Table of contents
- Seborrheic dermatitis and dandruff
- Androgenetic alopecia
- Alopecia areata
- Scarring alopecia
- Diagnostic imaging of hair diseases
Hair diseases are pathologies of hair follicles and/or shafts, leading to disruption of their growth, structure, and function.
In our company you can purchase the following equipment for diagnosing hair diseases:
- FotoFinder dermoscope Vexia (FotoFinder)
- FotoFinder ATBM bodystudio (FotoFinder)
- FotoFinder (FotoFinder)
- Handyscope (FotoFinder)
The most common hair diseases are:
- Seborrheic dermatitis and dandruff
- Androgenetic alopecia
- Alopecia areata
- Scarring alopecia
Causes of problems
The reasons that can lead to hair problems can be divided into external and internal:
- External – hair dyeing and bleaching, prolonged wearing of tight and uncomfortable hats, tight hairstyles, injuries, improper care, aggressive environmental factors
- Internal - these are various skin diseases, intoxications of the body, infectious diseases, the postoperative period, allergic reactions, hormonal disorders, disorders of the nervous system, deficiency conditions, disruption of the gastrointestinal tract, etc.
Seborrheic dermatitis and dandruff
Papulosquamous disease associated with inflammation of areas of the skin rich in sebaceous glands. When it occurs on the head in a mild form, it is called dandruff. The prevalence of seborrheic dermatitis in the world is 3-5%, dandruff is more common - up to 15-20%.
Pathogenesis of seborrheic dermatitis
The pathogenesis of seborrheic dermatitis is complex and is at least partially related to the most common fungi in the human body, Malassezia. They live both on the surface of the stratum corneum of the epidermis and inside it, as well as in the area of the hair funnel - the recess of the skin where the hair root passes into the shaft. On the surface of the skin, fungi interact mainly with dead corneocytes, and in the area of the hair funnel they also affect living keratinocytes, since the barrier function here is reduced. But most of all, Malassezia is “interested” in sebum, the components of which this fungus feeds.
Under the influence of the environment and the skin microbiome, triglycerides and sebum esters break down into di- and monoglycerides, glycerol and fatty acids - the latter are saturated and unsaturated. Due to a lack of desaturase, Malassezia is only able to metabolize saturated fatty acids. As a result, a lot of unsaturated fatty acids remain on the skin , which, with a certain sensitivity of the epidermal barrier, begin to destroy it. The genetic defect responsible remains to be determined.
Research suggests that patients with seborrheic dermatitis and dandruff have increased skin barrier permeability, which is exacerbated by unsaturated fatty acids, particularly oleic acid. As a result, chronic inflammation and active exfoliation of corneocytes are triggered, which is manifested by typical symptoms of seborrheic dermatitis and dandruff.
Interestingly, the number of Malassezia in sick and healthy people is approximately the same - the state of epidermal defense and innate immunity is key.
Seborrheic dermatitis clinic
The appearance of seborrheic dermatitis on the scalp ranges from a light whitish coating to extensive thick crusts. From the scalp they can move to the forehead, the back of the neck and the auricle and postauricular area ( Fig. 1 ). Sometimes seborrheic dermatitis spreads to the chest, interscapular, axillary or groin area.
In more severe cases, the affected areas appear as scales against the background of a red, inflamed focus. With secondary infection, eczematoid dermatitis develops with weeping and crusting. People with dark skin phototypes (V–VI) may experience focal hypopigmentation.
Rice . 1. Seborrheic dermatitis on the auricle (Danish national service on dermato-venereology)
Trichoscopy of seborrheic dermatitis
- Red lines
- Yellow and brown dots
- Hidden hair
- Perifollicular white plate
- Twisted red loops
- Cricoid vessels
- Pigmented honeycomb
- Atypical red vessels
- Perifollicular hyperpigmentation
- Glomerular vessels
- Structureless red areas
- Vessels in the form of commas ( Fig. 2 ).
Rice. 2. Trichoscopic sign of seborrheic dermatitis - comma-shaped vessels (Kibar M., et al. Dermoscopic findings in scalp psoriasis and seborrheic dermatitis; two new signs; signet ring vessel and hidden hair. Indian J Dermatol 2015; 60(1): 41 –45)
Laboratory tests for diffuse effluvium
In patients with effluvium of unknown cause, laboratory testing should be performed to exclude, in particular, the following: Iron deficiency (ferritin) (7) Thyroid dysfunction (TSH, T3, T4) Stage II syphilis (TPPA test). Syphilis is very rare, but omitting an appropriate history or TPPA test in a patient with hair loss can have serious consequences for both the patient and the clinician if neurosyphilis develops further.
Androgenetic alopecia
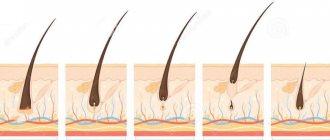
A genetically determined disease in which hair gradually transforms from thick terminal to intermediate and then to thin vellus, followed by baldness. Vellus is a small, weakly pigmented hair with a diameter of less than 30 microns and a length of less than 2 cm. Its bulb is located at the level of the reticular layer of the dermis, and the shaft is devoid of medulla and the levator pili muscle. The norm for vellus is considered to be up to 20% inclusive.
Androgenetic alopecia (AGA) affects about 50% of men after 40 years of age. Up to 13% of premenopausal women have some signs of AGA, and the incidence of the disease increases after 65 years - according to some data, AGA at this age occurs in 75% of women.
Pathogenesis of androgenetic alopecia
One of the basic mechanisms of AGA is considered to be the influence of the enzyme 5-alpha reductase, found in the cells of the hair follicle and papilla, on testosterone. This sex hormone is transformed into a more active 5-alpha-dihydrotestosterone, which penetrates the cell and forms an activated complex with a cytoplasmic protein. After interacting with a nuclear acceptor, the complex moves into the cell nucleus, where it disrupts protein synthesis - as a result, the size of the follicles decreases, and the hair turns from terminal to vellus.
Another mechanism of AGA occurs in women. The aromatase enzyme transforms testosterone into estradiol, and dihydrotestosterone into estrone. These estrogenic hormones have a modulating effect on androgens, resulting in the development of androgenetic alopecia of the female type.
These are not all the mechanisms of AGA - scientists are constantly finding new links in pathogenesis, as a result of which the overall picture becomes more complicated.
Androgenetic alopecia clinic
Main symptoms of AGA:
- Gradual onset of the disease
- Increased hair loss ( Fig. 3 )
- Transformation of hair from thick pigmented terminal hairs to thinner indeterminate ones and then to short thin vellus hairs without pigment.
- As a result, areas of complete baldness appear.
In men, the hair in the temporal areas gradually becomes thinner, which leads to a change in their growth line. The hairline on the forehead is often affected.
In women, hair thinning may not result in complete baldness, but when it does occur, it is usually on the top of the head. At the same time, the frontal and temporal growth lines in women are almost never affected.
Rice. 3. Degree of hair loss (the number of hairs per day is indicated): 1–4 - normal, typical for women with long hair; 5–6 - increased, leading to alopecia (Sinclair R., et al. Androgenetic alopecia: new insights into the pathogenesis and mechanism of hair loss. F1000Res 2015; 4(F1000 Faculty Rev): 585)
Trichoscopy for androgenetic alopecia
- An increase in the number of vellus hairs of more than 20% is the main diagnostic sign of AGA.
- Anisotrichosis is a heterogeneity in hair diameter that occurs due to the fact that the process of miniaturization does not occur simultaneously.
- Yellow dots are the mouths of empty hair follicles filled with sebaceous secretions, which are formed due to an increased latent period of hair.
- White dots are a reflection of fibrosis of the hair follicles.
- An increase in the number of single follicular units is observed with a decrease in the number of active hair follicles.
- Brown halo - occurs due to microinflammation in the follicle. Such patients are less responsive to therapy.
- Reduced hair density can be both local and diffuse in nature ( Fig. 4 ).
Rice. 4. Reduced hair density in androgenetic alopecia (Sinclair R., et al. Androgenetic alopecia: new insights into the pathogenesis and mechanism of hair loss. F1000Res 2015; 4(F1000 Faculty Rev): 585)
Taking a history of a patient with hair loss
The complaint of “hair loss” may indicate one of two things: an increased amount of hair being lost daily (effluvium) or visible baldness (alopecia). Up to 100 hairs are typically lost daily (3). It is important to ask patients about the medications they are taking. While “hair loss” is listed as a possible side effect in almost all drug labels, only some drugs actually have this as an issue (e1). For example, hair loss after 2-4 months is not uncommon after multiple injections of heparin (e2). Women should be asked about gynecologic factors such as initiating or stopping hormonal contraceptives. Transient postpartum hair loss is normal: labor stress and hormonal changes after childbirth cause many hair follicles to transition from the anagen to telogen phase, and thus hair loss may be noticeable after 2–4 months (2). Highly toxic factors such as chemotherapy drugs can cause severe damage to the follicles, causing hair to break off within the follicle within one to three weeks. As a reassurance, patients can be told that this process synchronizes the growth phases of the follicles so that when the hair grows back, it is often thicker than before. Structural changes may occur in which initially straight hair will re-grow as curly hair, or vice versa (4).
Terminology
Increased daily hair loss is called “effluvium”; visible baldness is called “alopecia.”
Alopecia areata
An autoimmune disease characterized by non-scarring hair loss. It is a widespread pathology - up to 3.8% of all dermatologist patients suffer from focal alopecia. About 20% of patients are children, and in 60% the disease manifests itself before the age of 20 years.
Pathogenesis of alopecia areata
The exact pathogenesis of alopecia areata is unknown. The most popular hypothesis is that it is an autoimmune condition associated with a T-cell immune response in genetically predisposed individuals.
Clinic for alopecia areata
Alopecia areata is usually asymptomatic, but some patients experience burning or itching in the affected area. About 80% of patients have 1 area of baldness, 12.5% have 2 areas, 7.7% have 3 or more areas. Alopecia areata most often affects the scalp - 70–95% of cases, less often the beard - 28%, eyebrows - 3.8% and limbs - 1.3%.
Localized form (alopecia areata) - less than 50% of the hair falls out, the affected areas are limited, in most patients the hair grows back spontaneously within a few months ( Fig. 5 ).
Common form (total/universal alopecia) - more than 50% of hair falls out; this option is less common (on average in 7% of patients). In 30% of patients with total alopecia, complete hair loss occurs within 6 months after the onset of the disease.
Rice . 5. Alopecia areata (Danish national service on dermato-venereology)
https://www.danderm-pdv.is.kkh.dk/atlas/4-18-4-1.html
Trichoscopy for alopecia areata
- Short vellus hair
- Yellow dots
- Black dots ( Fig. 6 )
- Broken hair
- crimped hair
- Exclamation mark hair
Rice. 6. Trichoscopic signs of alopecia areata: black spots ( blue arrow ) and crimped hair ( red arrow ) (Jha AK, et al. Dermoscopy of alopecia areata - a retrospective analysis. Dermatol Pract Concept 2017; 7(2): 53–57)
Physical examination
An examination of the scalp will show whether there is a visible reduction in the amount of hair (alopecia) and, if so, of what nature. Inflammatory erythema or scaling should be noted, as psoriasis and eczema can cause effluvium (e3). Dermatoscopy of the scalp is also useful (5). The clinical hair pulling test is complemented by a tricho(rizo)gram, in which 20–50 hairs are epilated with a rubberized hemostat and then analyzed under a microscope. Thus, it is possible to count roots of varying degrees of maturity in each growth phase. A percentage of telogen phase hair greater than 20% indicates increased hair loss (6, e4). Non-invasive phototrichogram can also assess the anagen to telogen ratio (e5), but cannot detect root abnormalities such as hair dystrophy.
Scarring alopecia
They represent the loss of the mouths of hair follicles with their replacement by fibrous tissue and irreparable hair loss. Cicatricial alopecia occurs against the background of viral or bacterial infections (systemic lupus erythematosus, pustular and fungal skin lesions), as well as after physical trauma, thermal or chemical burns. The worldwide prevalence is about 7%.
Classification of cicatricial alopecia
- Associated with lichen planus follicularis:
- Frontal fibrosing alopecia is a common clinical variant of lichen planus follicularis that develops in postmenopausal women.
- Patterned fibrous alopecia has histological and clinical similarities to androgenetic alopecia.
- Graham-Little syndrome is a polymorphic dermatosis with follicular atrophic keratosis of unknown etiology.
- Central centrifugal cicatricial alopecia is a broad category of alopecia recognized by the North American Hair Research Society. It is not a clinical variant in itself, but includes some pseudopelades, traction alopecia, etc.:
- Broca's pseudopelade is an alopecia alopecia that occurs in women after 40 years of age.
- Traction alopecia - develops with prolonged mechanical impact on the hair. It is more often observed in the African-American population due to hair styling in tight braids - up to 17% of girls aged 6–21 years and up to 32% of older women suffer from this pathology. Traction alopecia is common among athletes who wear their hair in tight buns during training and among professional break dancers.
- Mucinous alopecia - occurs against the background of mycosis fungoides.
- Alopecia after chemotherapy - develops after several courses of cytostatic drugs.
- Atrophic keratosis pilaris includes a range of clinical manifestations that lead to scarring hair loss.
- Secondary systemic cicatricial alopecia occurs against the background of systemic diseases of the body: scleroderma, discoid lupus erythematosus, etc.
Pathogenesis of cicatricial alopecia
Primary cicatricial alopecia develops due to a chronic inflammatory process in the hair follicle area. An important point in pathogenesis is the location of the infiltrate in the upper half of the follicle - the area of the sebaceous glands, under which multipotent stem cells of the bulge zone are grouped. Since the sebaceous glands and bulge are key structures that determine hair growth and regeneration, their loss leads to its death. A decrease in the number of sebaceous glands is also an early histological sign of the disease.
The pathogenesis of secondary cicatricial alopecia is associated with systemic diseases of the body - for example, scleroderma.
Scarring Alopecia Clinic
- Associated with lichen planus - common symptoms include itching, burning and pain. 30% of patients develop androgenetic alopecia.
- Central centrifugal cicatricial alopecia - slow, asymptomatic hair loss is observed.
- Alopecia mucinosa - Patients report dyshidrosis (eczema-like symptoms with clear blisters in the epidermis) and dysesthesia (changes in sensation).
- Alopecia after chemotherapy is accompanied by a tingling sensation in the scalp. Cytotoxic effects on hair follicles result in temporary hair loss, usually after 4 weeks of treatment ( Figure 7 ). New hair grows after the start of anagen, i.e. on average after 6 months, subject to completion of chemotherapy.
- Atrophic keratosis pilaris - Patients with keloid acne usually complain of itching, burning and increased sensitivity of the skin.
- Secondary systemic cicatricial alopecia - itching, burning, soreness of the scalp.
Rice . 7. Alopecia after chemotherapy (Danish national service on dermato-venereology)
Trichoscopy of cicatricial alopecia
- Large branching vessels
- Elongated vascular loops
- Perifollicular plaque ( Fig. 8 )
- Dotted vessels with white halo
- Whitish and reddish areas with minimal follicular ostia
- Mottled brown pigmentation ( Fig. 9 )
- Structureless yellowish areas
- White dots
- Black dots
- Yellow convex dots with dystrophic hair inside
Rice. 8. Trichoscopic signs of cicatricial alopecia in follicular lichen planus: a - perifollicular plaque, b - elongated vascular loops, c - classic white dots with a tendency to form fibrotic areas (Rakowska. A., et al. Trichoscopy of cicatricial alopecia. J Drugs Dermatol 2012;11:753–758)
Rice. 9. Trichoscopic signs of cicatricial alopecia in discoid lupus erythematosus: a - thick branching vessels, b - large yellow dots, c - spotted brown pigmentation (Rakowska. A., et al. Trichoscopy of cicatricial alopecia. J Drugs Dermatol 2012; 11: 753 –758)
Diagnostic imaging of hair diseases
As can be seen from the description of hair diseases, visually assessed signs are of great importance in their differential diagnosis. Trichoscopy is a separate young direction in dermatoscopy, which combines techniques for examining the scalp using a dermatoscope.
Today, there are about 200 nosologies among hair diseases, and in most cases, trichoscopic examination is necessary for proper treatment. The most modern and convenient method is digital trichoscopy - a study using a dermatoscope that takes digital photographs, as well as processes and stores them. This typically uses 60x or 70x magnification, which is much higher than a regular dermatoscope. This is very important because... During trichoscopy, it is necessary to visualize the condition of small vessels, hair shafts and follicles.
A recognized leader in digital dermatoscopy is the German company FotoFinder, which produces a range of software and hardware systems, including for diagnosing hair and scalp diseases. Today, all the leading trichologists in the world use FotoFinder solutions, and most trichology textbooks and atlases are created on FotoFinder digital cameras.
Another research method in trichology is trichography . It consists of a quantitative assessment of the condition of the hair: counting the number and density of hair shafts, the number of follicles, the proportion of thin, medium and thick hair and other characteristics that are important primarily for assessing the effectiveness of treatment.
The modern standard is the phototrichogram, during which digital photographs taken with a dermatoscope are stored and analyzed. This technique cannot yet be fully automated - the calculation is done manually, which is not very convenient and takes a lot of time. Fortunately, there are already remote analysis services for entrusting routine calculations to professionals. They will not only determine all the parameters of the phototrichogram, but also make a presumptive diagnosis. A striking example of such a service is tricholab.com, a division of FotoFinder that brings together world-class experts in the field of trichology.
When diagnosing a number of hair diseases, an important sign is to assess the amount (density) of hair in the anagen stage. Today this can be done using computer analysis using FotoFinder software products. This requires preliminary preparation of the patient: a small section of the skin is shaved, after 48 hours the growing hair is dyed, a picture is taken and analyzed using a special program. Hair in anagen grows within 48 hours and is very different in length from other hair. The program can recognize and count anagen hair, quickly providing the doctor with the most accurate information.
Questions from our users:
- hair diseases in women
- hair loss diseases
- hair diseases statistics
- treatment of hair diseases