Skin depigmentation is the uneven coloring of the epidermis that occurs due to a deficiency of the coloring substance – melanin. Loss of pigmentation in the skin can be caused by genetics, exposure to ultraviolet rays, or a serious dermatological disease. The main symptom of pathological changes is the presence of lightened areas on the surface of the epidermis. Lightened spots can have different forms of expression, usually depending on the stage of the disease. You should consult a dermatologist with this problem.
Features of skin depigmentation
Depigmentation of the dermis indicates a violation of pigment metabolism in the human body. The disease can manifest itself in two forms: achromia (complete absence of coloring matter), hypochromia (deficiency of melanin in epithelial cells).
The appearance of lightened areas on the skin is considered by doctors to be the only sign of depigmentation. Since melanin is present in the hair, iris and inner ear, their color also changes. Depigmentation can be complete (lightened areas of the skin have no gaps and are continuous) and incomplete (uneven alternation of lightened spots with normal skin).
The disease is divided into persistent and temporary phases. In the first case, restoring the functioning of melanocytes is impossible. Temporary depigmentation can be treated with medication.
Content:
- Features of skin depigmentation
- The main causes of the disease
- Forms of depigmentation of the epidermis
- Depigmentation in children
- The main causes of skin depigmentation in children
- Diagnostics
- At-risk groups
- Preventive measures
Clinical classification. Types of melanoma
Melanoma manifests itself in various forms, there are 3 main types:
- Superficially widespread.
Tumor of melanocytic origin. The most common disease (70 to 75% of cases) among middle-aged Caucasians. Relatively small, complex in shape with uneven edges. The color is uneven, reddish-brown or brown, with small patches of bluish tint. The neoplasm tends to become a tissue defect, accompanied by discharge (usually bloody). Growth is possible both on the surface and in depth. The transition to the vertical growth phase can take months or even years.
The main causes of the disease
There are acquired and congenital causes of this disease. They are associated with the lack of melanin in certain areas of the skin. In rare cases, epithelial cells do not have an important pigment at all; an example is albinism, which is congenital.
Acquired causes include: chronic skin diseases; inflammation; long-term treatment with corticosteroids; starvation; pregnancy period; lack of iron in the blood; autoimmune disorders. Also acquired factors are endocrine dysfunction and dermatological diseases such as leprosy, streptoderma and psoriasis.
Depigmentation can occur due to prolonged exposure of a person to ultraviolet rays. Doctors can diagnose a pathology that is caused by a burn or previous trauma with skin damage.
Forms of depigmentation of the epidermis
The forms of skin pigmentation disorders are: albinism; vitiligo; idiopathic or guttate hypomelanosis; Ito's hypomelanosis. Congenital absence of melanocytes is hereditary. Features of the pathology are pronounced achromia or hypochromia, white hair, translucent irises, photophobia, pinkish skin tone. Albinism does not cause skin cancer in 90-95% of cases.
Vitiligo is a skin disease that causes lightened spots on the neck, upper and lower extremities. They can grow, merge and spread throughout the body. More often, white spots are localized on the knees, elbows, near the mouth and eyes.
The main cause of the disease is considered to be a deficiency of melanocytes. Other factors that influence the appearance of pathology include: disorders of the central nervous system; reduced immunity (if the cells responsible for pigmentation are damaged, vitiligo may develop); self-destruction of the coloring matter. Scientists have not yet fully figured out whether the disease is transmitted from parents to children or not.
Idiopathic hypomelanosis can be acquired or congenital. Typically, such depigmentation of the epidermis appears in children and adolescents. The spots have different shapes, and very rarely have clear contours. Guttate hypomelanosis is observed in 60-70% of cases in women over thirty years of age. People with fair skin get sick more often than people with dark skin.
Depigmentation increases after prolonged sun exposure. The first sign of pathology is light lesions on the legs. The spots are usually oval or round in shape (diameter reaches 1-1.5 centimeters). If the disease progresses, they appear on the chest, abdomen and back. The neck and face often remain outside the risk zone (up to 5% of cases have been recorded when guttate hypomelanosis was localized on the skin of the face and neck).
Ito's hypomelanosis is genetically transmitted. Symptoms of the disease usually appear in infancy. Signs of pathology: wavy and zigzag stripes on the epidermis; spots have different sizes; chaotic localization of clarified areas. During adolescence, pigment elements become smaller, and sometimes they disappear completely. Ito's hypomelanosis is quite often accompanied by a congenital malformation.
Sometimes people experience other forms of depigmentation: piebaldism (partial albinism, which is a rare autosomal dominant pathology); Bourneville disease (a rare genetic pathology, the peculiarity of which is damage to the central nervous system, skin damage, and the presence of hamartomas in internal organs); phenylketonuria (a disorder of amino acid metabolism causes depigmentation of the dermis and a profuse rash).
The first signs of melanoma
Melanoma is the acquisition by cells of unfavorable signs of malignancy (malignancy properties), expressed by various symptoms.
To make it easier to remember the signs of melanoma, use the “FIGARO” rule:
Shape – swollen above the surface;
And changes - accelerated growth;
Borders are openwork, irregular, indented;
And symmetry is the absence of mirror similarity between the two halves of the formation;
P size – a formation with a diameter of more than 6 mm is considered a critical value;
About paint - uneven color, inclusion of random spots of black, blue, pink, red.
In widespread practice, the English version is also popular, summarizing the main, most typical features - the “ABCDE rule”:
A symmetry is an asymmetry in which, if you draw an imaginary line dividing the formation in half, one half will not be similar to the other.
B order irregularity – the edge is uneven, scalloped.
Color is a color that is different from other pigment formations. Interspersed areas of blue, white, and red colors are possible.
D iameter – diameter. Any lesion larger than 6 mm requires additional observation.
E volution – variability, development: density, structure, size.
Without special studies, it is difficult to determine the type of nevus, but timely changes in the nature of the spot will help detect malignancy.
Depigmentation in children
Uneven coloration of the epidermis in children often appears from the moment of their birth. There are cases when the problem arises as the child grows older and affects only certain areas of the body. Depigmentation of the epidermis is, first of all, a cosmetic defect, which causes the appearance of complexes and internal clamps.
Since children's skin has a pale tint, parents cannot always detect pathology from the first days of life. They should monitor the condition of the baby’s epidermis and promptly consult with a pediatrician and dermatologist.
Character traits
A melanoma tumor developing from a nevus is characterized by a prolonged increase in changes (up to several years) and subsequent aggressive transformation (1-2 months). Early self-diagnosis and timely examination by a specialist will help identify the symptoms of melanoma:
- Smooth mirror surface, with disappearance of skin grooves.
- Increase in size, growth over the surface.
- Unpleasant sensations in the area of the mole: itching, tingling, burning.
- Dryness, peeling.
- Ulceration, bleeding.
- Signs of an inflammatory process in the area of the mole and surrounding tissues.
- The emergence of subsidiaries.
The sudden appearance of subcutaneous lumps and nodules may also indicate a developing disease.
The main causes of skin depigmentation in children
A deficiency or absence of melanin can be present from birth or occur in adulthood. Depending on the forms of depigmentation, the doctor judges possible other diseases. For example, with vitiligo, a child can suffer from infectious diseases.
Causes of skin depigmentation in children:
- genetic predisposition;
- stressful situations;
- central nervous system disorder;
- vitamin deficiency (vitamin deficiency in the body);
- intoxication and poisoning;
- problems with the thyroid gland.
The most common causes of depigmentation in children are frequent stress, strong emotions and mental disorders. Vitiligo usually becomes more active during adolescence. Doctors state that problems with melanin are chronic and occur over a long period of time. Infants develop white spots of various shapes, often with rounded or even edges.
Causes of changes in skin pigmentation and symptoms
Changes in skin color in certain areas - in the décolleté, arms, legs or face - are associated with disorders in the reproduction of melanocytes. This mechanism has not yet been fully studied. However, it is known that there are factors that contribute to the appearance of age spots. These include:
- Hormonal imbalances associated with puberty, pregnancy, menopause.
- Exposure to sunlight, which includes photoaging.
- Lack of vitamins in the body or, on the contrary, their excess.
- Genetic predisposition.
- Improper lifestyle, alcohol abuse and smoking.
- An age factor that is associated with a natural decrease in melanin production.
- Diseases of internal organs, for example, the gallbladder and liver, in which yellowing of the skin and sclera of the eyeballs is observed.
In addition, changes in skin color can be caused by the use of certain types of medications, in particular tetracycline, antihistamines and sulfonamides.
Diagnostics
Adult women and men who experience skin depigmentation should consult a dermatologist. This doctor diagnoses dermatological diseases and understands the issues of prevention and prevention of the development of serious pathologies. The specialist also studies the relationship between diseases and pathological and abnormal conditions.
The doctor may refer a patient with depigmentation of the skin to undergo a number of tests: allergy tests, blood tests for antibodies and antigens, scrapings, microflora cultures. The specialist may prescribe the patient a dermoscopic examination of skin formations.
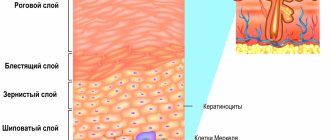
Methods for examining human skin are: palpation (the doctor determines the density and turgor of the dermis, its temperature, the presence of swelling, nodules); assessment of the color of the epidermis (the doctor visually assesses the condition of the nails, mucous membranes, hair, and looks for rashes, peeling, cracks and ulcers).
If a specialist has discovered any pathologies, it is worth taking into account their localization, symmetry, size, shape, color, mobility, and density. After examination and receiving the results of laboratory tests and studies, the dermatologist writes a conclusion and prescribes an effective therapeutic course.
At-risk groups
Best materials of the month
- Coronaviruses: SARS-CoV-2 (COVID-19)
- Antibiotics for the prevention and treatment of COVID-19: how effective are they?
- The most common "office" diseases
- Does vodka kill coronavirus?
- How to stay alive on our roads?
Depigmentation is very often treated with medications. After eliminating the main cause of the spots, they disappear or become less visible on the skin. The exceptions are albinism and vitiligo. The spots do not cause pain or discomfort to a person. The only disadvantage of the pathology is aesthetic unattractiveness and the appearance of complexes.
Uneven skin coloring most often appears in people before the age of twenty. People aged 30-40 years very rarely seek medical help. A person's race does not play a special role in skin diseases. According to statistical reports, dermatological diseases develop several times less often in men than in women.
Risk groups include people: with a genetic predisposition to skin diseases; have experienced a severe stressful situation; with second and third degree burns; with severe sunburn; with autoimmune diseases. With constant visits to solariums, the risk of depigmentation of the dermis increases by 2-3 times.
The pathology is not accompanied by pain or itching. The only problem with vitiligo and albinism is the psychological factor associated with the aesthetic appearance of the spots.
Principles of treatment
Treatment of abnormal skin pigmentation is based, first of all, on finding the cause that led to the development of this condition. However, in many cases, treating the underlying condition does not eliminate (or does not completely eliminate) skin discoloration. Therefore, you need to do the following:
- Normalize hormonal levels.
- Reduce skin sensitivity, “calm” it.
- Reduce inflammation.
- Restore microflora and barrier function of the epidermis.
- Strengthen antioxidant protection.
- Reduce melanin synthesis in pigment cells.
- Block the transfer of pigment from melanocytes to keratinocytes.
- Stimulate skin renewal.
- Protect skin from ultraviolet radiation and other negative factors.
Whitening ingredients and points of their application are presented in table. 1 .
Table 1. Ingredients and points of their influence on abnormal pigmentation
| Impact points | Ingredients |
| Inhibition of tyrosinase activity | Hydroquinone, resorcinol, kojic acid, arbutin, deoxyarbutin, ascorbic acid |
| Chelation of tyrosinase with copper | Ellagic acid, kojic acid |
| Suppression of glycolysis of tyrosinase | Glucosamine, N-acetin-glucosamine, tunicamycin |
| Melanosome transfer | Niacinamide, protease inhibitors |
| Inhibition of alpha-melanocyte-stimulating hormone binding to melanocytes | N-undecylenoyl-phenylalanine |
| Decreased tyrosinase activity | Retinoids |
| Antioxidant action | Vitamin C, vitamin E |
| Anti-inflammatory activity | Hydrocortisone, phytosterol, glycyrrhetinic acid, tranexamic acid, chamomile extract |
| Activation of cellular renewal | Retinoids, salicylic acid, alpha hydroxy acids, adenosine monophosphate |
Since the advent of devices operating on the principle of selective photothermolysis, they have become a reliable tool in the treatment of various forms of pigmentation, including abnormal ones.
If pigmentation is caused by the accumulation of melanin, IPL systems are successfully used, which selectively destroy areas of excess pigment accumulation due to their absorption of light energy.
In some cases, treatment of pigmentation is possible using an Nd:YAG Q-Switched laser. Its principle of action is instant heating of melanosomes with their destruction, which occurs very quickly and does not lead to a serious increase in temperature in the surrounding tissues. This method of therapy is suitable for types of hyperpigmentation that can be stimulated by intense heat. Fractional lasers are also successfully used to treat pigmentation, especially when the pigment is deeply embedded.
IPL, Nd:YAG Q-Switched and fractional lasers are included in the M22, which is the most versatile and convenient solution for treating pigmentation.
Questions from our users:
- abnormal skin pigmentation on the hands
- abnormal skin pigmentation on the hands treatment
- abnormal skin pigmentation laser removal
- abnormal skin pigmentation in the form of white spots