Quick transition Treatment of alopecia areata
Alopecia areata is a skin disease in which areas of hair loss quickly, often suddenly, appear on the scalp or any other areas of the skin.
In alopecia areata, the body's immune system attacks the hair follicles for unknown reasons.
Hair loss is not accompanied by the death of hair follicles. This means that the hair loss process is reversible and hair growth can be restored in most patients. In almost half of the cases, hair growth is restored within a year, however, as a rule, the course of the disease is not limited to just one episode.
The onset of the disease is possible at any age, but the first episode most often occurs before the age of 30 years.
Forms and complications of alopecia areata
According to the prevalence of the process, alopecia areata is divided into the following forms:
- local - one or more clearly defined areas of hair loss;
- subtotal - more than 40% of hair on the head is missing;
- total - complete loss of hair on the head;
- universal - hair is completely absent on the scalp, in the area of eyebrows and eyelashes, and on the skin of the body.
There are forms with band-type prolapse in the occipital (ophiasis) or frontal zone (sisapho), as well as a multifocal form. A special form is diffuse - foci of hair loss visible to the eye do not form.
Stages of pathology development
Pathology goes through the following stages of its development:
- Progressive. At this stage, areas without hair gradually expand and new lesions appear. To pull out a hair, just pull it lightly. The stage is also characterized by slight itching of the affected area.
- Stationary. At this stage, new lesions do not form, the skin stops becoming inflamed, becomes smooth and turns pale.
- Regressive. Areas with receding hairlines are overgrown with new hair. Then they thicken and become pigmented.
If the pathology worsens, the transition to the first stage will occur again, the process will be started again.
Treatment of alopecia areata
Treating alopecia areata is not an easy task. To date, there are no methods with proven effectiveness. Moreover, in an impressive number of patients (up to 50%), alopecia areata can go into remission spontaneously, without treatment. Patients themselves do not always choose treatment, preferring to wait for spontaneous remission or undergo aesthetic replacement correction using a wig or hair system.
Treatment for alopecia areata includes:
- corticosteroid hormones - can be used topically, in the form of ointments, intralesional injections, orally;
- vasodilator antihypertensive agent for stimulating hair growth Minoxidil - used externally outside the acute stage, can be useful for mild forms of alopecia areata;
- immunosuppressive therapy (Cyclosporine, Methotrexate) - used when long-term maintenance treatment is necessary;
- PUVA therapy, long-wave ultraviolet irradiation of lesions in combination with a photosensitizer drug, is carried out in specially equipped dermatology departments, its effectiveness is currently questioned, and recommendations for the use of the method are ambiguous.
Alopecia areata cannot be completely cured. Even after achieving a good effect and complete remission, repeated episodes of hair loss are possible.
Intralesional corticosteroid injections
The procedure of intralesional corticosteroid injections is recommended for adult patients (in some cases adolescents) with a limited area of hair loss. It is performed by a doctor under local anesthesia with lidocaine cream (Emla). The frequency of the procedure is 1 time every 4-6 weeks (prescribed by a doctor).
The advantage of intralesional administration of corticosteroids is the ability to create a high concentration of the drug in the lesion.
Disadvantage : pain associated with parenteral administration (injection) of the drug.
Systemic therapy
In severe forms with rapid formation of extensive foci of hair loss, an initial course of systemic corticosteroids is possible. It is limited in time due to the rapid development of side effects. As independent therapy or to maintain the effect obtained while taking systemic corticosteroids, it is possible to prescribe drugs with an immunosuppressive effect (Ciclosporin, Methotrexate). All of these drugs show moderate effectiveness, are prescribed without registered indications and have a significant number of side effects. Their appointment requires constant medical supervision. The course of treatment is up to a year or longer.
The advantage of systemic therapy is its global impact on the process of autoimmune inflammation (not only locally in existing lesions). Prescribing such therapy is important when new lesions continuously appear against the background of overgrowth of old ones.
Disadvantage : side effects, lack of products with 100% effectiveness.
How is alopecia areata treated at the Rassvet Clinic?
The dermatologist will ask you to talk about the course of the disease and the treatment that was carried out previously. The diagnosis of alopecia areata in most cases is established on the basis of clinical examination. To clarify the diagnosis, the doctor may perform trichoscopy (examination of the scalp with magnification). In difficult cases, a skin biopsy may be required.
Causes of pathology
Before treatment, it is very important to establish exactly why the disease occurred.
The main factors provoking pathology include:
- Heredity.
- Chronic respiratory tract infections that are not fully treated. The infection penetrates the hair follicles, the immune system begins to fight it, and this leads to the death of the hair follicles.
- Constant stress and prolonged depression. They negatively affect the circulatory system, increasing blood viscosity and causing vascular spasms. Hair does not receive the required amount of oxygen and nutrients.
- Malfunctions of the endocrine system. If there are disorders in the thyroid gland or adrenal glands, the pituitary gland also suffers. This also becomes the reason that alopecia (including alopecia areata) begins to develop.
- Hormonal disorders. They can occur during pregnancy, taking contraceptive medications, and during menopause. Important! Pregnant women are not usually treated. This is due to the fact that after the birth of a child, alopecia usually goes away on its own.
Recommendations for patients
- Avoid mechanical trauma to hair when washing and combing.
- Avoid tight hairstyles.
- Eat fully and balanced.
- If necessary, do not be afraid to correct with a wig or hair replacement system.
- Some men (and women) prefer shaving to treatment.
- Do not forget about photoprotection; a hairless scalp is not protected from exposure to sunlight.
- Be careful with coloring, young growing hair may turn a different color.
- Be careful with extensions, artificial eyelashes and eyebrows, tattooing, and the use of masking fibers.
- Psychological and informational support can be obtained from special resources on the Internet and in communities for patients with alopecia areata. If you need specialized help, see a psychotherapist.
Author:
Voronina Vera Removna dermatologist
Benefits of therapy at An-Tech Labs
Our laboratory employs exclusively experienced doctors. All trichologists have the knowledge and skills necessary for effective and safe therapy. They successfully treat even advanced forms of pathology. But we strongly recommend contacting An-Tech Labs as early as possible to prevent hairless lesions from spreading.
When starting treatment for baldness, we provide:
- Individual approach. It consists of careful diagnosis and selection of means and methods that are suitable for a particular patient.
- A complex approach. Baldness therapy is carried out using several means at once.
- Professional consultations and innovative diagnostics. They make it possible to find out why the patient has alopecia and how baldness can be eliminated.
- No queues. This is ensured by a sufficient number of doctors.
- Attentive attitude towards patients on the part of all clinic staff.
Contact us!
The treatment process can be started by our trichologists in the near future. Back to list of services
Baldness (alopecia) – how to cope with the problem?
In many cultures, both ancient and medieval, hair was seen as the center of the soul, a carrier and a symbol of strength. The ancient gods Zeus, Apollo, Venus, the Old Testament David and Samson had lush hair. The insidious Delilah, with the help of a slave, cut Samson’s hair, and “...his strength departed from him,” but when the hair grew back, Samson’s strength returned. Hair, as a very significant object, was sacrificed to the gods: in Ancient Greece to Artemis after a successful birth, in Ancient Rome - to Virbius upon marriage. Priests of the ancient Egyptian goddess Isis, Indian Brahmins and Buddhist monks shaved their heads, emphasizing their slavish submission to the deity. The tonsure of Christian monks is a sign of dedication to God, the removal of secular thoughts, a symbol of the crown of thorns of Christ. It was customary among many peoples to shave or cut their hair during mourning ceremonies. It was widely believed that having hair makes it possible to influence the human psyche, so after cutting it they were not thrown away, but carefully hidden so that they would not get to enemies, evil forces or animals close to them. However, they tried to have the hair of a loved one with them; they were kept in special medallions. As it was believed at that time, the hair of saints and righteous people had special powers of amulets; they were even placed in the parts of weapons. The way of styling hair has had great social significance at all times and influenced the image of a person, often indicating the caste and profession of a person, his marital status.
Our mental reactions are reflected in a certain way in the way we organize our hair, we try to give a signal to the environment about our sense of self. This is why the loss of part or, moreover, all hair is perceived so acutely by a person.
Alopecia is a pathological hair loss; a distinction is made between cicatricial alopecia, caused by the destruction of hair follicles due to inflammation, atrophy or scarring (for example, after injury) and non-scarring alopecia, which occurs without prior damage to the skin.
A little about hair physiology
Almost 95% of human skin is covered with hair; its color, thickness and density are determined by the individual characteristics of the body and age. Long hair is located on the scalp, pubic area, armpits, mustache, beard; bristly hair is located on the eyebrows, eyelashes, skin of the nostrils and external auditory canal, vellus hair is located on the entire rest of the body. Sebaceous and (in most cases) apocrine sweat glands are always associated with hair. Hair is distributed in the skin along certain metametric lines, unevenly, the largest amount of it is located on the skin of the scalp, with maximum density on the crown, where the hair is thickest and longest (on average 60-75 cm, can be up to 1-1.5 m ). The change of long hair occurs every 5-7 years in women and 0.5-2 years in men; the maximum length of newly formed hair can be achieved at any age, except old age.
Anatomically, the hair is divided into the shaft - the part that protrudes above the surface of the skin, and the root - the part located in the dermis and surrounded by the epithelial root sheath (hair follicle). The hair follicle is formed from the invagination of the fetal epidermis during intrauterine development, is a unique mini-organ and plays a critical role in the process of hair growth and its disorders. The lower part of the hair is called the hair follicle, and both root epithelial sheaths merge with it. The lower part of the onion (matrix) consists of undifferentiated cells that have enormous and time-independent mitotic activity (even tumor cells do not have such high proliferation). Here there are also Langerhans cells, which protect hair from the penetration of damaging antigens, and melanocytes, which synthesize different types of melanin, which changes the pigmentation of hair and skin. Melanogenesis is strictly regulated, its intensity is influenced primarily by the hypothalamus and adenohypophysis, which stimulate the release of melanocyte-stimulating hormone, and the pineal gland (epiphysis), which produces melatonin, which suppresses the functions of melanocytes. Stimulates melanogenesis ACTH, hormones of the gonads, adrenal cortex, vitamins B1, B2, and suppresses catecholamines. From below, connective tissue protrudes into the hair follicle, abundantly supplied with hemocapillaries, the so-called. dermal papilla, which is a kind of computer that regulates hair growth. Hair follicles are richly supplied with afferent nerve fibers; these are finely tuned receptor devices. In the epithelium of the outer root sheath of the follicle there are clusters of Merkel cells - neuroendocrine skin cells in which various neuropeptides and growth factors are localized. These cells are related to the regulation of the metabolism of pain modulators - substance P, endorphins and enkephalins; when the skin is stimulated, their release increases. Met-enkephalin is also a strong stimulant of the immune system, helping to better resist infectious diseases and cancer processes. Maybe that's why people and animals like to be stroked and brushed.
In long and bristly hair, the root is formed by 3 layers of cells: the inner medulla, the middle cortex and the hair cuticle, located on the outside. The hair root medulla consists of one or more layers of cells, all derived from a stem cell located directly above the papilla. Moving upward during hair growth, these cells differentiate. In humans, the medulla is found only in long hair, where it is located either in a reticular pattern or in a continuous homogeneous strand. The cortex of the hair root consists of one or more layers of cells, which also differentiate from the cambial cells of the bulb. The cells of the cortex are densely located, oriented along the axis of the hair, make up its bulk and determine its mechanical strength. The hair cuticle is adjacent to the cortex layer. In the middle zone of the follicle there is a zone of keratinization (keratinization), where the hair gains strength due to the formation of proteins - keratins, containing large amounts of sulfur, disulfide bonds and cysteine. At this stage, the differentiation of hair cells ends, the cells lose water and, as a result of complete keratinization, die. The cells of the inner root membrane end at the level of the sebaceous gland duct. The secretion secreted by these glands lubricates the hair and gives elasticity to the skin, and also prevents heat loss.
The hair shaft, in which all differentiation processes have already been completed, consists mainly of compact, fully keratinized cortical cells, which are located along the axis of the hair. There is a hollow space in the center of the hair, which improves its strength and thermal insulation properties. The cortical cells are surrounded and protected by the cuticle, which contains up to 10 layers of cells arranged like tiles and directed towards the tip of the hair along its entire length. Hair is one of the most resistant structures of the body to environmental factors, and is second only to teeth in this regard. The integrity of the cuticle is damaged by perm, coloring and exposure to sunlight. It is believed that when it is destroyed, the cortical layer is also destroyed, but it can be preserved if the action of the damaging factors stops.
Hair growth phases - why do they exist?
The processes of hair growth and change are cyclical, back in 1926 they were designated as anagen - the period of growth, telogen - the resting phase and catagen - the period of transition from one to another. In the anagen phase (from 2 to 7 years), active hair growth and pigmentation occurs, and the intensity of these processes depends on the condition of the surrounding skin, age and changes in the external environment. Then comes the catagen phase, when hair growth stops, melanocytes lose their activity, the hair follicle sharply decreases in size, and the terminal part of the hair thickens. Next, the hair goes into a resting state - telogen, in which it remains until the development process begins again (on average 3 months). At this point, the hair can be removed with light force, and it falls out on its own when new hair begins to grow underneath it; Normally, a person can lose up to 5-150 hairs per day. The duration of telogen is very variable, it is influenced by the levels of androgens, estrogens, prolactin, ACTH, thyroid hormones, and retinoids. Throughout life, 20-30 hairs can grow from each follicle; under physiological conditions, approximately 70% of hair is in the growth stage, and 10% is in the resting phase. Mechanical removal of conical hair from the telogen follicle always induces anagen and a new hair cycle (this is why hair grows back so quickly after depilation with wax or cream), and even a severely damaged hair follicle has great regeneration potential.
It still remains a mystery why the hair follicle regularly interrupts its growth with the catagen and telogen phases, since this is a very “costly” mechanism. Perhaps this protects the body from possible malignant formations in the actively proliferating hair follicle, or previously made it possible to quickly change the fur coat according to the season. During hair growth, very complex and diverse interactions between cells occur, involving various cytokines and growth factors, which require very precise regulation. The “time sensor” of the hair cycle is autonomous and located in the skin itself, although it can be modulated by various external signals (oxygen, hormones, retinoids), neuropeptides and neurotropins secreted by nerve fibers, etc.
Diffuse alopecia
Physiological telogen hair loss is observed in newborns after 6-8 weeks from birth, in women after 2-4 months. after childbirth, in postpuberty in young girls 16-20 years old and in old age, more often in men (presenile alopecia). With diffuse alopecia, the hair follicles of the head are most often affected, because it is here that 85% of mitotically active anagen follicles, sensitive to damaging factors, are located (in other regions up to 60-90% of follicles in the resting phase).
Various toxic influences or metabolic disorders can cause disruption of hair synthesis and premature completion of the growth phase; 2-4 months after their action, toxic-metabolic telogen effluvium develops. Such processes can be episodic or chronic. The causes of episodic telogen effluvium are most often acute severe infectious diseases occurring with high and recurrent fever (influenza, malaria, infectious mononucleosis, tuberculosis, brucellosis, syphilis), surgical or traumatic shock, collagenosis or medication (thyreostatics, carbamazepine, cimetidine, colchicine , heparin, dicumarol, etc.). Chronic telogen effluvium can develop with iron deficiency (anemia), zinc (with long-term parenteral nutrition), as well as with unbalanced or insufficient nutrition, incl. when treated with fasting or long-term use of reduced diets for weight loss. Chronic alopecia can be a consequence of chronic diseases, primarily endocrine: thyrotoxicosis, hypothyroidism, adrenal insufficiency, hypopituitarism, as well as psoriasis, hepatitis, sarcoidosis, dermatomyositis, encephalitis, leukemia, erythroderma, encephalitis. Strong psycho-emotional stress and stress can also cause alopecia. In rare cases, anagen diffuse alopecia develops - a sudden, diffuse and almost complete loss of hair caused by exposure to drugs, chemical agents or radiation (usually after 1-3 weeks). Typical causes are thallium, mercury, lead, colchicine, antitumor drugs (bleomycin, vincristine, methotrexate, etc.), X-ray irradiation, when a large number of hair follicles in the growth phase are damaged at once. Hair loss caused by chemotherapy is completely reversible.
Androgenetic alopecia
Androgenetic alopecia is a progressive baldness caused by the action of androgens on the hair follicles and occurs in people with a hereditary predisposition. Alopecia is associated with high activity of the enzyme (5-a-reductase), which converts testosterone into its active form - dihydrotestosterone (DHT), its increased content and high sensitivity of hair follicles to this hormone. It is interesting that under the influence of DHT, the terminal hair follicles of the head are degenerated, begin to produce vellus hair, then completely atrophy, and in the vellus hair follicles the opposite process occurs, and hair growth of the face, pubis, and armpits increases with the growth of coarse terminal hair. Hair follicles also contain a 5-a-reductase antagonist, the aromatase enzyme, which converts DHT into testosterone and estrogens. In women, the content of this enzyme in the follicles of the frontal region of the scalp is several times higher than in men, which may be why diffuse androgenetic hair thinning is less pronounced in women.
The disease most often begins after 40-50 years, but can occur at any age after puberty; its frequency depends on ethnic and family factors. Men are more often affected, in whom androgenetic alopecia accounts for about 95% of all cases of hair loss. The hemocapillaries of the papilla of males predisposed to baldness have increased sensitivity to male sex hormones, and when their content increases during puberty, they respond with persistent spasm. There are 5 stages of the disease: first, hair falls out along the anterior border of hair growth (1), then bilateral bald patches form on the forehead and hair thinning on the crown (2), in stages 3-5 there is progressive hair loss with the merging of foci of baldness and complete symmetrical fronto-parietal baldness. In women, this type of alopecia is associated with endocrine disorders, but if there is a genetic predisposition, it can develop without increasing the level of androgens in the blood. Usually this problem occurs between 20-40 years and often causes severe mental trauma. Hair thinning begins in the parietal region, and the frontal strip of 1-3 cm remains unchanged (1), then obvious hair thinning occurs in the parietal region (2), in stage 3 pronounced thinning is detected in the frontal, temporal and lateral areas. Long hair replacement does not involve the lower part of the occipital region, even in the most severe cases and in old age, because follicles that are resistant to the action of dihydrotestosterone are located there.
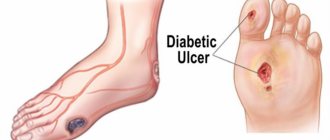
Alopecia areata
Alopecia areata is a chronic dermatosis that is characterized by pathological hair loss and clinically manifested by the formation of circular non-scarring lesions with a complete absence of hair on the scalp, beard area, eyebrows, eyelashes and torso. The frequency of the disease does not depend on gender and race, in 80% of patients the disease occurs before the age of 30, 34-50% of patients get rid of the disease within a year, but almost all patients have more than one episode. The etiology of the disease is unknown, but it is assumed to be of autoimmune origin, since patients exhibit specific changes in cellular immunity parameters, and there is a frequent association with autoimmune diseases. The hair follicle is an immunoprivileged organ (like the eye chambers, brain and chorion), i.e. there is no expression of major histocompatibility complex molecules on the tissue. If immune privilege is violated for any reason, an inflammatory infiltrate of this area occurs, which is a significant factor in the etiopathogenesis of alopecia areata. Zinc deficiency, malabsorption in the small intestine, the presence of cytomegalovirus infection and mental stress are also important.
There are several clinical forms of alopecia areata: 1) local - isolated round lesions, the skin around is not changed; 2) ribbon-shaped - the lesion appears in the occipital region and spreads towards the ears and temples in “ribbons”; 3) subtotal - fusion of small foci; 4) total - no hair on the entire surface of the head (including eyelashes and eyebrows); 5) universal - no hair on the entire surface of the head. During alopecia areata, progressive, stationary and regressive stages are distinguished. In the acute stage, there may be a slight sensation of tingling and burning in the lesion, the skin is swollen, with severe hyperemia, and along the edge of the lesion a zone 0.3-1 cm wide is determined. "loose hair" This hair is dystrophic, split, and can be easily and painlessly removed with gentle pulling. In the stationary stage, skin changes are less pronounced, and the area of “loose hair” is not clearly defined or absent. With regression, vellus hair begins to grow in the area of baldness, which gradually thickens and becomes pigmented. Sometimes already grown hair differs in color from normal hair and has a variegated color - the so-called. poliosis. With syphilis (the eyebrows are affected in the form of small patches), trichotillomania, as well as microsporia of the scalp, trichophytosis and favus, focal hair loss is observed, so a differential diagnosis is made with these diseases.
Alopecia has occurred - how should it be examined?
In addition to a thorough history collection (including family history) and a detailed examination of a patient with alopecia, the doctor must conduct a number of laboratory tests:
Stages of the disease
Alopecia areata goes through 3 stages of development, characterized by certain symptoms. They are reflected in the table.
| Stage | Characteristic |
| Actively progressive | In areas of inflammation, the skin becomes reddish and swollen. A person is bothered by itching, tingling, burning and pain in the area of inflammation. Hair in this area is easy to pull out, even if you pull lightly. Broken hairs can be seen around the lesion. |
| Subacute (inpatient) | It often occurs without pronounced symptoms. In some cases, inflamed lesions appear and disappear very quickly. Their skin is pale or slightly reddish and there are no broken hairs. |
| Regressive | Delicate light growth appears on bald areas of the skin. Gradually it darkens and does not differ from the rest of the hair. |
If there are foci of baldness for more than six months, we can talk about the transition of the disease to the chronic stage.
Will a transplant help?
One way to eliminate alopecia is to transplant hair from healthy areas to the bald area. Transplantation is used only in advanced stages of baldness, when it cannot be dealt with in other ways. If an operation with a skin incision is performed, patients then complain of headaches, which sometimes persist for six months. Scars and scars also remain.
A non-surgical method is hair transplantation using HFE technology. The transplantation is carried out using microscopic needles, which extract healthy follicles, without incisions on the skin, and therefore is minimally invasive. After the procedure, there are no unpleasant symptoms (swelling, pain), no scars remain, and micro-wounds heal within a week. The patient is restored to full volume of hair on his head.
It is recommended that the transplant be performed on men over 40 years of age. At this age, it is possible to understand which follicles will not be affected by testosterone, and they are suitable for transplantation. Otherwise, the transplanted follicles will fall out after some time under the influence of hormones. Doctors do not recommend a transplant for men who have a family history of people who went completely bald before the age of 40.
Alopecia areata can occur in men at any age. But most often it ruins life from 20 to 40 years. If there have been cases of baldness in the family or there is a predisposition to autoimmune diseases, you should take more careful care of your hair on your head in advance. Get a massage, use special shampoos, masks based on folk recipes, eat right, and treat infectious diseases in a timely manner. These simple preventive measures will keep your hair beautiful for a long time.
Principles of treatment for alopecia areata
Treatment of alopecia areata is aimed primarily at eliminating inflammation around the hair follicle, as well as suppressing overactive cells of the immune system, that is, it is anti-inflammatory.
Depending on the severity, activity and extent of the process, anti-inflammatory therapy can be:
- Local - home use of ointments, lotions on skin lesions)
- Injection - injecting areas of hairlessness with corticosteroid drugs
- Systemic – ingestion of drugs that suppress inflammation (immunosuppressants, cytostatics, JAK kinase inhibitors).
- Physiotherapy – using various methods of hardware trichology