Huggies Elite Soft diapers 8-14 kg (size 4) 66 pcs
1099 ₽ More details
Huggies Diapers Elite Soft 5-9 kg (size 3) 80 pcs
1099 ₽ More details
Engine
A mastectomy is the surgical removal of the breast. The name of the manipulation is derived from Lat. “mastòs” and “ek tome” – “breast” + “removing”. Depending on the degree of pathology, mastectomy can be partial, radical, or performed for preventive purposes. Some types of intervention are named after the inventor of the method. If the process of metastasis affects other tissues, then the lymph nodes, pectoral muscles and subcutaneous fat are excised together with the mammary gland. Mastectomy for breast cancer is often used as the only correct and effective method of treatment.
Indications
Removal of the mammary gland is recommended in 97% of cases for females; men are much less likely to be affected by breast cancer. Indications for prescribing a mastectomy are the following diseases:
- Oncological degeneration of breast tissue.
- Sarcoma of the gland.
- Phlegmonous or gangrenous mastitis.
- Multiple nodes in the chest.
- Mastopathy of fibrocystic type.
In these cases, a competently performed operation saves a woman’s life. In men, mastectomy is performed for gynecomastia. The peak incidence occurs at 50–65 years of age, but older patients also suffer from breast cancer - the disease can strike at 75 and 87 years of age. The older the woman, the more difficult the operation and rehabilitation period are. Similar interventions are performed on female animals; this type of invasion is called unilateral mastectomy.
What causes breast cancer?
- Heredity.
- Hormones.
- Microtrauma of the gland.
- Degeneration of fibroadenoma - a benign tumor.
- Degeneration of cysts. And they appear when the mammary gland does not fulfill its purpose: a woman does not give birth and does not feed children every year.
- Impaired milk flow when feeding a baby.
There are many factors that play a role in the development of cancer; it is impossible to single out just one to try to avoid it. There is no prevention that would 100% protect a woman from this disease. Therefore, the only way to protect yourself is to get checked regularly. Once a year, go to a mammologist, have a mammogram, and for women under 35 years old, have an ultrasound of the breast.
Preparing for surgery
Removal of the mammary glands is preceded by a lot of tests and the use of hardware methods, on the basis of which the doctor concludes that there is a pathology that requires surgery:
- Blood and urine analysis.
- Mammography.
- MRI of the affected area.
- Taking a biopsy sample.
- ECG.
- Fluorography.
A thorough examination and detailed questioning of the patient by the treating mammologist is required. The health care provider should be informed about allergies to any drug or anesthetic, about taking any medications, including herbal remedies, vitamins and dietary supplements, the presence of chronic diseases and previous illnesses.
Two weeks before surgery, it is necessary to treat any inflammation occupying the body with antibiotics, and stop taking medications that affect blood density.
Immediately 12 hours before the mastectomy you should not eat, 2 hours before the mastectomy it is not recommended to drink, and the day before you must have a cleansing enema. You should also consider who will pick up the patient from the hospital and care for her during the postoperative period.
Types of surgery
Previously, surgery to remove the breast was carried out in the only way - the gland tissue was radically excised together with all adjacent components. Now it is not necessary to use the total invasion method according to Halstead-Meyer - more gentle types of interventions have been developed:
- Partial mastectomy.
- Modified radical interventions.
- Preventive surgery.
The choice of invasive penetration depends on many factors: the stage of the disease, the degree of its development, age, hormonal status. The general condition of the patient’s body and the timing of menopause (for older patients) are taken into account.
Partial mastectomy
This type is used in women with stages 1 and 2 of breast cancer, purulent mastitis and mastopathy with changes in fibrous tissue and the formation of multiple cysts. The essence of sectoral intervention is to remove the area of tissue affected by the disease without affecting the adjacent ones. There are three types of mastectomy of this type:
- Lumpectomy. The tumor and a small percentage of tissue are removed.
- Segmentectomy. A larger fragment of the breast is excised.
- Quadrantectomy. A quarter of the breast gland will be removed.
For breast cancer, after any type of regional excision, radiation therapy is prescribed. Its goal is to kill the remaining pathological cells. But relapses still happen - in such cases, the mammologist decides on radical removal of the mammary gland.
Halstead radical mastectomy
This type involves complete removal of the mammary gland, excision of all types of pectoral and axillary muscles, and fatty tissue under the scapula. Radical Halstead surgery involves cutting out the lymph nodes, nipple and skin layer. The method is used for aggressive forms of breast cancer if sectoral resection does not produce results; it is also used for active metastasis and muscle damage, as part of palliative therapy. This method is used infrequently, strictly according to indications, since total excision sometimes leads to serious complications, in particular, impaired movement of the shoulder joint.
Prophylactic mastectomy
Preventive surgery is performed less frequently - the need for it arises in case of hereditary genetic failure (BRCA mutations). This method has been used more than once by famous people, for example, a preventive bilateral mastectomy with one-stage plastic surgery was performed on Angelina Jolie. The volume of surgical invasion varies - it is carried out with the removal of muscles, nipple and damaged dermal tissue and without excision of the latter two. If the risk of breast cancer is high, then after prophylactic resection it is reduced by more than 90%.
Women with removed breasts resort to such an intervention so that the cancer does not spread to the second mammary gland, because relapses are common. During the operation, immediate or subsequent breast reconstruction using implants and the patient's own skin is possible. This subsequently relieves the woman of psychological discomfort after a unilateral or double mastectomy. Before and after restoration, the breasts look as shown in the photo.
According to Madden
The least traumatic and small in terms of invasion volume is a modified radical method, in which the tissue of the affected breast, fascia, partially the tissue under the scapula, armpit and lymph nodes are removed to the second level. Both types of pectoral muscles and type 3 lymph nodes remain intact. This technique is used in the Russian Federation in the early stages of cancer detection.
Peyti mastectomy
The Patey-Dyson operation is a modified, gentle method of removing the mammary gland, which belongs to the group of radical interventions and involves complete excision of breast tissue, the small muscle mass and partially fatty tissue. A large muscle mass is preserved. Lymph nodes of types 1–3 are also removed, but not all, but only those affected by cancer.
Endoscopic mastectomy is the latest technique for performing breast removal surgery using a special device. Punctures are made in the cancerous gland and the required amount of tissue is removed through them under the control of an endoscope. Therefore, this method is suitable for any type of intervention. The patient is under general anesthesia; subcutaneous mastectomy lasts no more than two hours. The use of this method is possible if the cancer has not affected the skin of the breast and nipple.
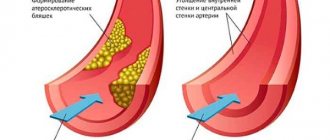
Removal of lymph nodes
Often, surgical treatment for breast cancer involves removing nearby lymph nodes. Previously, surgeons acted blindly. It was believed that if there is the slightest suspicion of damage to regional lymph nodes by cancer cells, it is better to remove the latter. This approach is logical and has helped save the lives of many women. But after removal of the axillary lymph nodes, a serious complication arises in the form of lymphedema - swelling of the arm. Currently, there is such a diagnostic procedure as sentinel biopsy , or sentinel lymph node biopsy . The surgeon injects a radioactive or fluorescent dye into the tumor tissue, which then penetrates the lymphatic vessels. The lymph node that received the drug first is called a sentinel or sentinel node . It is removed and examined under a microscope for the presence of cancer cells. If the sentinel lymph node is “clean”, there is no need to remove the rest.
Postoperative period
Breast amputation, regardless of typology, is a complex invasive intervention. You will have to spend about a week in the hospital, then the patient will have a recovery period lasting up to 3 months. After a mastectomy without plastic surgery, the operated patient will stay in the clinic for 4 days. In the first month, visits to the inpatient department are required for regular dressing changes and examinations.
When the anesthesia wears off, severe pain begins, lasting about 4-6 days. During this period, painkillers are usually prescribed. The patient must wear a drainage system for a week. Since you are sometimes discharged home with tubes attached to your body, the nurse will tell you in detail how to avoid damaging the device and dressing. You can get up and move around a little the day after surgery. In the future, wearing a corset and compression garments is recommended. Under no circumstances should you lift heavy objects or make sudden movements.
Disability after invasion is due if the diagnosis that led to the mastectomy is breast cancer. The intervention is followed by mandatory chemotherapy and radiation therapy, the consequences of which deprive the woman of her ability to work. Usually the patient is assigned a second disability group with re-examination after a year.
Modern approaches
The main question that arises during surgical treatment of breast cancer: is it possible to remove only the tumor, or is it worth performing a mastectomy? On the one hand, organ-conserving operations allow you to preserve breasts - one of the attributes of femininity. But won't this increase the risk of relapse? Currently, studies have been conducted and it has been found that lumpectomy, supplemented by a course of radiation therapy, is not inferior in effectiveness to mastectomy and is not accompanied by a higher risk of relapse. Many women can have their breasts preserved. Another question is that not every doctor may have enough experience, knowledge, and skill. Contact us and we will tell you where to find a good breast cancer surgeon.
Consequences
The postoperative period does not always go smoothly. Complications may appear immediately or later, and there is also a risk of relapse. Life after a mastectomy is often overshadowed by psychological worries, doubts about one’s own attractiveness, and the expectation of potential disability. If depression occurs, you will need the help of a psychotherapist.
Complications of mastectomy more often occur in elderly, chemotherapy-weakened, and obese patients. Within 3–4 days, bleeding and lymphorrhea are observed, sutures come apart, necrotic tissue damage, and purulent inflammation are observed. Later, phantom pain appears, disruption of venous and lymph flow, swelling, loss of sensitivity, keloid scars form, and limb movements are distorted.
Relapses of cancer occur six months to a year after mastectomy. Most often they occur if the operation was performed in the late stages of cancer due to incorrect diagnosis, refusal of radiation therapy, or the presence of active metastasis. After 5 years, cancer can be considered defeated.
It is important to follow the doctor’s recommendations even after the postoperative period. Contraindications after invasive mastectomy:
- No sex for three months.
- Do not take hot baths.
- Avoid saunas and steam baths.
- You can't get pregnant for three years.
- Holidays at sea for 3 years are not advisable.
- Do not lift weights exceeding 1–3 kg.
- Smoking and drinking alcohol are contraindicated.
- Sharp bends and raising of arms are excluded.
A salt-free diet is recommended, excluding fatty and smoked foods. The support of relatives is crucial in the rapid recovery of the operated patient.
Treatment continues
After the operation, the patient will undergo further treatment. The oncologist decides what it will be depending on the extent of the process (whether there were metastases in the axillary lymph nodes) and the sensitivity of the tumor to hormones. If the tumor was hormone-dependent, hormone therapy is prescribed. This treatment is the easiest: the patient will take 1–2 tablets of the hormonal drug per day for several years.
Question answer
Will “cutting off” save you from cancer?
There is, although not often, such a favorable option when only surgical treatment is sufficient. This happens if the tumor was caught at the 1st stage of development and there were no metastases in the lymph nodes. After the operation, the patient only needs to undergo dynamic observation by an oncologist.
Some patients will have to undergo chemotherapy. The first course is often carried out in the hospital, and upon discharge the patient receives recommendations for further treatment at the oncology clinic at her place of residence. And in some regions, the most modern treatment is already being used: targeted therapy (from the English word target - “target”), when the drug acts specifically on cancer cells and blocks their growth.