Main reasonsVideo
Who should I sign up with? Prices
Unfortunately, the result of breast augmentation surgery does not always satisfy the patient 100%. Our clinic is often approached by patients who want to undergo repeated breast surgery to correct the results of unsuccessful plastic surgeries performed in various clinics not only in Moscow and other regions of Russia, but also abroad.
All photos of breast reconstruction
Photo report 1.
Before
7 days after stage 3 of reconstruction
Patient after radical mastectomy 3 years later (convalescent).
At the moment, a three-stage reconstruction of the right breast and a T-shaped lift of the left breast have been performed.
Determining the size
After all the measurements are received, you need to calculate the size. The rounded underbust circumference is subtracted from the rounded bust circumference. The resulting value will allow you to determine your bra cup size. If the difference is 10-12 cm - size zero, 12-14 - first, 14-16 - second, 16-18 - third, and so on. Each size is designated by a letter, for zero it is AA, for the first A, for the second - B, 3 - C, 4 - D, 5 - DD, and 6 - E.
Add the letter corresponding to your cup fullness to the rounded underbust measurement to get your bodice size. For example, 75B.
Photo report 2.
The patient has already undergone 2 stages in another clinic.
Stage 1.
Removal of the mammary gland.
Stage 2.
Installation of an expander for tissue stretching.
We will go through all other stages with the patient together.
Stage 3.
Removal of the expander and installation of a permanent implant.
Stage 4.
Lifting one breast and restoring the areola on the right breast using tissue from the left areola.
Stage 3. Removal of the expander and installation of a permanent implant.
Breast appearance before surgery:
As a result of the installation of the expander and its swing, the inframammary fold was displaced and the fold of the right breast is located significantly lower than the left healthy breast. We will remove the expander and install a permanent implant, restore the submammary fold of the right gland, expand the breast pocket upward to raise the right breast to the level of the left breast, and excise scars and adhesions. As a result of the operation, the submammary folds of the right and left breasts will be at the same level.
Photo of the breast with an expander:
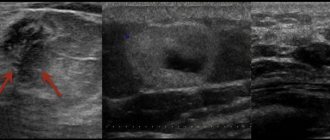
Carrying out the necessary measurements to plan the tactics of the operation:
An incision is made through which the expander will be removed and the implant installed:
Removing the expander:
Expander removal video.
Remote expander view:
Restoration of the submammary fold, expansion of the breast pocket, dissection of scars and adhesions:
Implant installation:
Skin suture after implant placement:
Video commentary by Sviridov S.V. after the operation is completed:
View of the breast before surgery and immediately after:
Before
After
What breasts look like after mammoplasty
We did not touch upon the topic of capsular contracture in the previous sections. That fibrous membrane that the body builds around any foreign body and breast implant too. The implant is designed in such a way that this capsule is formed thin and does not affect the softness of the implant. In rare cases, the body’s immune response to a foreign body is strongly expressed; the process of capsule formation continues throughout the entire time the implant is in place, which leads to the prosthesis being encased in a dense fibrous frame. The breasts harden and become deformed. Contracture can be unilateral or bilateral. Be pronounced or moderate.
The mechanisms of this response are not entirely clear. Prevention is only possible during the operation itself, but does not guarantee one hundred percent effectiveness. If this happens, then the first signs of compaction appear precisely in the first months or first years after breast replacement. Nothing can be done about this and we can only hope that the process will not be aggressive. At the moment, we operate with data on the risk of extreme forms of capsular contracture in the region of 8-10% over 10 years of observation. These are average numbers. The spread across different sources is very wide. Some report single percentages, others 15% or higher. It should be noted that the connection with the implant manufacturer, the type of texture of the breast implant shell, has not been clearly established.
There is complete clarity only on the issue of the need to excise the capsule around the implant in extreme degrees of capsular fibrosis.
Questions from our patients
I have had implants since 2010. Everything is fine, but the mammologist said that we need to change them to new, modern ones. What should I do?
— Firstly, you should not rely in this matter on the opinion of a mammologist who, being a specialist in the field of breast diseases, does not have surgical experience in breast prosthetics. Secondly, there is no concept of “new or “old” implants. This is not something that deteriorates over time or is released in new and improved versions every year. And, of course, there are no implants good or bad, reliable or unreliable, dangerous or safe. They can all be equally recommended for use. If you are happy with the result and nothing bothers you, then there is no point in thinking about a replacement. A breast examination for diseases of the mammary gland itself is indicated, as for any woman without implants.
I had prosthetics 4 years ago. Two years ago I gave birth to a child. A year ago I stopped breastfeeding my baby. Now the breasts hang and look ugly. What should I do? Change implants?
— If there are no signs of capsular contracture and the implant suits you in terms of volume, then we can discuss a breast lift on an existing implant. Formally, this is the excision of excess skin and the formation of a new breast shape due to a suitable “cut”.
I had an anchor breast lift a year ago. Breast size 2. The left one is a little smaller. I want the same size 3. What do you advise?
— Breast replacement (augmentation mammoplasty) with implants of different volumes to correct differences in volume. For access, you can use an existing scar under the areola or any other existing one (under the breast or vertical).
You can schedule a consultation with me by phone or by clicking
on the link .
I will always answer your questions!
With uv. Dr. Ross
Seam gluing during breast augmentation
Today, plastic surgery is developing exponentially. And the main goal of a plastic surgeon is to make scars as invisible as possible. Specialists use innovative technology of “seam gluing”. Its essence lies in the use of special medical glue for the skin. By the way, the seam gluing technique is often called the “seamless method of breast augmentation.” How does this happen?
In the operating room, the plastic surgeon applies a cosmetic suture to the wound using absorbable suture. This is an important point! Do not believe if they tell you that the edges of the wound will only be glued together with glue. There are always stitches! This is usually an absorbable thread, so the stitches are not removed after breast augmentation.
Only a stitched wound can be sealed by a plastic surgeon with glue. It is applied to the seam. In fact, medical glue acts as a kind of “plaster” that protects the wound and suture.
Advantages of seam gluing after mammoplasty:
- maximum protection of the seam from the external environment, bacteria and weathering;
- the seams do not require care;
- obtaining a high aesthetic result.
The scar after breast augmentation, made using the “suture gluing” technique, looks the same after 1 month as it did after 6-8 months. By the way, seam gluing is used for a tummy tuck (abdominoplasty).
Sizes in different countries
Most often, the manufacturer has a specific table that indicates the value in cm corresponding to the products presented in their line. Sometimes from some manufacturer your usual 70B may be small, or, conversely, large. Or you may not find such designations at all. The same applies to different countries - the size values are slightly different. Please check the tables carefully for consistency. Russian ones often coincide with the values given in the article. The same applies to linen from Belarus or Germany. With other countries everything is somewhat more complicated.
USA
Bodices are marked completely differently. To calculate your size, you can measure yourself in centimeters and then convert to inches (1 inch = 2.54 cm). The second way is to determine the length of your bodice using a measuring tape. You can simply outline it at the back, and slightly lift it at the front. The result should be divided by 2.54. You will get the chest volume in inches. To get your cup depth, subtract the previous measurement (in inches!) from your chest measurement. If the difference is 0, then your size is AA, 1 is A, 2 is B, etc. (the size will correspond to the difference in inches and the standard letter designation).
The smallest underbust size in the US is 30 inches. According to Russian tables, this is 65. Accordingly, 32 - 70, 34 - 75, 36 - 80, 38 - 85 and 40 - 90.
Europe
In France or Spain, to convert to Russian sizes, add the number 15. For example, for volume 75, French size is 90.
Italian sizes are designated by numbers from 1 to 7. For example, girth 65 - 1, 70 - 2, etc. In Australia, 65 equals 8, and each subsequent one adds 2 to size. That is, 70 is 10, 75 is equal to 12 and so on, up to 20 for a girth of 95.
It is also important to know the correspondence of international clothing sizes to bodice sizes. This will be relevant when choosing sports bras, swimsuits, and blouses. Everything here is quite simple - Russian AA corresponds to XXS, A - XS, and for the sixth Russian size the international size will be XXL. It is important to remember that cup fullness does not equal girth. Check the brand's sizing chart.
Why do keloid scars appear?
Keloid scars are a complication of breast augmentation. Among the reasons for their formation are the following:
- features of the body's immune system,
- hereditary predisposition,
- excessive skin tension in the healing zone,
- suppuration or infection of a postoperative wound.
It should be noted that sutures after mammoplasty rarely turn into keloids. This process mainly has a hereditary predisposition and manifests itself gradually, in some cases up to 2 years. Therefore, with constant monitoring by a doctor, you can notice changes occurring in time and stop their development.
How to care for seams?
Every patient, before stepping into the operating room, must understand that thin and barely noticeable scars after surgery will remain in any case. But thanks to proper and careful care, they can be made unnoticeable. Here is a list of basic recommendations on how to handle sutures after mammoplasty:
- Smoking is strictly not recommended during the period of preparation for the intervention and until final rehabilitation.
- It is mandatory to wear compression garments for up to six weeks after the surgical procedure.
- During the first week, contact with water is prohibited - the sutures after mammoplasty must be kept dry during this period.
- After hygiene procedures, it is necessary to apply a moisturizing cream or lotion to the stitches to avoid drying out the skin and to maintain its elasticity.
- For the first 2 months after surgery, physical activity on the shoulder girdle of muscles should be limited.