthalmos in subgroups 1A and 1B at 2 weeks ( R
=0.712;
p
=0.021 and
R
=0.524;
p
=0.018, respectively), 1 month (
R
=0.780;
p
=0.008 and
R
=0.555;
p
=0.011) and 2 months (
R
=0.666;
p
=0.036 and
R
=0.479;
p
=0.038) after injection. The correlation between the magnitude of lagophthalmos and filler volume in the subgroup of patients with EOP was statistically insignificant at all follow-up periods.
Within 2 weeks after the injection, all patients noted swelling and hyperemia of the upper eyelid, as well as isolated subcutaneous hemorrhages of varying severity. These undesirable effects did not affect the long-term outcome of the injection and did not require additional therapy. In this case, swelling, hyperemia and subcutaneous hemorrhages should be considered as a natural local reaction to the administration of the drug associated with damage to the skin by the needle/cannula (Fig. 7, a).
Rice. 7. Adverse events after intrapalpebral injection. a - swelling, hyperemia and subcutaneous hemorrhages; b — contouring of the drug depot.
In 7 patients, contouring of the drug depot was noted when filler was administered in a volume of more than 0.3 ml (see Fig. 7, b). However, its presence was not accompanied by complaints in any of the patients. In this case, the injected drug could be visualized subcutaneously in a blue-blue color for several months, which is due to the so-called Tyndall effect due to light refraction.
The effectiveness of intraorbital injection.
To evaluate the effectiveness of injection of GHA into the orbit in patients with enophthalmos of various etiologies, 20 patients were recruited, the average age of which was 45.5 years (from 24 to 76 years), the average volume of the injected drug was 1.8 ml (1-3 ml).
The causes of insufficient orbital volume were: previously operated severe traumatic deformity with implant placement (alloplant or demineralized bone autoimplant (DCAI)) and residual enophthalmos (8 orbits), silent sinus syndrome (1 orbit), hemifacial atrophy syndrome (1 orbit) - these patients formed subgroup 2A. All patients with operated traumatic orbital deformity underwent CT of the orbits to exclude unconsolidated defects of the bone walls, which could lead to filler dislocation. All patients complained of a cosmetic defect due to retraction of the eyeball; 2 patients had exposure keratopathy, accompanied by hyperemia and lacrimation due to non-closure of the palpebral fissure, caused by limited mobility of the upper eyelid on the affected side.
Subgroup 2B included 10 patients with anophthalmic syndrome who had previously undergone surgery with the formation of a musculoskeletal stump, but satisfaction with the cosmetic result was low.
All patients of the 2nd group had slight enophthalmos/retraction of the prosthesis (from 1 to 4 mm), deepening of the superior orbitopalpebral groove, hypophthalmos (from 1 to 2 mm), lagophthalmos (from 1 to 2 mm), limited mobility of the upper eyelid compared with the healthy side (difference (D) in upper eyelid mobility), which improved after the ocular compression test due to repositioning of the eyeball.
After injection of filler into the orbit according to the proposed method, all patients in subgroup 2A showed a positive effect, accompanied by reposition of the eye and a decrease in the retraction of the superior orbitopalpebral groove (Fig. 8).
Rice. 8. View of patient K., 76 years old, with post-traumatic enophthalmos on the left before and 6 months after the injection. a - position with head thrown back; b - look straight; c - look down. In 6 (60%) patients, complete correction of enophthalmos was achieved; in other cases, the residual enophthalmos did not exceed 1 mm. In 3 (100%) patients with hypophthalmia, complete correction was achieved.
A statistically significant decrease in the effect of the drug was recorded 9 months after the injection, however, the median enophthalmos did not reach the initial values. Patients in this subgroup also showed a statistically significant increase in mobility (decrease in D) throughout the entire period of long-term follow-up. Starting from the 9th month after the injection of GHA, this indicator gradually decreased towards the end of the long-term observation period, but did not reach the initial values (Fig. 9, a).
Rice. 9. Dynamics of changes in enophthalmos, retraction of the prosthesis and differences in the excursion of the upper eyelid compared with similar parameters of the healthy eye before and after injection of HHA in patients with enophthalmos (a) and anophthalmic syndrome (b). * — p=0.05. Maintenance of the injection effect over 18 months was observed in 3 (33%) patients.
In subgroup 2B, patients showed a significant decrease in the amount of retraction of the prosthesis and a statistically significant improvement in the excursion of the upper eyelid within 9 months after the GHA injection. After this period, a gradual decrease in the effect was recorded by the 18th month of the long-term observation period (see Fig. 9, b). However, the amount of retraction of the prosthesis and mobility of the upper eyelid did not reach the initial values. In 4 (20%) patients in this subgroup, the effect persisted for more than 18 months of follow-up.
In subgroup 2A, according to the correlation analysis, a statistically significant relationship was identified between the magnitude of enophthalmos and hypophthalmos and the volume of the administered drug immediately after injection of the drug ( R
=0.757;
p
=0.049 and
R
=0.806;
p
=0.029, respectively).
A statistically significant correlation was established between the volume of the drug and the change in the mobility of the upper eyelid immediately after the injection of GHA ( R
= 0.835;
p
= 0.019), after 3 (
R
= 0.816;
p
= 0.025), 6 (
R
= 0.899;
p
= 0.006) and 9 (
R
=0.874;
p
=0.01) months after drug administration. At the remaining periods of long-term follow-up, no statistically significant correlation was registered between these indicators.
In subgroup 2B, a statistically significant correlation was noted between the amount of retraction of the prosthesis and the volume of the injected drug immediately after the injection of GHA ( R
=0.722;
p
=0.043) and at all stages of the long-term follow-up period: after 3 and 6 months (
R
=0.722;
p
=0.043), 9 (
R
=0.932;
p
=0.001), 12 (
R
=0.866;
p
=0.005) and 18 (
R
=0.709;
p
=0.049) months, but not with a change in the excursion of the upper eyelid.
Clinically significant complications during or after the procedure were not recorded in any patient. Patients reported a feeling of moderate discomfort and pressure during the injection. There were no cases of implant dislocation subcutaneously or into periorbital structures. Patients from subgroup 2A complained of slight double vision in the extreme periphery, upon the appearance of which the injection was stopped. Double vision regressed within 24 hours after drug administration.
The described adverse events that occurred after intrapalpebral or intraorbital injections did not affect the effectiveness of the drug. Serious side effects such as hypersensitivity reaction, necrosis at the site of GHA injection, or decreased visual acuity have not been reported. Satisfaction with the effect of the injection was high in all patients, and no hyaluronidase was required for enzymatic breakdown of the injected drug.
Pros and cons of the surgical method
Surgical intervention differs from hardware and injection techniques in a wider range of targeted tasks, high efficiency and sustainable results. Surgery helps with severe age-related manifestations, significant congenital anomalies, when minimally invasive procedures are powerless. Unlike fillers, which dissolve in 6–18 months, the operation provides a long-lasting lifting and rejuvenation effect for 5–15 years.
Like any operation, surgical blepharoplasty can cause complications. Among the possible ones are eye infection, hematomas, swelling, hypertrophied scars. By choosing an experienced, qualified surgeon, the risk of side effects is minimized. The relatively high cost of the procedure is justified, because over 5–15 years it is necessary to undergo from 5 to 30 courses of injection plastic surgery of the upper eyelids for a similar result, which will cost more.
Photos of completed work
Upper eyelid blepharoplasty
Photos "before" and "after"
Photos "before" and "after"
Photos "before" and "after"
Photos "before" and "after"