Table of contents
- Etiology and pathogenesis
- Clinical manifestations
- Principles of treatment
Acne (pimples, acne vulgaris, acne, comedones, acne vulgaris) is a chronic inflammatory skin disease that manifests itself as open or closed comedones and inflammatory lesions (papules, pustules, nodules).
In our company you can purchase the following equipment for acne treatment:
- M22 (Lumenis)
- Thermage (Solta Medical)
Today, acne, without exaggeration, can be called the most common skin disease among young people - according to statistics, up to 95% of boys and up to 83% of girls suffer from it. Approximately 60% of them have a mild form with a small number of rashes (so-called physiological acne). If acne occurs in adolescence, in 64% of adults, acne persists at the age of 20–30 years, in 43% at 30–40 years, in 15% at 40–50 years (more often in women).
Causes of acne
Causes:
- unbalanced diet. Wrong diet, constant exercise in gyms;
- prolonged exposure to direct sunlight without cosmetic protection;
- increased sweating;
- genetic predisposition;
- deterioration of the sebaceous glands;
- alcohol;
- smoking.
Hormonal imbalances, water imbalance, poor sleep.
In newborns
The statistics of the disease in newborns is 20%. Rapid development of papules in the cheeks, nose, closed comedones. Causes:
- hormonal crisis;
- excessive secretion rates.
Hormonal imbalance - a decrease in esterol levels in the first days after birth. Maternal use of systemic glucocorticosteroid drugs. There is no treatment. Natural restoration of the body in the first month. No scarring, no side effects. Recovery under the supervision of a dermatologist.
Etiology and pathogenesis
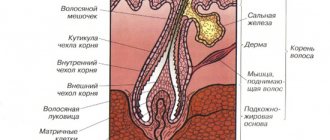
The main sex hormones that regulate the activity of the sebaceous glands are androgens . They affect the development and increase in the size of the sebaceous glands in androgen-dependent areas of the skin, the hyperproduction of sebum and the proliferation of keratinocytes in the ducts of the sebaceous glands, the hair canal and the mouths of the pilosebaceous follicles.
According to the inflammatory concept of acne, the chain of pathogenetic events begins with androgen-induced inflammation of the sebaceous gland . This causes proliferation and active desquamation of keratinocytes in the upper part of the pilosebaceous follicles. Progressive hyperkeratosis and the associated difficulty in the outflow of sebum lead to the formation of comedones , which subsequently transform into papules and pustules or spontaneously regress.
Overproduction of sebum contributes to changes in its qualitative composition. In sebum, the concentration of linoleic acid decreases, which suppresses the expression of transglutaminase and is involved in the synthesis of the main components of the intercellular matrix. This leads to an increase in the pH of sebum and a change in the permeability of the walls of the follicles and the stratum corneum of the epidermis.
Sebum stagnation creates anaerobic conditions that are optimal for the proliferation of propionibacterium acnes in the pilosebaceous follicles. They secrete substances that damage the walls of ducts and glands, as well as factors that attract neutrophils.
The release of lysosomal enzymes by neutrophils further reduces the strength of the follicle wall, which ultimately leads to their rupture. The contents enter the dermis, where local inflammation develops according to the “foreign body reaction” type.
Exogenous factors contributing to the development of acne:
- taking sex hormones, anabolic steroids ( Fig. 1 );
- high glycemic index diet;
- smoking;
- whole milk;
- fast food;
- chocolate;
- various occupational hazards;
- hot and humid climate.
Rice. 1. Acne on the shoulder and back of an athlete due to the use of anabolic steroids (Danish national service on dermato-venereology)
https://www.danderm-pdv.is.kkh.dk/atlas/4-120-9.html
Clinical manifestations
The general picture of acne is characterized by polymorphism ( Fig. 2 ). The evolution of acne elements is as follows:
| Closed comedones and milia → open comedones → follicular papules and nodules → follicular pustules → scars and spots. |
Clinical forms of acne:
- Prepubertal acne
- Juvenile acne
- Late acne
- Indurative acne
- Acne conglobata
Prepubertal (pre-adolescent) acne - occurs at the age of 7-12 years and is caused by the onset of puberty. There is an increase in skin oiliness and a large number of comedones, mainly on the forehead and in the central part of the face (T-zone).
Juvenile (ordinary, vulgar) acne is the most common type of acne. They are open and closed comedones, papules and pustules located on the forehead, nose, cheeks, temples, often on the chest and back. In girls, 5–7 days before the onset of menstruation, the rashes become more numerous.
Late-onset acne (adult acne) occurs more often in women. There are relatively few rashes - unlike youthful ones, they are located in the lower part of the face (on the cheeks, chin, around the mouth) and on the neck. Almost half of patients have a rash on their body. Papules exist for a long time (1–3 weeks), are painful, there are usually few or no comedones, exacerbations are associated with stress. Late acne also includes postmenopausal with the predominant formation of comedones and the absence of pronounced inflammation.
Indurative acne is characterized by an active inflammatory reaction and a predominance of deep-lying, dense, painful nodes that merge with each other. Subsequently, they heal through scars ( Fig. 3 ).
Acne conglobata - it affects mainly men with very oily skin. With age, there is a tendency to recovery, but outbreaks of the disease occur from time to time. The main morphological element is a large red painful hemispherical node. At first it is dense, but later softens. The nodes can merge and turn into abscesses, after opening which remain long-term non-healing ulcers and fistulas that heal with rough scars. Sometimes, when nodes merge, draining sinuses are formed. The disease is almost never limited to the skin of the face - on the contrary, the largest nodes are usually located on the chest and back.
To assess the severity of acne in clinical practice, it is convenient to use the recommendations of G. Plewig and M. Kligman ( Table 1 ).
Table 1. Determination of acne severity according to G. Plewig and M. Kligman (2004)
| Severity | Comedones | Papules, pustules | Papules (>1 cm) | Nodes, cysts, fistulas | Inflammation | Scarring |
| I (mild) degree - comedonal acne | <20 | <10 | No | No | No | No |
| II (medium) degree - papulopustular acne | >20 | 10–20 | <10 | No | Clear | No |
| III (severe) degree - papulopustular acne | >20 | >20 | 10–20 | Few | Strong | Eat |
| IV (very severe) degree - conglobate acne | A lot of | A lot of | >20 | A lot of | Very strong and deep | Eat |
A separate form of the disease is medicinal acne, which occurs while taking certain medications - these are glucocorticosteroids, anabolic steroids, androgens, thyroxine, antiepileptic drugs, barbiturates, anti-tuberculosis drugs, azathioprine, cyclosporine A, lithium salts, iodine, chlorine, bromine preparations, cetuximab , some vitamins (for example, group B).
Rice . 2. Polymorphism of acne elements on the patient’s cheek (Danish national service on dermato-venereology)
https://www.danderm-pdv.is.kkh.dk/atlas/4-102-4.html
Rice. 3. Scars on the face that appear after healing of large inflammatory elements of acne (Danish national service on dermato-venereology)
https://www.danderm-pdv.is.kkh.dk/atlas/4-133.html
Principles of treatment
A carefully collected anamnesis will allow the specialist to understand what tactics should be used in the treatment of acne in a particular patient.
Among the general recommendations, it is worth mentioning the possibilities of diet . You should eat more vegetables, avoid fast food, whole milk and casein-containing products, chocolate, saturated fats, trans fats, easily digestible carbohydrates, foods with a high glycemic index, and also eat regularly and properly, and monitor your weight.
A basic acne control strategy involves the following steps:
- Cleansing - you can use emulsions, solutions and foams that have a neutral pH (5.5–7.0). It is important that they do not contain anionic surfactants (surfactants) that increase alkalization of the stratum corneum of the epidermis. The fact is that this leads to its swelling, maceration and increased blockage of the mouths of the pilosebaceous follicles.
- Exfoliation - its purpose is to smooth the surface of the skin, free the mouths of the sebaceous hair follicles from accumulated secretions, exfoliate corneocytes and restore the normal outflow of sebum. This procedure should not be overused, since aggressive exfoliation leads to damage to the epidermal barrier, which is clinically expressed by redness, irritation, peeling and increased sensitivity of the skin.
- Skin nutrition - active ingredients may include: vitamin D, vitamin B2, vitamin C, genistein, daidzein, kigelia, tea tree oil, papaya, various prebiotics, formononetin, equol, apricot extract, basil extract, cornflower extract, chondrius algae extract Crispus, ginkgo biloba extract, etc.
- Sun protection is very important, since ultraviolet and infrared rays activate sebum production and reduce local immunity in the skin, which often leads to exacerbation of acne after sun exposure.
Avocutin (butyl avocadate) was biotechnologically isolated from avocado oil , a fatty acid ester that can suppress the synthesis of 5-alphareductase, an excess of which is present in the skin of people with acne. It has been established that as a result of using a product containing 3% avocutin, the oiliness of the skin of the face and scalp is reduced by a third in the first two weeks of use.
A fairly universal cosmetic ingredient that will also be useful for acne is bitter aloe extract (Aloe Ferox Extract). It destroys and blocks the activity of many pathological microorganisms - streptococci, staphylococci and propionibacteria.
To treat acne, you can use chemical peels, creams and gels with tretinoin, 20% azelaic acid cream, 10% sulfacetamide lotion, 2.5–10% benzoyl peroxide gels, various antibiotics (erythromycin, clindamycin), as well as injection procedures: PRP therapy (injection of platelet-rich plasma into the skin) or mesotherapy (for example, hyaluronic acid modified with vitamin C, cysteine and glutathione).
Western acne treatment consensus recommends a combination of topical retinoids with topical and systemic antimicrobial therapy. It has been proven that its effectiveness significantly exceeds monotherapy with these drugs, which is due to complementary mechanisms of action aimed at various pathogenetic factors of the disease:
- retinoids (tretinoin) reduce excessive desquamation of the epithelium, exhibit comedolytic and some anti-inflammatory effects;
- local antibiotics (benzoyl peroxide) reduce the number of propionibacteria in acne lesions and have some keratolytic effect;
- systemic antibiotics (doxycycline, minocycline) suppress inflammation and inhibit the proliferation of Propionibacterium acnes.
It is impossible not to mention systemic retinoids - isotretinoin preparations. They are typically used to treat severe and treatment-resistant forms of acne. For some patients, one course of oral isotretinoin is enough to achieve remission of the disease, while others require additional courses. One study found that 38% of patients treated with systemic retinoids had no signs of acne during a 3-year follow-up period, 17% had their disease controlled with topical therapy, 25% required topical and systemic antibiotics, and 20% received a repeat course. isotretinoin. Relapse was more common in young patients and girls. However, it should be remembered that for all its effectiveness, isotretinoin has serious side effects associated with the development of depression and possible suicide of patients.
Hardware treatment of acne can be used in cases where therapy with systemic retinoids is ineffective or contraindicated. There are at least 2 methods of effectively influencing the inflammatory elements of acne:
- Deep heating of the skin, which leads to normalization of sebum formation and improved cleansing of the mouths of hair follicles. Such heating can be carried out by an IPL system ( M22 ) or an RF device ( Thermage ).
- Exposure of the anaerobic bacteria Propionibacterium acnes to broadband pulsed light in the blue part of the spectrum in order to induce the formation of free radicals from the uroporphyrin metabolite in these bacteria and their subsequent death. This method is implemented in IPL systems equipped with a special filter ( M 22 IPL , Acne filter with passbands 400–600 nm and 800–1200 nm).
Questions from our users:
- acne treatment
- acne treatment
- acne laser treatment
- acne laser treatment Moscow
Complex therapy
A mild form of the disease is complex external therapy. Treatment is as prescribed by the treating doctor based on the diagnostic results. Methods:
- mechanical;
- chemical peeling.
Peeling is based on salicylic and pyruvic acid extract. Mechanical cleaning is the middle stage of treating the disease. An initial cleaning step is often necessary. It is planned to complete the chemical peeling with mechanical peeling. Additionally, complex use of general and local medications, antibiotics.
Treatment of moderate disease is an addition to the external type of systemic therapy. Peculiarities:
- comprehensive laboratory tests: clinical blood test, biochemical diagnostics, general urine analysis;
- in-depth study of the patient’s hormonal background.
Prescription of local and general antibiotics, use of oral contraceptives with a pronounced antiandrogenic effect.
Reference: androgens for effective treatment of women. Purpose - based on the results of a complete examination of the patient’s hormonal imbalances. Many oral hormonal medications have a pronounced effect: “Zhanin”, “Yarina”.
The complex course of the disease is characterized by taking medications based on isotretinoin. Medicines for advanced stages of chronic disease. Contraindicated in women prone to pregnancy - after prescribing contraceptive medications or procedures. Severe side effects:
- severe severe headaches;
- increased feeling of dryness;
- increased anxiety;
- periodic outbreaks of dizziness.
The use of isotretinoin-based medications is accompanied by careful monitoring by a dermatologist. Treatment of post-acne is complex and time-consuming compared to common acne. If there are primary signs of an inflammatory process, immediately contact an experienced dermatologist at the medical center.
The psychosomatic state of the patient in the presence of a chronic disease is a separate side effect. Pronounced feeling of stiffness, constriction. The resulting facial defects force people to lead a hidden lifestyle. Side effects:
- the rapid increase in numerous complexes;
- expressed feelings of resentment;
- significant deterioration in mood.
The doctor establishes close, trusting cooperation with patients. Parallel work is carried out with a professional psychologist. The drug and the correction method for treating the chronic course of the pathology are specified. Getting the first visible results.