Stages of rehabilitation after abdominal surgery
In medicine, rehabilitation after abdominal surgery is divided into several periods:
- Early period: covers the time immediately after the end of the operation until the removal of the sutures, lasts on average 10 days.
- Late period: this is a period of recovery under medical supervision, lasting until the patient is discharged from the hospital hospital.
- Long-term period: this is the time required to fully restore performance and return to normal life.
Depending on the type of operation, doctors may also prescribe different modes of physical activity during rehabilitation after abdominal surgery. The regime can be strict bed, bed, ward and free.
Bloating and gas formation: modern treatment options
Bloating is a very common and very unpleasant symptom that makes a person suffer even more than from abdominal pain. Bloating is a gas-related symptom. The sensation of excess gas in the gastrointestinal tract (GIT) is most often associated with increased tension in the wall of the hollow organ and can be a consequence of both actual excess formation (and/or impaired removal of gases from the GIT) and the result of high visceral sensitivity.
The subjective feeling of bloating (part of the symptom complex of flatulence syndrome) is usually accompanied by painful objective manifestations: an increase in abdominal circumference, loud rumbling (borborygms), sudden release of gases through the mouth (belching), accompanied by specific sound manifestations, uncontrolled release of foul-smelling gases (flatulence). All these symptoms cause psychological discomfort, feelings of shame and guilt, and negatively affect mental status, leading to restlessness, anxiety, depression, and phobic moods. If bloating and associated problems become persistent, a person’s normal lifestyle, family and social relationships are disrupted, the quality of life decreases, and the range of social and behavioral activity is narrowed. As a rule, gas-associated symptoms worsen during periods of psycho-emotional stress, with changes in climatic and time zones, and changes in nutritional patterns.
The symptom of bloating has no age limit [1] and is one of the most common, observed in more than 85% of gastroenterological patients [2]. Among patients with a functional gastrointestinal disorder (FGID), abdominal bloating is observed in approximately 24–97% of patients and, in addition, very often occurs in patients with gastroesophageal reflux disease (GERD), diseases of the pancreas and gallbladder, premenstrual syndrome, and impaired intestinal motility . Patients suffering from irritable bowel syndrome (IBS) with bloating are more likely to visit the doctor, and the impact of their disease on quality of life is more pronounced than the impact of IBS without bloating [3].
Abdominal bloating occasionally occurs in almost all people and, as a rule, is clearly related to dietary habits, i.e., consumption of foods with a high gas-forming potential. Thus, according to the results of a population study conducted in our country among a practically healthy contingent of respondents, it was found that over the last week signs of flatulence were noted by 28%, over the last month - 44%, over the last year - 62% of respondents [4].
The prevalence of functional bloating in adults in the United States ranges from 6% to 31%, with an average pooled prevalence estimate of 15.9%, and is more common in women (19.2%) than in men (10.5%) [5].
The high variability in the prevalence of bloating is associated, firstly, with different perceptions of the term. Patients and doctors interpret the content of this concept differently (as a variant of a subjective feeling of fullness and bloating of the abdomen; the appearance of hardness and tension in the anterior abdominal wall; excessive formation and discharge of gases; and as an objective increase in abdominal girth, and, finally, as a manifestation of any other dyspeptic complaints). Secondly, some patients suffering from bloating do not seek medical help for a long time, in particular, because of the moral and ethical complexes that accompany the excessive formation of gases in the intestines; on the contrary, other people ignore these symptoms, believing they are of little significance for overall health. All this not only complicates the epidemiological assessment of the syndrome, but also does not allow us to formulate diagnostic criteria convenient for clinical practice and objective assessment of the effectiveness of drug therapy.
In the new edition of the Rome IV criteria, functional abdominal bloating/distension still forms part of a large group of functional gastrointestinal disorders of the gastrointestinal tract-central nervous system interaction (Table 1) and is considered as a diagnosis per se in patients who do not meet the Rome criteria within the framework of other gastrointestinal tract disorders, although the possibility of mild abdominal pain and/or minimal bowel movements is acceptable.
Experts of the Rome IV criteria propose to combine functional abdominal bloating and distension into one concept, although they emphasize that these symptoms can be observed in isolation, do not correlate with each other and have different pathophysiological mechanisms of development [6].
Functional bloating differs from other cases of abdominal distension in its circadian rhythm: in typical cases it increases after meals (usually after eating certain so-called problem foods) and during the day and decreases or disappears at night. Problematic foods include sugars, more specifically oligo- and polysaccharides, which pass unchanged into the large intestine, where they are fermented by fermenting and proteolytic microorganisms. This process is accompanied by the release of gas. Excessive perception of intestinal gases forms the symptoms of the disease [7].
Key points in the conceptual understanding of the pathogenesis of functional abdominal bloating/distension include visceral hypersensitivity, gas formation in the colon, and changes in gastrointestinal motility. The mechanisms associated with visceral hypersensitivity are fueled by alert anticipation of perceived unpleasant events. In the dysregulation of the brain-gut axis, genetic predisposition, environmental factors, chronic stress, and disorders of the intestinal microflora play a role [8].
Currently, the main causes of functional bloating are considered: visceral hypersensitivity, colonic fermentation, excessive bacterial growth in the small intestine and changes in the metabolic potential of the colon microbiota, disruption of intestinal transit and rectal gas evacuation [9].
The study of the pathophysiological mechanisms of development of the symptom of functional abdominal distension, thanks to innovations in diagnostics, including abdominal induction plethysmography (which makes it possible to measure abdominal distension), allows us to consider an abnormal viscerosomatic reflex involving the diaphragm and muscles of the anterior abdominal wall as the main predictor of the formation of this symptom. The mechanism of this reflex is not yet known. Studies have shown that colonic fermentation, decreased rectal sensation, and impaired intestinal transit may contribute to abdominal distension in some patients [9, 10].
The diagnosis of functional swelling must be established with indispensable reliance on 3 key positions: 1) anamnesis and clinical picture; 2) a thorough physical examination; 3) exclusion of anxiety symptoms with the minimum required set of laboratory and instrumental tests [11].
Despite the significant prevalence of functional bloating/distension of the abdomen, there are no clearly developed treatment algorithms for this pathology. The list of methods for effective treatment of bloating and distension is very limited (Table 2).
Some dietary changes, such as avoiding carbonated drinks and foods that tend to cause gas, can help reduce the symptoms associated with bloating. The exclusion from the diet of poorly digestible and assimilated short-chain carbohydrates (fermentable carbohydrates; oligo-, di- and monosaccharides; polyols) also has a positive effect, that is, bloating decreases when following a diet that excludes the entry into the colon of intensively fermentable substrates, such as wheat products; fruits rich in fructose (for example, apples, pears); vegetables containing fructans (onions, asparagus, etc.); products containing raffinose (for example, legumes, beets), sorbitol (sugar-free chewing gum) [3].
Helps prevent bloating caused by eating problematic foods by taking alpha-galactosidase (Orlix, dietary supplement) with meals. Alpha-galactosidase provides enzymatic activity missing in the human body, breaking down oligosaccharides into simpler, easily digestible forms. As a result of the use of Orlix, the amount of fermentable substrates entering the colon is reduced and the overproduction of gas associated with nutrition is prevented [12, 13].
In addition, some improvement can be expected from moderate physical activity, which facilitates bowel movements and gas transport.
Reduces the severity of bloating and abdominal distension by taking prokinetics. Prokinetics, accelerating intestinal transit, promote the movement of gas through the intestine and its removal to the outside [14]. However, prokinetics (lubiprostone and linaclotide), recommended by experts of the Rome IV criteria, for the treatment of bloating are not registered in our country. Among the drugs available on the Russian pharmaceutical market, trimebutine (Trimedat) is a universal regulator of gastrointestinal motility. Trimebutine is an opiate receptor agonist, its modulating effect on gastrointestinal motility and analgesic effect are associated with a nonspecific effect on all classes of peripheral opiate receptors: μ, κ and δ. Trimebutine stimulates the evacuation function of the stomach, normalizes intestinal motility and gas transit, reduces visceral sensitivity, helps relieve the feeling of bloating and discomfort, and has a beneficial effect in both hypokinetic and hyperkinetic forms of disorders of motor activity of the gastrointestinal tract. In the treatment of flatulence, a course prescription of the drug Trimedat 200 mg three times a day 30 minutes before meals for 30 days or more is indicated [15].
Currently, the study of the role of disturbances in the intestinal bacterial flora in the occurrence of gastrointestinal tract is ongoing. Thus, it was found that there are some species differences in the microbiome of healthy people and patients with bloating. This has prompted numerous clinical studies to study the effectiveness of antibiotics, probiotics and prebiotics for flatulence. Two probiotics have been shown to reduce visceral sensitivity in animal models: Bifidobacterium infantis and Lactobacterium acidophilus.
In the treatment of disorders associated with high levels of gas in the gastrointestinal tract, antiflatulents, or defoamers, are traditionally used. A drug that reduces foaming in the intestinal lumen is simethicone, which is a high-molecular silicon-based polymer - dimethylsiloxane with the addition of silicon dioxide. According to its mechanism of action, simethicone is a surfactant that reduces the surface tension of gas bubbles in chyme and mucus in the intestinal lumen, leading to their rupture. In this case, a process of coalescence occurs - the fusion of gas bubbles and the destruction of foam, as a result of which free gas is able to be absorbed through the intestinal mucosa or evacuated along with the intestinal contents. The dose is selected individually depending on the severity of symptoms. The main use of defoamers in clinical practice is the symptomatic treatment of various gastrointestinal diseases accompanied by excessive gas formation [2].
It is known that antidepressants modulate visceral sensitivity, they are often recommended for patients with gastrointestinal tract, but to date, based on the results of clinical studies, impressions of their effectiveness have not been definitively determined [3].
As a result, we have to admit that bloating and distension of the abdomen are difficult to treat. As soon as the connection of these symptoms with organic diseases is excluded, it is reasonable to place emphasis on the functional nature of these conditions, and in treatment it is advisable to pay attention primarily to the implementation of a diet and taking the biologically active food supplement Orlix.
The active component of Orlix is a natural enzyme - alpha-galactosidase (producer - the bacterium Aspergillus niger). 1 tablet contains 5 mg (corresponds to 150 units) of alpha-galactosidase. Does not contain GMOs, lactose, milk proteins, dyes, flavors and preservatives.
In order to study the effectiveness and tolerability of Orlix in patients with functional bloating/distension of the abdomen, an open, non-randomized, placebo-uncontrolled, multicenter study was conducted in Moscow city clinics.
Objectives of the clinical trial:
- To study the possibility of correction of gas-associated symptoms after ingestion of problematic foods in patients with functional bloating/distension of the abdomen when consuming Orlix with meals.
- Assessment of the tolerability of Orlix and its impact on quality of life.
Problematic foods:
- all types of beans (white, red, brown and their variants);
- lentils - all types;
- all types of cabbage (white, red);
- kohlrabi and Brussels sprouts;
- cauliflower and broccoli;
- salads of all kinds;
- onion garlic;
- carrots, parsley;
- flour and flour products (especially from wholemeal flour);
- pistachios and sesame;
- soybeans and soy products (soy milk, tofu).
Study design
The study involved 55 patients with complaints of flatulence (bloating, belching, increased passage of gas, a feeling of fullness in the abdomen, increased abdominal circumference) associated exclusively with the consumption of problematic foods, after excluding all other possible causes of gas-associated symptoms. Patients were examined according to a unified plan (general clinical analysis of blood, urine, stool, biochemical blood test, esogastroduodenoscopy, colonofibroscopy, ultrasound examination of the abdominal organs). At the end of the study, all patients underwent a repeat examination of general clinical and biochemical blood tests.
The average duration of complaints in patients included in the study was 3.5 years. The male to female ratio is 20:35. Average age 38 ± 5.5 years.
A prerequisite for patient inclusion in the study was the refusal to use any antiflatulent drugs and the continuation of taking problematic (gas-forming) products in the usual volume.
All patients included in the study took the dietary supplement Orlix with the first portion of problem food in a dose of 2–4 tablets for 2 months.
The effectiveness of Orlix was assessed based on the patient’s subjective assessment of the manifestations of flatulence at the beginning of the study, and then during the 1st and 2nd control studies (after one and two months of treatment, respectively) according to the severity of symptoms: 1st degree - all gases associated symptoms are completely eliminated, 2nd degree - mild symptoms of flatulence that do not bother the patient in everyday life, 3rd degree - improvement is observed, but in a mild form gas-associated symptoms persist, 4th degree - very little or no improvement.
As part of the overall assessment of the effectiveness of Orlix after 2 months of its use, based on a subjective assessment of the severity of symptoms of flatulence, patients were divided into 4 groups: 1st group - excellent - improvement of symptoms by 100% (corresponding to the assessment of the 1st degree), Group 2 - very good - improvement of symptoms by 50-80% (corresponding to a grade 2 assessment), Group 3 - moderate - improvement of symptoms by 30-50% (corresponding to a grade 3 assessment), 4th group - no changes - 0–30% (corresponds to a grade 4 assessment). All study statistics are based on patients' subjective assessment of gas-related symptoms after consuming problematic foods.
The effectiveness and safety of Orlix was also analyzed based on data from the SF-36 questionnaire to assess quality of life.
A study of anthropometric parameters (body weight and abdominal circumference) was carried out before the start of treatment and upon its completion.
Research results
Subjectively, already at the first control examination, 28 (50.9%) patients noted a complete elimination of the development of symptoms of flatulence after eating problematic foods while taking Orlix with meals; after 2 months of treatment, the number of patients with excellent effectiveness of Orlix increased to 32 (58.2 %).
Mild symptoms of flatulence persisted and did not bother the patient in everyday life in 19 (34.6%) patients at the end of the first month of treatment; subsequently, two of them noted the almost complete disappearance of gas-associated symptoms (with an increase in the single dose of Orlix to 3 tablets).
It is noteworthy that the number of patients who reported that, despite taking Orlix, they still had mild gas-associated symptoms, did not depend on the duration of treatment: 6 (10.9%) people at the 1st control and 5 ( 9.1%) at the end of observation. In one patient from this group, complete relief of abdominal bloating occurred when the single dose of Orlix was increased to 3 tablets.
Only 2 (3.6%) patients noted no improvement during the first month of treatment. One patient had the Orlix dose increased to 3 tablets per dose when consuming problematic foods, and against this background he noted a significant improvement. In another patient, increasing the dose of Orlix to 4 tablets per dose resulted in only minor relief of symptoms.
Thus, subjective improvement, despite continuing to take the usual amounts of problem foods, when using Orlix with meals was detected in 98.2% of patients (Table 3), and all of them noted the rapid onset of action of the biologically active food supplement when following the regimen taking Orlix with the first portions of food.
The overall assessment of the effect of Orlix after 2 months of its use, based on the patient’s subjective assessment of the severity of symptoms of flatulence, is presented in table. 4. An excellent effect was registered in 32 (58.2%) patients, a very good effect in 17 (30.9%), moderate improvement in symptoms was noted by 5 (9.1%) people. Only one patient in the study reported very little improvement in flatulence symptoms.
At the same time, not only subjective improvement was noted in patients; when studying the dynamics of anthropometric parameters, a tendency to a decrease in abdominal circumference was revealed, which was more pronounced in women while maintaining a constant body weight (Table 5).
When analyzing changes in the quality of life according to the nosologically nonspecific questionnaire SF-36 during treatment with Orlix, positive dynamics were also revealed: there was a significant improvement in the quality of life in almost all indicators of both physical and mental functioning. The mean physical functioning (PF) score increased from 85.1 ± 6.4 to 92.2 ± 2.1 points (p < 0.05); role physical functioning (RP) - from 51.3 ± 5.1 to 85.2 ± 2.3 points (p < 0.05); the general health (GH) score increased from 48.9 ± 8.4 to 61.21 ± 2.1 points (p < 0.05). Indicators of the psychological component of health changed as follows: vitality (VT): 54.6 ± 6.3 and 78.2 ± 4.9 points (p < 0.05); social functioning (SF) - 47.6 ± 11.2 and 68.8 ± 5.3 points (p < 0.05); role emotional functioning (RE) - 58.8 ± 8.4 and 70.2 ± 3.1 points (p < 0.05).
As part of the subjective assessment, the dosage of Orlix was statistically evaluated. At the beginning of the clinical study, a dosage of 2 tablets was prescribed to 32 (58.2%) patients, 3 tablets to 23 (41.8%) patients, a dosage of 4 tablets was not prescribed. During the first control, in 6 patients with the 3rd degree of severity of gas-associated symptoms, the dosage of Orlix was increased to 3 tablets and in 1 patient who did not notice an improvement in symptoms, the dose of the drug was increased to 4 tablets. However, increasing the dosage did not significantly affect the subjective feeling of the severity of flatulence symptoms. Thus, it was found that the dosage of Orlix is less correlated with the severity of gas-associated symptoms, and more dependent on the amount of food eaten; usually it is enough to take 2-3 tablets during a normal lunch (Table 6).
The dynamics of the main parameters of general clinical and biochemical blood tests (ALT, bilirubin, glucose) in the direction of deterioration were not observed (Table 7).
All patients noted good tolerability while taking Orlix; no adverse reactions were recorded.
Discussion
The study included patients with functional bloating/distension. All of them noted the connection between the occurrence of gas-associated symptoms and the consumption of problematic foods, such as beans, lentils, all types of cabbage, as well as kohlrabi, broccoli, salads of all types, onions, garlic, carrots, parsley, whole wheat flour products, pistachios and sesame seeds, soybeans and soy products. These products are united by a high content of oligosaccharides (melibiose, raffinose, stachyose, verbascose), formed by galactose and fructose, in various ratios (Table 8), since soy contains a lot of them, they are also called “soy oligosaccharides”.
Galactose (from the Greek root γaλακτ-, “milk”) is one of the simple sugars, a monosaccharide from the hexose group. D-galactose is widespread in nature, it is part of oligosaccharides (melibiose, raffinose, stachyose), some glycosides, plant and bacterial polysaccharides (gums, mucus, galactans, pectins, hemicelluloses), in animals and humans - in the composition of lactose, group-specific polysaccharides, cerebrosides, keratosulfate, etc. Fructose (fruit sugar), C6H12O6 - monosaccharide, isomer of glucose. In its free form, fructose is present in almost all sweet fruits, and also makes up up to 80% of honey; as a monosaccharide unit it is part of sucrose and lactulose.
Soy oligosaccharides are widely used in the food industry (soft drinks, candies, cakes, industrially prepared wheat products, dairy products, infant milk powder, etc.), and are included in many pharmaceuticals.
But human digestive enzymes are not able to break down the chemical bond between two galactose molecules, so these oligosucroses are not absorbed in the small intestine, but are hydrolyzed by enzymes of colon microbes (which have a set of enzymes that utilize soy sugars) with the formation of organic acids and large amounts of gases: H2, CH4 , CO2 (hence the name of products containing such oligosaccharides - gas-forming, or problematic).
As a result of research, it was possible to isolate a unique bacterial enzyme - α-galactosidase, which hydrolyzes galactosidase compounds, breaking down oligosaccharides into simple carbohydrates without the formation of gases. Such enzymes are found in the bacteria Bacteroides fragilis, Bacteroides thetaiotaomicron and Streptomyces avermitilis.
Alpha-galactosidases (syn. melibiases) have “exoactivity”, i.e. they cleave off the terminal non-reducing residues of alpha-D-galactose from the oligosaccharide molecule, hydrolyzing complex sugars to monosaccharides: glucose and galactose, which are absorbed by the cells of the intestinal mucosa and are used in body as a source of energy.
The use of the enzyme alpha-galactosidase in nutrition provides enzymatic activity absent in the human body, limiting the entry of oligosaccharides into the large intestine in an undigested form, where they undergo anaerobic bacterial hydrolysis with the formation of gases.
When adding this enzyme in the form of a dietary supplement to Orlix food, we found its effect in a group of 55 people to be excellent in 58.2%, and very good in 30.9%. Thus, patient-reported improvement after taking Orlix occurred in the vast majority of patients (89.1%).
When analyzing changes in quality of life according to the SF-36 questionnaire during monotherapy with Orlix, a significant improvement in quality of life was revealed in terms of both physical and psychological functioning.
All patients while taking Orlix noted that it was well tolerated.
Conclusion
In patients with functional bloating, taking the dietary supplement Orlix (active substance alpha-galactosidase) provides high effectiveness in relieving gas-associated symptoms and improves quality of life. Recommended dosage of Orlix: 2-3 tablets with meals with the first portions of food when consuming gas-forming foods. It is important to note that the onset of action of Orlix is immediate; flatulence does not occur when eating problematic foods. The dosage depends on the volume of problem foods eaten; 2-3 tablets are usually sufficient for average amounts of food. In the future, the patient can determine the optimal dose for himself.
Orlix is safe to use and can be recommended for healthy people who consume gas-producing products.
Reducing gas production in the intestines may represent an effective therapeutic strategy to prevent the development and/or exacerbation of gas-related symptoms in any gastrointestinal disease (functional or organic) when their cause is at least in part due to hyperproduction of gas.
Literature
- Belmer S.V., Gasilina T.V., Khavkin A.I. et al. Functional disorders of the digestive organs in children. M.: RGMU, 2005. 36 p.
- Butorova L.I., Kolomoets A.N., Tarasova E.S. Excessive gas formation syndrome in the intestines: clinical significance and principles of therapy // Difficult Patient. 2005.
- Functional disorders of the gastrointestinal tract. A practical approach based on clinical experience / Ed. B. E. Lacey, M. D. Crowell, D. C. DiBaiza. Per. from English edited by S. V. Demicheva. M.: GEOTAR-Media, 2022. 352 p.
- Flatulence syndrome in therapeutic practice: optimization of treatment approaches: educational manual / Ed. Yu. P. Uspensky. St. Petersburg: InformMed, 2010. 63 p.
- Sandler RS, Stewart WF, Liberman JN, Ricci JA, Zorich NL Abdominal pain, bloating, and diarrhea in the United States: prevalence and impact // Dig DisSci. 2000; 45:1166–1171.
- Drossman DA Functional gastrointestinal disorders: history, pathophysiology, clinical features and Rome IV // Gastroenterology. 2016; 150: 1262–1279.
- Agrawal A., Houghton LA, Lea R. et al. Bloating and distension in irritable bowel syndrome: The role of visceral sensation // Gastroenterology. 2008. Vol. 134. P. 1882–1889.
- Camilleri M., Lasch K., Zhou W. Irritable bowel syndrome: Methods, mechanisms, and pathophysiology. The confluence of increased permeability, inflammation, and pain in irritable bowel syndrome // Am J Physiol. Gastrointest. Liver Physiol. 2012, 303: 775–785.
- Lewis MJ, Reilly B, Houghton LA et al. Ambulatory abdominal inductance plethysmography: towards objective assessment of abdominal distension in irritable bowel syndrome // Gut. 2001; 48: 216–220.
- Houghton LA, Lea R, Agrawal A et al. Relationship of abdominal bloating to distention in irritable bowel syndrome and effect of bowel habit // Gastroenterology. 2006; 131:1003–1010.
- Pimanov S.I., Silivonchik N.N. Rome IV recommendations for the diagnosis and treatment of functional gastroenterological disorders. A manual for doctors. M., 2016. 160 p.
- Orlix®. Instructions for use.
- Expert opinion of the Federal Budgetary Institution of Health and Safety of Rospotrebnadzor No. 10–2 FC/2098 dated May 28, 2015.
- Cadarella M., Serra J., Azpinoz F. et al. Prokinetic effect in patients with intestinal gas retention // Gastroenterology. 2002. Vol. 122. P. 1748–1755.
- Ivashkin V. T., Poluektova E. A., Reykhat D. V. et al. Efficacy of the most commonly prescribed groups of drugs in patients with functional disorders of the gastrointestinal tract - functional dyspepsia syndrome and irritable bowel syndrome (Results of an observational study) // Ross. Journal of gastroenterology, hepatology, coloproctology. 2016; 26 (4): 15–23.
- Posserud I., Stotser PO, Bjornsson ES et al. Small intestinal bacterial overgrowth in patients with IBS // Gut. 2007. Vol. 56. P. 802–808.
L. I. Butorova*, 1, Candidate of Medical Sciences N. G. Kadnikova** M. A. Osadchuk*, Doctor of Medical Sciences, Professor T. E. Plavnik*** G. M. Tokmulina*, Candidate of Medical Sciences
* Federal State Autonomous Educational Institution of Higher Education First Moscow State Medical University named after. I. M. Sechenova Ministry of Health of the Russian Federation, Moscow ** TsKBVL FMBA “Goluboe”, Goluboe *** State Budgetary Institution of Public Health No. 195 DZM, Moscow
1 Contact information
Bloating and gas formation: modern treatment options / L. I. Butorova, N. G. Kadnikova, M. A. Osadchuk, T. E. Plavnik, G. M. Tokmulina
For citation: Attending physician No. 2/2018; Page numbers in the issue: 61-66 Tags: excess gas formation, enzymatic preparation
General recommendations for rehabilitation
The early period of rehabilitation after abdominal surgery takes place in a hospital-hotel under the supervision of a medical doctor. During the first few hours, the residual effect of anesthesia appears in the body, to which is added emotional stress and pain in the area of the surgical wound. In addition, the patient exhibits symptoms of hypokinesia: the respiratory organs work with impaired function. To make all these unpleasant symptoms disappear faster, doctors recommend the following:
- After abdominal surgery, the position in bed should be slightly elevated. Be sure to observe strict bed rest until your doctor allows you to break it.
- However, even with strict bed rest, everything should be done to avoid bedsores. For this, moderate regular movements, massage of the chest and limbs are recommended.
- It is imperative to monitor the hygienic condition of the surgical suture, as well as monitor the slightest negative changes in both pain and general condition.
- The nutrition process after abdominal surgery should be carried out only according to the scheme indicated by the doctor.
In the first few days after surgery, it is necessary to monitor the results of blood and urine tests and measure the temperature. If there is even the slightest sign of intoxication (fever, thought disorder, lack of coordination), then the patient requires urgent medical attention.
Suture healing after abdominal surgery
Rehabilitation after abdominal surgery is largely related to how quickly and well the postoperative suture heals. The speed of healing is influenced by the following factors:
- patient's age;
- immune status;
- body mass;
- blood supply to tissues that were damaged during surgery.
It is also important during the entire healing process of the postoperative wound to ensure that it is not infected.
For example: after surgery to remove the appendix, the suture heals for at least a week. And if an extensive laparotomy operation was performed, then healing will take at least 2 weeks. Wounds heal fastest after laparoscopic surgery.
Recommendations for rehabilitation at home:
- The post-operative wound will be covered with a bandage for the first weeks, and the wound will also be treated by a nurse with special products to speed up healing. This dressing should not get wet, so when going into the shower (bath is not recommended), you should use a waterproof patch.
- It is necessary to regularly do moderate physical exercise: this increases blood supply to the suture area, and thus speeds up healing. But high physical activity is strictly prohibited.
- If the bandage on the seam becomes dirty or torn, it must be replaced as quickly as possible (this can only be done by a nurse).
Pneumococcal infection: symptoms, prevention
Leptospirosis: symptoms and vaccination
Vaccination to prevent pneumococcal infection
Tetanus: why vaccination is needed
Vaccination against tick-borne encephalitis in Yeysk
Vaccination in Yeysk: Anti-Rhesus immunoglobulin against Rh-conflict
Vaccination in Yeysk: vaccination against hepatitis C
Flu 2022: symptoms, type, prevention
Vaccine against drugs invented
11 myths about vaccinations
Why is it necessary to treat a postoperative hernia?
The very appearance of a hernia indicates that the organs have changed their location, and their normal mutual pressure on each other has been disrupted. This leads to disruption of the functions of all organs involved in the formation of a hernia.
Postoperative hernia is often accompanied by chronic constipation. Constipation, in turn, leads to general intoxication of the body and can affect the condition of the entire gastrointestinal tract.
Lack of treatment will eventually lead to serious complications
- coprostasis - stagnation of feces in the large intestine,
- inflammation of the hernia - inflammation of the organs located in the hernial sac,
- strangulated hernia - sudden compression of the hernial contents in the hernial orifice, leading to disruption of the blood supply to the organs in the hernial sac, and as a result - necrosis (death) of tissue. Strangulation of a postoperative hernia quite often (in 8.8% of cases) leads to death.
If a protrusion appears in the area of a postoperative scar, you should immediately consult a doctor, since it is much easier to treat a fresh hernia than one that has existed for a long time.
Over time, the hernia increases in size, the tissue surrounding it becomes thinner, so the operation becomes more complex, with a worse prognosis.
Recovery time
How long it will take the body to recover after abdominal surgery depends on the extent of the surgical intervention, the patient’s age, physique, emotional state and the presence of concomitant diseases. On average, the suture heals within one and a half months.
Abdominal surgery is a complex process, after which patients face problems with the appearance of scars and a sagging abdomen. Following the recommendations of your doctor, proper nutrition, physical activity and cosmetics will help restore your previous shape without harm to your health.
What is the most effective method for removing a postoperative hernia?
Our surgeons are fluent in endoscopic technology, but this technique is not always applicable for complex hernias. Often, much better results can be achieved by open hernioplasty.
Based on many years of experience in hernia repair, our surgeon will choose the optimal access method based on the characteristics of your particular disease.
The main factor in the successful outcome of hernia surgery is its impeccable technical execution. Poor surgical technique can ruin any method, even the best one. If all stages of the operation are performed correctly, then with any type of access the probability of hernia recurrence is minimal.
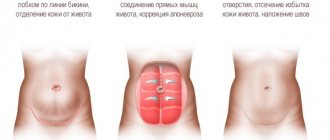
Indications for abdominoplasty
Abdominoplasty is most often used in two cases:
- excess skin on the abdomen (or fatty “apron”) appeared after radical weight loss (10 or more kilograms);
- It is necessary to remove fat from the abdomen after childbirth or cesarean section.
In addition to aesthetic discomfort and psychological self-doubt, a sagging belly can lead to unpleasant health consequences. Excessive tissue mass contributes to the curvature of the spine, causes congestion in the vessels of the lower extremities and the risk of developing varicose veins.
Why to get the best results from abdominoplasty in St. Petersburg, the N. I. Pirogov Clinic?
- The Pirogov Clinic was recognized as the best plastic surgery clinic
according to the national rating of private clinics in St. Petersburg by the medical portal “Doctor Peter” and the city portal “Fontanka.ru” in 2022; - qualified plastic surgeons with extensive experience in aesthetic surgeries;
- our doctors constantly exchange experience with foreign specialists, attract colleagues from Israel, which allows us to perform plastic surgeries using progressive world techniques;
- the opportunity to undergo all preoperative examinations in the clinic within one day;
- own laboratory: test results - quickly and with a guarantee of reliability;
- equipping operating rooms with the most advanced medical equipment from leading Western companies;
- attentive and responsible medical staff: a team of anesthesiologists, resuscitators, assistants and nurses coordinately and quickly resolves any issues around the clock;
- affordable prices for abdominoplasty, promotions;
- free consultations with plastic surgeons;
- use of the latest generation of anesthesia that does not cause any discomfort after the intervention;
- modern comfortable hospital: you feel like you are in a European hotel room;
- quick return to normal life: as a rule, patients are discharged the very next day after the intervention;
- the departments of medical cosmetology and laser dermatology carry out procedures for the fastest possible tissue regeneration, allowing you to start enjoying the results as soon as possible;
- interest-free installment payment for any operations, credit;
- online consultations with plastic surgeons.
- Sign up for a consultation - take the first step towards your new figure!
Make an appointment
Survey
Detecting a hernia is usually not difficult. Most often, a visual inspection and palpation of the protrusion is enough. If necessary, an ultrasound examination is performed.
However, when preparing for surgical treatment, it is necessary to conduct a full examination in order to identify and timely correct concomitant diseases that may become risk factors for hernia recurrence. And also evaluate the function of the respiratory and cardiovascular systems in order to choose the most suitable method of operation for each patient.
If difficulties arise in diagnosis - in case of complex multi-chamber hernias, when it is necessary to determine the topography of the hernia defect, measure the hernial orifice for individual selection of a mesh implant - an MRI of the abdominal organs is performed.
Abdominoplasty result
During abdominoplasty surgery, excessively stretched skin along with fatty tissue is removed. Removing the skin-fat flap allows you to achieve a completely flat stomach and elegant waist. If there are stretch marks in the area of the tissue being removed, then the intervention allows you to get rid of them, enhancing the aesthetic effect of the operation. After abdominoplasty, the abdomen acquires a smooth, neat appearance, but do not forget that the ideal shape must be maintained by controlling your own weight, a balanced diet and physical activity. Healthy skin condition will be supported by wraps in our Cosmetology department.
Preoperative preparation
Necessary for patients with large and giant postoperative hernias, as well as in the presence of diseases that predispose to the occurrence of hernias. Preparation should include not only drug correction of concomitant diseases, but also preparation of the skin in the area of surgery (treatment of ligature fistulas, diaper rash, maceration); bowel preparation (constipation treatment); prevention of respiratory and cardiovascular complications, prevention of intra-abdominal hypertension syndrome. Most of the preparatory activities are carried out on an outpatient basis under the supervision of a therapist (cardiologist) and a surgeon.