“Aesthetic Guide” presents to your attention the second part of an article by the head of a clinic in the city of Bochum (North Rhine-Westphalia, Germany), German cosmetologist and plastic surgeon Jan Balczun, about the side effects and complications caused by dermal filler injections
V. In the first part, the author talked about the types of fillers and their characteristics, spoke in detail about mild and some moderate complications, as well as ways to combat them.
In the second part, Jan Balchun examines other moderate and severe complications, giving each a detailed description and prescribing a treatment plan.
Happy reading!
Moderate complications
Change in skin color
No matter what filler is used during the procedure, there is always a risk of skin discoloration or discoloration.
A slight redness that occurs almost immediately after the injection is a typical side effect and usually goes away within a few days - a common inflammatory reaction in the injection area. If after this period the redness does not disappear, this may lead to a hypersensitivity reaction. Its treatment should be similar to that of rosacea: with topical steroids and oral tetracycline or isotretinoin. Vitamin K applications also give good results.
Another risk in the injection area is excessive distension, caused either by the product itself or by excessively active movements of the syringe. It can lead to neovascularization, which usually resolves in 3-12 months without treatment. If neovascularization worries the patient, laser cosmetology will come to the rescue. The choice of laser depends on the size of the vascularity: the list of options includes the 532 nm KTP laser, 585 nm copper vapor diode laser, 585 nm pulsed dye lasers and IPL pulsed light therapy.
As for the relationship between hyaluronic acid fillers and the Tyndall effect, recent research suggests that the blue tint is actually due not to the effect itself, but to the reflective properties of the skin. Since there is no point in waiting for the product to dissolve in the body on its own, treatment should begin with the use of hyaluronidase. If this is not enough (which is possible if the HA crosslinks too tightly), an incision and extrusion/removal of the drug can be carried out within 12 months.
According to the National Plastic Surgery Data Bank, in 2013, 22% of all cosmetic procedures were performed on racial and ethnic minority patients. Skin of color tends to become hyperpigmented after trauma, and since dermal filler injections represent minor trauma, post-inflammatory hyperpigmentation is a common problem after contouring procedures, especially for Fitzpatrick skin types IV-VI.
If hyperpigmentation occurs after drug administration, a whitening agent (eg, topical hydroquinone) along with Retin-A and a strong daytime sunscreen should be used in the first stage of treatment. If this does not help, the next step should include IPL and laser treatments. To minimize the risk of post-inflammatory hyperpigmentation, the number of injection sites should be limited.
Malar edema
This complication can occur as a reaction to any filler that is used to fill the infraorbital cavity or nasolacrimal groove.
In a retrospective study, 12 of 51 patients (23%) who underwent infraorbital socket correction with hyaluronic acid filler had prolonged swelling for an average of 5.4 months.
As part of the dissection cadaver study, scientists were able to identify the malar septum - a fascial structure leading from the orbital ridge, above the arcus marginalis, to the skin of the cheek, approximately 3 cm below the outer corner of the eye. The malar septum divides the SOOF (suborbicularis oculi fat) into superficial and deep sections. While the lymphatic drainage of the deep compartment flows into the buccal fat, the superficial compartment, in turn, compromises this process.
This lymphatic barrier is very important and worth remembering; By introducing the drug superficially, into the malar septum, you can enlarge and inflate it, which will make it impermeable to lymphatic fluid - this, in turn, will lead to the accumulation of fluid and malar edema. Since any conservative therapy does not cope well with this problem, if it occurs, it is necessary to introduce hyaluronidase to dissolve the compromising HA.
To avoid malar edema, the injection must be carried out in the deep section, and the filler should only be based on hyaluronic acid.
Nodular neoplasms
If a patient develops nodular tumors after an injection, it is important to properly evaluate the impact that treatment has on the patient.
For example, some nodes are noticeable but not noticeable, in which case it would be better to leave everything as it is and wait and watch the dynamics. Other neoplasms may require immediate action from the doctor. Typically, these delayed-effect nodules persist for weeks or even months and can subsequently be classified as inflamed or non-inflamed.
Non-inflamed nodules with delayed effect
Non-inflamed nodules are considered one of the most common side effects of contouring procedures. They have a firm, non-draining and regular surface with no signs of erysipelas or fever. The most common cause of these nodules is product misuse or product migration.
Treatment directly depends on the injected material. When using HA fillers, the most logical solution would be hyaluronidase. With stronger substances such as calcium hydroxyapatite, another workable option is to break the product with either a sodium chloride solution or lidocaine, followed by vigorous massage.
If this does not produce the expected effect, the nodules can be treated with small amounts of intralesional steroids to prevent skin atrophy. Between procedures, the patient should be given a home massage to speed up the filler dissolution process.
If the nodules persist for several months and do not respond to treatment, they will become fibrotic and will require excision.
Inflamed nodules with delayed effect
As a rule, inflamed nodules with a delayed effect are painful, sensitive formations of a reddish hue.
The scientific literature debates whether these delayed-onset inflammatory nodules may be the result of biofilms. The latter occur if the drug is injected into the subdermal layer and becomes covered with bacteria, which, having united, form a complex and secrete a protective (as well as adhesive) matrix - this allows them to live both in the living structure and on the inner surface of the skin. This infection is very resistant to antibiotics.
Because delayed-onset inflamed nodules are difficult to distinguish from mild hypersensitivity reactions, any area of deep red skin, no matter how quickly it has paled, should be considered a biofilm.
Treatment should begin with an antibiotic, macrolide, or tetracycline, which the patient should take for at least 14 days and then re-evaluated. If improvements are noticeable after two weeks, antibiotics should be continued for another 4 weeks. If no improvement is observed, therapy should be reconsidered by prescribing double doses of the antibiotic.
If after 6 weeks there is still no improvement, subsequent treatment for the effects of HA filler and other fillers will vary. In the case of the former, therapy should be continued with hyaluronidase every four weeks until the nodules completely disappear, without also stopping taking antibiotics. Topical steroids should be chosen for the second category of fillers (they should also be used if the hyaluronic acid filler does not respond to hyaluronidase).
The most preferred is triamcinolone acetonide 40 mg/ml. The patient should also be aware of possible soft tissue atrophy (20-30%) and telangiectasia after treatment - these side effects are described in relevant articles.
The last resort for any such nodules is surgical excision.
Foreign body granulomas
This is a very rare delayed complication and occurs in only 0.1% of patients.
Most foreign body granulomas appear after injection of non-biodegradable or semi-biodegradable fillers. This reaction of the body to foreign material can occur either singularly or in a small group, usually in the form of dermal nodules. They usually appear within 6 months after injection, but there are also reports of granulomatosis with a delayed effect - more than 14 months after injection with a product containing polymethyl methacrylate.
Infection
As a procedure that disrupts the natural skin barrier, contouring may carry the risk of infection of the correction area.
To minimize it, it is important to follow general precautions, such as disinfection, use of sterile supplies and drugs themselves, and remember to wear gloves during the procedure. If the consequence of the injection is diffuse inflammation of the correction area, its common pathogen is Staphylococcus aureus (Staph. Aureus) or Strep. pyogenes - as a natural causative agent of intractable skin colonization. This infection may be misinterpreted as a hypersensitivity reaction, but it is worth remembering that erysipelas may be accompanied by fever and itching. Depending on the severity of the infection, antibiotics should be given orally or intravenously. It is not recommended to massage this area as this may spread the infection.
If the infection continues to spread, it can cause an abscess, which is a very rare complication. As with any abscess, incision and drainage should be performed in addition to antibiotics.
Herpes outbreak
If the patient has a history of herpes infection (even in the past), reactivation of the virus may be caused by the injection due to direct injury to the axon by the needle.
Manipulation of skin tissue or an inflammatory reaction after filler injection could themselves serve as alternative causes of reactivation, the scientists say, but this hypothesis requires further study. Hyaluronic acid itself has been shown to act as a protective agent by preventing viral replication.
Reactivation of the herpes infection, if it occurs, usually occurs within 24-48 hours after the injection. Localization, as a rule, becomes the injection point, most often in the nasolabial folds, as well as in the perioral area. Spread into adjacent areas is rare, but can also happen.
The treatment program depends on the severity of the outbreak. As antiviral therapy, you can use ointments or administer special blockers intravenously.
Filler injection: precautions
- To minimize unwanted results, it is recommended to start with temporary hyaluronic fillers. This will allow the doctor and patient to evaluate the cosmetic effect and decide on the need to introduce permanent filler.
- Swelling and bruising can be avoided by stopping anti-clotting medications and using ice packs.
- The depth of filler injection is essential. When using fillers in cosmetology, you need to take into account the manufacturer’s recommendations and the specialist’s own experience.
- During the first three days after the procedure, sudden, repetitive movements should be avoided so as not to provoke migration of the drug.
- Certain parts of the body and types of scars are more prone to developing unwanted effects. For example, bumps most often form around transverse wrinkles on the forehead and vertical lines near the mouth. In areas with thin skin, such as the eyelids and the eye area, injectable fillers can move easily, so injections are not performed here. Lumps and nodules can also form in the corners of the eyes, however, some fillers give excellent results here too. The risk of necrosis in the glabella area increases when using the patient's own fat. Narrow, deep and depressed scars are the result of chicken pox or acne. When correcting them, a phenomenon may occur in which the edges of the scar increase in volume along with the deepened area into which the drug is injected.
- When using fillers in cosmetology, it is sometimes necessary to conduct several tests first. For example, products based on bovine collagen must undergo a preliminary allergy test.
Severe complications
Damage to the vascular system
As one of the worst side effects of fillers, this one indicates a serious and immediate complication.
Therefore, prompt recognition of the problem and prompt and aggressive treatment to prevent serious, potentially irreversible complications is essential. Possible complications described in the literature, in addition to tissue necrosis and retinal artery occlusion (see below), are acute loss of vision and hemiplegia after autologous fat injections into facial areas as a result of ocular and cerebral embolism, as well as acute stroke that can occur after fat injection to the glabella.
Tissue necrosis
Tissue necrosis after dermal filler injection can occur in two scenarios: the first refers to damage to the vascular system by injecting too much material too close to the vessel, which leads to disruption of blood supply due to compression;
another option is to inject material directly into the vessel, resulting in direct obstruction. The first noticeable signs of damage to the vascular system are prolonged pallor, often accompanied by pain, followed by darkening of the area after some time. Always be alert if pallor persists for more than 30 minutes.
The points most susceptible to injury are areas with minimal collateral circulation such as the nose, areas with terminal blood supply such as the glabella, or large vessels such as the nasal artery.
The terminal frontal artery has small branches and is responsible for a large area of forehead skin with minimal collateral circulation. In addition, the vascular anatomy in this area is unpredictable, poor, and predominantly terminal. The majority (more than 50%) of reported cases of this complication occurred in the glabella region.
Retinal occlusion
If the force of drug injection exceeds intra-arterial pressure, the injection may move proximally to the angular artery.
With continuous movement, the injection can reach the base of the central retinal artery. If pressure on the syringe plunger is released, the material moves distally into the retinal artery. Injections in different areas can lead to different types of occlusion. When filler is injected into the glabella area, the material moves through the frontal artery towards the supraorbital artery; in the nasolabial fold, any injection into the anastomosis of the dorsal nasal artery from the ophthalmic artery can cause blindness.
Typically, the particle size of HA is 400 microns. This means that the particle is not prevented from moving within the ophthalmic artery, which is typically about 2 mm in diameter. In comparison to this relatively large vessel, the central retinal artery has a diameter of about 160 microns, which is much smaller than HA particles—meaning it can easily be blocked by filler.
Patients suffering from retinal artery occlusion report immediate blurring or loss of vision and sometimes experience pain in the eye area.
If you suspect any form of vascular damage or arterial occlusion in the patient, the injection should be stopped immediately and the next step is to apply thermo- and nitroglycerin paste to induce vasodilation, and so on until improvement is noticeable. Additionally, at least 75 U of hyaluronidase combined with 1.5 mL of 0.5% lidocaine should be injected along the underlying vessel and adjacent skin to dissolve all previously injected material and decompress the vessel. After injection of hyaluronidase, the damaged area must be intensively massaged.
For more severe cases and if there is no response, subcutaneous injection of low molecular weight heparin into the affected area may give good results.
Drug migration
The lower the degree of biodegradation of the filler, the higher the risk that it may migrate.
In particular, this was clearly proven by the results of work with polytetrafluoroethylene. Some studies with calcium hydroxyapatite have reported no migration, while others have reported active migration of CaHA filler, especially in the perioral area, causing a “popcorn lip” effect. This product migration can even occur several years after injection. Silicone, unlike other filler bases, has a unique ability to migrate to areas distant from the injection site: there is plenty of evidence of cases where silicone has managed to migrate even to other organs.
Causes of the Tyndall effect
First, let's figure out what the Tyndall effect is. In fact, it is found not only in cosmetology, but also in everyday life: it is the transmission of a beam of light through a relief texture. A striking example: the sun's rays, which are visible through the foliage.
In this article, we consider such a defect as filler showing through the skin - a phenomenon that is not as picturesque as the crown of trees, but, fortunately, you can get rid of it. How to do this - read on.
The Tyndall effect after filler occurs in the following cases:
- too thin and light skin (usually occurs in people with Celtic or Scandinavian phototypes);
- age - over the years, the skin becomes thinner, which means that the older the woman, the more likely it is that unpleasant swelling will occur;
- cosmetologist’s mistake: incorrectly calculated amount of the drug or incorrect administration technique;
- false diagnosis of the problem or lack of indications for the procedure;
- poor quality of the filler itself;
- failure to follow skin care recommendations after the procedure.
Before the procedure, an experienced cosmetologist will definitely ask:
- are you currently taking medications, especially hormones and antibiotics;
- are you allergic to any medications?
- How old are you;
- Are you sick with anything at the moment, do you have any chronic diseases?
It is also important to understand the condition of the skin and the facial contour of the patient - the selection of the filler itself and the calculation of its quantity depend on this.
After the procedure, the specialist must observe the girl’s condition for another hour and schedule a second appointment in a few days. This is a necessary measure, because darkening and swelling do not appear immediately - it all depends on the individual characteristics of the body.
Conclusion
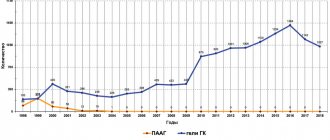
The dermal filler market has expanded significantly in recent years.
Currently, fillers can not only smooth out wrinkles, but also restore volume in many areas, thereby changing the overall condition of the face. However, to achieve decent results, the doctor must have a thorough understanding of the individual characteristics of the materials used, including indications, contraindications, as well as the prevention and treatment of any possible side effects, if they are unavoidable.
There is not a single filler that does not have side effects, but the likelihood of their occurrence is sharply reduced if the specialist is familiar with the range of both the fillers themselves and the means that stop their effects. Also, thanks to a deep knowledge of anatomy, mastery of various techniques and the ability to create an individual treatment plan for patients, almost all serious side effects can be avoided.
Source: Prime International Journal of Aesthetic and Anti-Aging Medicine
Share:
Date of publication: 11 October `17
More about the correction process
Modern cosmetology clinics can offer several variations of fillers:
- biosynthetic. Used for collagen formation and contouring;
- synthetic. They remain in place forever because they are not excreted by the body;
- biodegradable. Consist of hyaluronic acid or calcium hydroxyapatite.
The latter option is stored for a certain time, it is safe for health and is gradually eliminated. This ensures effective correction of folds, wrinkles, small defects, and unevenness. A tool is used for placement under the skin that does not cause injury. Local anesthesia is usually used because the puncture is unpleasant.