Recently, many patients have been asking the same question: “Is surgery on the nasal septum performed using a laser in the clinic?”
Laser radiation in rhinology is used for the purpose of planned non-destructive changes in the shape of cartilage tissue. This method is based on the effect of plastic changes in the shape of cartilage tissue under the influence of high-energy laser radiation, discovered in 1993 by Russian physicist Professor E.N. Sobol and Greek otorhinolaryngologist Professor E. Helidonis.
The method allows:
- give the cartilage a stable arbitrary shape in the absence of destructive, structural changes in the composition of the cartilage,
- has a universal character,
- In principle, it can be used to change the shape of cartilage of any localization.
Laser correction method
The essence of this method formed the basis of the idea of non-invasively changing the shape of deformed cartilage of the nasal septum— laser septochondrocorrection . It was possible to correct deformations of the cartilage of the nasal septum on an outpatient basis, bloodlessly under local anesthesia, thereby improving or restoring nasal breathing .
Advantages of this correction:
- the effect lasts no more than 12-15 minutes,
- well tolerated by patients,
- has a number of advantages in comparison with traditional methods of operations.
A feedback system has been developed, including a special computer program that turns off the laser when the shaping process is completed. This ensures safety and ensures a gentle effect on the tissues of the nasal septum and surrounding structures. to return to active life the very next day after the intervention .
Correction of the nasal septum
The objective difficulties of the recovery stage after septoplasty are one of the reasons for the popularity of alternative correction methods. After surgery, you need to follow numerous rules during the rehabilitation period. For some time, the patient has to endure the symptoms of the early recovery period, including breathing problems, swelling, hematomas, and pain.
Since surgical intervention is accompanied by a violation of tissue integrity, it is impossible to avoid edema even in theory. The doctor takes measures aimed at minimizing congestion during the operation and immediately after its completion. After septoplasty, tampons are installed in the nasal cavity, which prevent increased swelling and perform other important functions.
Tampons, or special silicone inserts (septal splints, rhinological stents), reduce swelling, stop bleeding, prevent mechanical damage to cartilage and bone, have a bactericidal effect and minimize the risk of infectious complications. It is strictly prohibited to remove tampons from the nasal cavity on your own. The doctor removes them on the third or fourth day.
The protective function is performed by a fixing plaster bandage or a plastic splint, which is applied to the middle third of the face. You need to wear the bandage for 7-10 days. Like tampons, only a doctor (ENT or plastic surgeon) can remove the bandage.
After removing the bandage, the face does not look very presentable. Swelling persists, hematomas are clearly visible. To speed up the healing of the ENT, the doctor or surgeon will prescribe anti-inflammatory drugs that have an anti-exudative effect. The doctor will also prescribe antibiotics to prevent infectious complications.
What is required from the patient? First of all, strictly follow the instructions received from the ENT doctor or plastic surgeon. After septoplasty, it is necessary to sleep on your back, otherwise there is a high risk of mechanical damage to the structures of the nasal skeleton.
After septoplasty, wearing glasses is unacceptable. People with poor vision should use contact lenses or temporarily abandon the correction. Subsequently, after the completion of the recovery period, the ban on wearing glasses is lifted.
Thermal procedures increase swelling, thereby slowing down recovery, so you will have to avoid hot baths, saunas and other thermal procedures during recovery. Solarium is contraindicated; sunbathing is prohibited.
Ethanol increases swelling and blocks enzymatic reactions, which are a key part of the regenerative process. Alcohol, as well as smoking, must be completely abandoned during rehabilitation.
Physical activity, especially intense training, is prohibited. Dancing, strength training, cardio training, yoga, fitness and other types of physical activity are contraindicated for a period of up to three months. In the future, you need to avoid playing and contact sports that can lead to injury.
After septoplasty, some specific requirements are relevant, violation of which can lead to complications, including septal perforation, repeated curvature, and abnormal mobility. It is forbidden to blow your nose. You can clean the nasal cavity using soft cotton swabs or rinsing with saline solution. It is strictly forbidden to sneeze with your mouth closed, since a powerful flow of air in the nasal cavity can deform areas of bone and cartilage weakened by surgery.
At the Galaktika clinic (Moscow), septal deformity is corrected using modern surgical and laser techniques. You can get individual recommendations from a specialist and find out the cost of treatment at a consultation with a plastic surgeon.
Application of laser surgical knife
A laser surgical knife is used to gain access to the operating area through the nasal cavity. The laser immediately coagulates the vessels and thereby reduces the risk of bleeding. In addition, laser radiation destroys all microorganisms and bacteria, which ensures the sterility of the intervention and prevents possible infection from the outside.
After using a laser surgical knife, the healing of soft tissues occurs faster, since they are traumatized to a minimum. The low-invasiveness of laser septoplasty helps reduce rehabilitation by approximately half when compared with the use of a traditional scalpel.
The price offered for laser septoplasty in Moscow is quite adequate - in terms of the level of the clinic and the level of training of the surgeon. The difference is explained by the categories of complexity of the surgeon’s work.
Deviated nasal septum and septoplasty
Deviation of the nasal septum (deformation of the nasal septum) and septoplasty (surgical correction of the nasal septum, septum surgery).
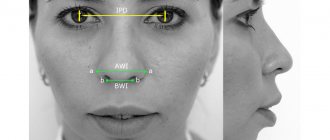
When starting to describe the problem, I try to carefully weigh my words so as not to offend my colleagues and not to cast doubt on the sacred - the most common operation in most of our ENT hospitals and clinics, the implementation of which often literally feeds surgeons, and also ensures the fulfillment of statistical indicators of surgical activity. However, I still have to say that a huge number of such operations are performed without indications - simply in vain. I’ll explain why later; first, let’s deal with the traditional general provisions. The nasal septum (people often say “nasal septum”) is a thin (1-3 mm in different areas) plate, consisting of septal cartilage in the anterior sections and thin bone in the posterior sections. This entire structure is covered with a mucous membrane, which is also very thin. The septum divides the nasal cavity into two halves, making the nose a paired organ. Thanks to the septum, the halves of the nose work harmoniously according to the so-called mechanism. nasal cycle - one half of the nose breathes, the other “rests” at this moment. Between the septum in the middle and the nasal conchas on the sides there is a space called the common nasal meatus. This is where air passes through when you breathe. A deviated nasal septum or enlarged nasal turbinates can narrow this passage, leading to poor breathing. It's simple, simple mechanics. An operation to correct the nasal septum, no matter what it is called, is performed, accordingly, in situations where the septum is deformed. Many studies have been devoted to the effect of a deviated septum on the body. It is believed that these deformations, causing difficulty in nasal breathing, can lead to various disorders due to insufficient aeration of the nasal cavity and reflex influences. At the same time, the frequency of sinusitis (including sinusitis) on the side of the curvature increases, compensatory hypertrophy of the concha develops, hearing may deteriorate due to impaired patency of the auditory tube, the course of acute otitis media is maintained, etc. Pressure of spines and ridges on the mucous membrane the membrane of the nasal cavity can contribute to the development of the neurovegetative form of vasomotor rhinitis, bronchial asthma and other reflex disorders. A small detail - all the described horrors occur only if the septum is so curved that it really makes nasal breathing difficult. And this situation is much rarer than asymptomatic deviated septum. Types of operations.
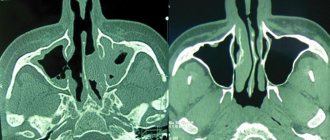
In classical Soviet otorhinolaryngology, the main method of straightening the nasal septum was “submucosal resection of the nasal septum according to Killian.” The name itself explains the essence of the operation - after peeling off the mucous membrane along with the perichondrium and periosteum from the septal skeleton, most of this skeleton was simply removed - resected. As a rule, a narrow strip of cartilage was preserved under the dorsum, not always part of the caudal (anterior) edge of the septum. In the era of operations with head reflectors and Ilyich light bulbs (which, unfortunately, still continues in many hospitals in our cities), the posterior sections of the vomer were often still preserved, simply because the doctor did not see them well during the operation. To remove the ridges of the lowest part of the septum (premaxilla), a chisel and a hammer were usually used, which, under local anesthesia (Novocaine!!!), the patients took very seriously. This is how a terrible fairy tale about leveling a partition with hammers was born among the people. If it were not for this frightening stereotype, then we probably would not have people left with unoperated septums. The sheets of the mucous membrane hung in the form of a curtain in the middle position and were brought together by tampons. That's all. By the way, gauze swabs, the length of which, according to classical requirements, should have been at least half a meter, were poorly tolerated by patients and gave rise to another popular horror story, firmly associated with this operation. As a result, at best, the septum became smooth, but thin, weak, floating, and often stuck to one of the halves of the nose when breathing. The absence of a cartilaginous framework often led to the formation of perforations or cosmetic defects - retraction of the columella, drooping of the nasal tip or saddle-shaped deformity of the dorsum. A more modern method is septoplasty, which is a collective concept. Traditionally, the difference between septoplasty and submucosal resection is considered to be the preservation of intact uncurved sections of cartilage or reimplantation (returning to place) of aligned fragments. However, each doctor puts his own vision into this name. At one time, the concept of leveling the septal cartilage using special notches was quite popular, but few surgeons today conduct experiments with the biomechanics of cartilage - unfortunately, it is not always possible to predictably change its shape. Some ENT doctors, trying to keep up with modern terms, changed their minds and began performing “septoplasty” on patients, performing the same submucosal resection of the nasal septum that they learned 30 years ago. Endoscopic septoplasty is often of interest to patients [video, photo]. This is simply the name for septoplasty performed under endoscopic guidance. But the standard technique is inconvenient to operate with an endoscope, so the method has its own characteristics - as a rule, an incision in the mucous membrane is made at the site of the curvature and then not sutured. It should be remembered that endoscopic septoplasty is only suitable for certain types of curvatures, as a rule, these are isolated spines of the nasal septum, ridges starting deeper than the caudal edge, the so-called. “bumps” of the septum in its upper sections. In these cases, this technique has undoubted advantages, but one must understand that the advantages here are not greater efficiency, but less trauma and an easier postoperative period. A septum that is curved along its entire length or with deformation in the anterior section is more difficult to operate endoscopically and there is little point in doing so. I sometimes do this to maintain my endoscopic skills. For several years, the community of patients was stirred up by one of the “Health” programs, and people actively began to look for where to straighten the nasal septum with a “laser” and without “surgery.” In response, they usually see a smile on the faces of the surgeons and a desire not to believe the fairy tales. But these are not fairy tales and indeed, such a method exists. We are talking about the so-called laser septochondrocorrection. The essence of the intervention is to “warm up” the nasal septum with a special laser, which leads to temporary softening of the cartilage, which, simultaneously with heating, is pressed with a special instrument and the curvature is reduced. If the patient is selected correctly, there will be an effect. The only problem is that rare individual types of curvature are suitable for this technique - it must be a smooth bend in the cartilaginous section. That's all. In the vast majority of patients, the nature of the deformity is not suitable for elimination by this method. Moreover, probably only the authors of the technique have equipment for laser septochondrocorrection, although other surgeons do not particularly try to acquire it. Very interesting insight into septoplasty and deviated septum by many unqualified plastic surgeons. Sometimes it seems that they simply do not know that this anatomical formation continues deep into the nose for a good 10 centimeters. In their view, the nasal septum is its skin part (collumella) and the caudal (anterior) parts of the septal cartilage. Accordingly, the correction of the septum in their implementation is limited to intervention in these sections, while significant deformations in the posterior sections, powerful spines and sharp ridges remain intact. The most annoying thing is that patients are sure that their septum was corrected. Septoplasty in one stage with rhinoplasty is becoming increasingly popular. And this is absolutely justified. When the external nose is deformed, especially with scoliosis, one-stage rhinoplasty improves the functional result of septoplasty, and vice versa, with proper rhinoplasty, it is most often necessary to correct the nasal septum. So, if you are faced with two problems - an ugly nose and a crooked septum - do not hesitate and look for a surgeon who will fix it for you during one operation. Septoplasty for cartilage harvesting. Sometimes it is necessary to perform intervention on the septum in the absence of functional indications. The fact is that the nasal septum is deservedly considered the best source of cartilage, which we often need during rhinoplasty, and less often during sinus surgery. Such an intervention consists of peeling off the mucous membrane and taking a cartilaginous fragment. It is important to take cartilage only where it does not have a supporting function - usually these are the posterior-inferior sections. Typically, the intervention takes a few minutes, is accompanied by minor surgical trauma and does not complicate the postoperative period. Open access septoplasty is common in some Western clinics. Only a few of us do it. The technique consists of a preliminary open rhinoplasty approach, through which the surgeon then gets to the septum. If we are only talking about correction of the nasal septum, then this approach does not make sense at all - the operation time and surgical trauma increase. It’s another matter if rhinoplasty is also performed or the nasal valve is corrected. Then this approach is justified. Single-stage septoplasty with sinusotomy. When a deviated nasal septum is combined with pathology of the paranasal sinuses, it is imperative to eliminate both. As a rule, the septum is operated on first; this, among other things, facilitates endoscopic access to the sinuses. A sinusotomy is then performed. Previously, surgeons had some doubts about whether it was worth operating on the septum for purulent sinusitis; this was somewhat contrary to the rules of asepsis. However, a huge number of observations - foreign, domestic, and our own - have shown that fears are unnecessary. I have never in my practice encountered any purulent-inflammatory processes in the operated septum that arose due to the fact that the sinuses were operated on in one stage. You should not be afraid of a more difficult postoperative period. As a rule, if operations are performed correctly, the condition of patients after surgery is the same as with isolated interventions only on the sinuses or only on the septum. One-stage septoplasty with correction of the nasal turbinates. Reduction of the nasal turbinates is a mandatory option, usually performed at the end of the intervention on the septum. Moreover, this stage of the operation, small in time and volume, often affects nasal breathing much more than the actual correction of the septum. Especially if there were no clear indications for septoplasty. There is even a joke among otolaryngologists that “the key to successful septoplasty is good correction of the nasal turbinates.” We will talk about operations on shells in a separate article. Indications for septoplasty. The most controversial issue, I already mentioned this at the beginning. I am sure that most operations on the nasal septum could not have been done. Nothing in the patients' lives would change. Data that have emerged in recent decades about the possible (no one has proven unequivocally) influence of local curvatures of the nasal septum in the form of spikes and ridges on the development of sinusitis [picture] has further encouraged otorhinolaryngologists to operate on septums that do not cause nasal breathing problems. Of course, such situations do occur, but in reality they are so rare that we show such patients to residents and students. If you are in doubt whether to correct the septum or not, it is most likely useless to seek the truth from other doctors - you probably have some degree of curvature and it is unlikely that any of your fellow otolaryngologists will dare to say that surgery is not necessary. I believe that most likely you do not need to have septoplasty if there are no problems with nasal breathing or you do not suffer from chronic sinusitis. If the deformation of the nasal septum did not cause complaints, but was detected during examination by an otolaryngologist or on a computer tomogram, it is simply an anatomical feature without clinical manifestations. You should not follow the lead of a surgeon or radiologist. And all the explanations about how someday this will lead to health problems are just children's horror stories. When it does, then you will perform the operation. And most likely it won’t, if it hasn’t already. This is confirmed by the huge number of patients with crooked septums and a complete absence of rhinological problems, whom we see during preventive examinations. An issue that deserves special mention is diagnosing a deviated nasal septum using computed tomograms.
Deviated nasal septum causing sinusitis
Radiologists (don't be offended) want to look like doctors too. And if a competent radiation diagnostician only describes the condition of the nasal septum, then the self-affirming doctor will categorically make the diagnosis “deviated nasal septum”, and will also comment on this to the patient in words. In this case, the most important medical rule is forgotten - the diagnosis is made only by a clinician, using, among other things, the results of additional research methods, including computed tomography. And patients most often do not know about this rule at all. And the conclusion based on the results of a computed tomography scan is like the ultimate truth for them. Well, what a cool modern method. And many ENT doctors don’t even try to argue - “since a curvature was detected on the tomogram, then we definitely need to do it!” Therefore, the widespread introduction of computed tomography has significantly increased the number of unnecessary operations in the nasal cavity. It also increased the number of people dissatisfied with the results of treatment. The fact is that the main focus of the operation is on those parts of the septum that are clinically significant, that is, they affect breathing. At the same time, there are sections that do not affect aerodynamics in any way, and correcting them is not only unnecessary, but sometimes dangerous and increases the risk of complications. Conservative surgeons, as a rule, do not touch these areas. And on tomographic sections at this level, it is clear that the deformation has been preserved. This is concluded and given to the patient, causing understandable indignation and complaints against the surgeon. Any explanations from the doctor will be regarded as excuses. This computer dictate forces surgeons not only to change approaches to diagnosis, but also to change intervention techniques. During an operation, I often catch myself thinking that I am performing those stages of the operation that I could have done without and operating more invasively, only so that later the radiologist does not write in the CT report about a deviated nasal septum, I just don’t want to explain to a perplexed patient why did this happen? Postoperative nasal tamponade. Traditional tactics for correction of the nasal septum included mandatory postoperative nasal tamponade. Tamponade had 2 goals: 1) to bring together the separated layers of the mucous membrane and perichondrium, preventing bleeding and hematoma formation; 2) fix the septum along the midline for the first time. In the era of submucosal resections it was impossible to do otherwise. They were tamponed with a long turunda at the end of the operation under local anesthesia, when the effect of novocaine had already worn off. It is clear that this moment was the most painful for the patient and was etched in his memory for a long time. The tampon burst the inside of the nose, causing pain in the nose and headache, while it was necessary to breathe through the mouth. Different clinics used different periods of tamponade, from one day to five, usually two. Removal of the gauze swab was accompanied by the appearance of a new wound surface on the mucous membrane and bleeding. All this added negative emotions to the patient and made septum correction one of the most “scary” operations. The change in surgical technique also led to a change in postoperative tactics. So-called “finger” tampons, made of rubber gloves filled with a sponge, began to be introduced everywhere. These tampons are easier to carry and are very easy to remove. The duration of tamponade in most departments was reduced to a day; it turned out that this was sufficient and did not increase the percentage of hematomas and bleeding. The understanding has come that if the septum is not reliably straightened during the operation, then no long-term tamponade will then give it a median position. Later, various tampons made from materials that expand when moistened began to appear on the market. Some of these tampons have breathing tubes. Other modern tampons are a sponge that does not require removal, it gradually softens and decomposes inside the nose and gradually comes out when you blow your nose. All this made the postoperative period significantly easier. Then the surgeons went further and began to refuse packing altogether. Several studies have appeared showing that the result of surgery without tampons is no worse, there are no more complications, and the patient’s well-being, of course, is better. Tampon-free management remains a controversial issue; most surgeons are not yet ready to accept such innovations. The technique of the operation is of great importance. If the intervention ends with suturing the septum using a special technique, then these sutures strengthen the septal frame, fix the septum in the midline and bring the layers of the mucous membrane together, preventing hematoma. This technique usually does not require tamponade. When correcting the anterior and middle sections of the septum, I actively use transseptal sutures and try, if possible, to do without tamponade. It is usually still necessary to pack the nose with “fingers” or a sponge if a one-stage “cold” correction of the nasal turbinates is performed and we see that there is a risk of bleeding from the turbinates. If the shells are reduced by any physical methods, then tampons are not needed at all. Another progressive method is “splinting” the septum. Today on the market there are several modifications of intranasal splints or, as they are also called, “splints” - thin soft silicone plates that are inserted into the nasal cavity after surgery and stitched together through the septum. The purpose of splinting is to stabilize the operated septum, prevent hematoma, protect the mucous membrane, prevent contact of the nasal septum and turbinates to prevent synechiae. As a rule, splinting helps to obtain a good result of the operation, but there are also disadvantages. The most important of them is that the splints must be removed, and this is an additional sensitive, albeit small, manipulation in the patient’s nose. I don’t see much point in the routine use of splints, but I am happy to use them in certain cases, for example, during complete reconstruction of a destroyed septum, during septoplasty performed simultaneously with the elimination of scoliosis of the external nose, as well as with injured or atrophic mucous membrane of the septum. Postoperative management. After removing tampons in hospitals, the patient is invited daily to the dressing room, turundas and cotton wool with various medications are inserted, mucus is sucked out, and crusts are removed. It is necessary to somehow justify the patient’s week-long stay in the hospital. And train residents. Despite the fact that it is not easy to ensure absolute sterility of instruments and good antiseptics in dressing rooms and ENT examination rooms. As a rule, there are not many tools. It often happens that the sinuses are washed with the same cannula for purulent sinusitis, and then, after a quick treatment, the nose is cleaned after septoplasty. I also used to be active in the postoperative period. Then I began to notice that the less you manipulate the patient’s nose after surgery, the faster and easier it heals. The fact is that normal healing of the mucous membrane occurs with the formation of fibrin plaque, under which a new epithelium is formed. In addition, the fibrin crust “pad” prevents contact with wound surfaces and prevents synechiae. Removing this plaque interrupts the normal healing process. Each intranasal manipulation injures and infects the mucous membrane, is unpleasant for the patient, and lengthens the postoperative period. It is optimal to prescribe anti-inflammatory and healing drops and ointments in the postoperative period, as well as regular follow-up examinations for the timely detection of hematoma or synechiae. And the removal of fibrin, plaque and crusts is only sometimes, with complete obstruction, to give the patient the opportunity to breathe through the nose. Or to take a good look at the septum if a hematoma is suspected. Duration of hospitalization. “Maintenance” of bed days after septoplasty in our ENT hospitals is usually intended to correct hospital statistics and meet the standards of insurance companies. If the operation is performed non-traumatically and the patient does not have severe concomitant somatic diseases, then he can be sent home the next day after the operation if there is no bleeding. At least that's how they do it all over the world. Only the doctor must be sure that the patient will strictly follow the prescriptions and instructions in the postoperative period. Prescribing antibiotics. Surgeries in the nasal cavity are classified as “conditionally clean”, that is, it is almost impossible to ensure the sterility of the surgical field and the wound is always contaminated with bacteria, which inevitably increases tissue inflammation in the postoperative period. To avoid this, the gold standard today is perioperative antibacterial prophylaxis, the essence of which is a single administration of a broad-spectrum antibiotic intramuscularly immediately before surgery or intravenously during the intervention. In the standard case, this is sufficient and a course of antibiotics after surgery is not required. Age for septoplasty [link to video about pediatric septoplasty]. The earliest. Previously, it was believed that it was necessary to operate on the septum only when the nose had finished growing. Much has been written about the so-called “growth zones” of the septal cartilage, damage to which during surgery can lead to cessation of growth of the external nose. Taking into account the then dominant technique - submucosal resection of the septal cartilage, this was justified. With the introduction of more gentle and tissue-preserving methods of surgery, the age limit has been lowered and many people report successful performance of this operation in children at 10, 7 and even 5 years old. The only problem is that it is very difficult to assess whether the operation affected the development of the external nose: firstly, very long periods of observation are needed, and secondly, no one knows what shape the nose would have had without the operation. Rare case reports of twins, one of whom had septal surgery as a child, show conflicting results. What I can say for sure is that the effectiveness of surgery in children is lower, especially in terms of long-term results. I've seen many such examples. A straight postoperative septum in a 10-year-old child very often becomes bent again by the age of 12-13 - this is due to the continued growth of cartilage and bones. Therefore, the indications for pediatric septoplasty must be narrowed and parents properly informed. I only perform surgery on small children if the septum is so deformed that it causes complete obstruction or sleep apnea. This doesn't happen often. Another rare indication is if a deviated septum begins to “pull” the growing external nose to the side and over time an aesthetic problem may also form. In any case, parents should be warned that there is a high probability of repeated surgery in the future, even if the surgeon is very qualified. The latest age. If there are indications and there are no serious somatic diseases, it is not limited. Only the readings must be well analyzed. Typically, a deviated nasal septum manifests itself between the ages of 20 and 40. At a later age, you need to think carefully; most likely, difficulty in nasal breathing is due to other reasons - for example, an enlargement of the nasal turbinates or a weakening of the nasal valve. Preparing for surgery. Standard preparation includes preoperative examination and exclusion of alcoholic beverages and aspirin-containing medications from the diet. No other special arrangements are usually required. However, you cannot give recommendations that contradict the guidelines of the surgeon you have chosen, so I will simply say - ask your doctor about the training. Choice of anesthesia. Previously, the vast majority of operations on the nasal septum in our country were performed under local anesthesia. Abroad - only under anesthesia. Today, with the modern development of anesthesiology and the presence of a good anesthesiologist, it is preferable to perform operations under anesthesia. This is more comfortable for both the patient and the surgeon. However, in adults, local anesthesia (the so-called “freezing”) is also acceptable. Modern local anesthetics are strong and long-lasting, the operation in a standard case takes no more than 30 minutes, and if the patient is psychologically balanced, then why not. Usually, the first communication with the patient, his reaction to the examination and diagnostic manipulations helps an experienced doctor understand who should not be offered local anesthesia. Complications. Complications during and after nasal septum surgery can be divided into groups. 1. Complications during the operation: fainting during local anesthesia and at the beginning of the operation; cases of blindness that developed during anesthesia before surgery have been described; bleeding that occurs during detachment of the mucous membrane, as well as after resection of the deformed part of the nasal septum; perforation of the nasal septum, which can occur both at the very beginning of surgery and during subsequent stages. 2. Complications in the immediate postoperative period: septal hematoma, which can develop in the first days after surgery, fester and turn into an abscess; swelling of the mucous membrane at the mouth of the auditory tube, sometimes developing as a result of nasal tamponade, which usually leads to the development of acute otitis media; inflammation of the orbit, intracranial complications or septic conditions, which, fortunately, develop very rarely. 3. Late complications: deformation of the nose (drooping of the tip or retraction of the back), atrophic rhinitis, late perforation of the septum as a result of atrophy, synechia of the septum with the lateral wall of the nose, flotation of the septum and return of the perichondrium to its previous position. All of the horror stories listed above happen, of course, rarely. The most discussed long-term consequences of septoplasty are, of course, saddle-shaped deformation of the external nose due to loss of rigidity of the cartilaginous dorsum and perforation of the nasal septum. Postoperative saddle deformity is most often the result of too high resection of the septal cartilage or destruction of connections in the so-called key areas: septospinal and in the upper parts of the connection of the cartilage with the vomer. Usually this problem appears immediately after the intervention, but sometimes postoperative tissue swelling “holds” the back for some time, and then it gradually lowers. Preservation or restoration of key connections is essential to prevent this deformation. Well, if possible, return the cartilage to the septum. I remember that earlier otolaryngologists did not know how to eliminate such deformities and each such case was a surgical disaster. Hence - a large number of operated septa with preservation of deformation in the upper sections. Surgeons were afraid of saddle-shaped retraction like fire and did not cut the cartilage high, believing that it was better not to let the nose completely suffocate than to have a cosmetic defect. Today the problem seems not so terrible - the profile of the back is restored during a small and uncomplicated rhinoplasty. We present an example of postoperative saddle deformity and the result of its correction.
Elimination of saddle deformity
Postoperative perforation of the nasal septum is another headache for surgeons. Many surgeons hate to say this, but it happens most often, of course, with unsutured ruptures of the mucous membrane on both sides at the same level. A long time ago, when I was taught to do Killian’s operation, experienced doctors did not advise trying to sew up tears - “you’ll tear it even more,” and if a perforation formed, they recommended widening it, “so that your nose wouldn’t whistle later.” This unspoken tactic was adopted, I don’t know why. Maybe there weren’t good tools, light or suture material back then. It turned out that mastering the technique of intranasal suturing of the mucous membrane is not difficult and most of the ruptures can be repaired quite easily today. Fortunately, postoperative perforations of the nasal septum most often have well-epithelialized edges and are located in the middle sections, without creating serious problems for the patient. If necessary, small and medium-sized perforations are closed surgically.
Result of plastic closure of perforation of the nasal septum
Less frequently, perforations do occur that are not related to the surgical technique, but to local or systemic tissue trophic disorders, for example, with atrophic rhinitis or diabetes mellitus. Such holes can form in the immediate postoperative period, even if everything went smoothly during the operation. Therefore, it is so important to carefully consider the indications for surgery in somatically burdened patients. Repeated (revision) septoplasty. Considering that a large number of secondary and residual deformities are detected in the population, especially in patients previously operated on by Killian, repeat septoplasty is performed quite often. According to my observations, most often the ineffectiveness of the previous operation is associated with two mechanisms: 1) persistence of deformation in the anterior-superior parts of the septum, at the level of the nasal valve. This area is often left “aside” from the surgeon’s main work, or the doctor is afraid to resect the cartilage high so as not to cause secondary deformation. Sometimes the cartilage fragment in this area “springs” and bends to one side, closing the nasal valve. 2) another reason for ineffectiveness is ridges and deformations in the lower and posterior parts of the septum. As a rule, they were simply not reached during the first operation. It is very difficult to perform revision septoplasty using the classical method - after all, for this it is necessary to separate the layers of perichondrium that have grown together and are welded together by scar tissue, often in the absence of cartilage between them. But it is not worth operating according to the classical method for repeated operations. It is faster, more convenient and more effective to perform separate small approaches in the projection of unresolved deformities. Even if there are several such cuts. Then most of the septum remains intact, and the operation becomes very effective. An endoscope is of great help with this technique. So patients with difficult memories and ineffectiveness of the first operation should not be afraid of revision - today it is a completely different story and the difference in sensations and results will be obvious.
Contraindications for septoplasty
There are few contraindications for surgery to correct the nasal septum. This operation cannot be performed:
- Pregnant;
- Nursing mothers;
- Suffering from diabetes;
- Under the age of 16–18 years;
- If you have cancer;
- In some other special cases or at the doctor's discretion.
But even the presence of contraindications does not mean that everything is lost - in this case, the doctor can simply prescribe laser correction.
Causes of curvature
In clinical practice, congenital or post-traumatic curvature of the nasal septum is most often encountered. In the first case, the cause of the deformation is a violation of the uniformity of development of various parts of the facial skeleton during the growth of the body. The defect appears at a young age, but for a long time it may not be accompanied by clinical manifestations (nasal congestion, impaired nasal breathing, other symptoms).
Post-traumatic deformities of the nasal septum are a consequence of facial trauma received during sports competitions or training, road accidents, at home, and at work. Very often, such curvatures are more pronounced and immediately manifest themselves as clinical symptoms. As a rule, the patient has an external deformation of the nose (flatness, asymmetry), which also requires surgical correction.
Less commonly, the cause of a pathological change in the septum is a disease, for example, a tumor of the epithelial tissues of the nasal cavity. The neoplasm itself leads to disruption of nasal breathing; in addition, it puts pressure on the cartilage of the nose, provoking their deformation.
Postoperative period
Restoring the body and appearance takes some time. Swelling usually goes away after a few days. Hematomas persist a little longer. To prevent complications, after laser rhinoplasty you must follow your doctor’s recommendations:
- reduce physical activity;
- sleep only on your back;
- protect the nose from damage;
- exclude sauna and smoking.
You can evaluate the results after 3 months, when complete healing occurs. The duration of rehabilitation is also influenced by the patient’s age, body characteristics, and compliance with recommendations.
Indications for laser rhinoplasty
The main indication for surgery is psychological discomfort associated with the presence of cosmetic defects of the nose. Aesthetic correction is recommended after the age of 20, when cartilage tissue stops growing.
Surgical intervention can correct the following deficiencies:
- crook in the nose;
- disproportionate shape, width of the nostrils;
- asymmetry, curvature of the nose;
- deformation after illness, injury;
- massive, drooping, bent or upturned tip of the nose;
- saddle back;
- birth defects.
Since laser energy softens cartilage tissue, it is possible to model any nose shape that matches the patient’s idea of a harmonious facial image (if this does not contradict common sense).
For medical reasons, rhinoplasty is performed to restore the nose after injury or disease. Surgery is necessary for respiratory dysfunction associated with the growth of cartilage and thickening of the mucous membrane of the internal turbinates of the nose.
Complications after laser septoplasty
- In some cases, after correction of the nasal septum with a laser, the following may occur:
- inflammatory process in the nasal cavity;
- formation of subcutaneous hematomas;
- burn of the nasal mucosa;
- formation of scars and scars.
The result of laser septoplasty, like any other method of nasal septum correction, largely depends on the skill and experience of the plastic surgeon. Plastic surgeons at our clinic prefer to solve the problem of deformation of the nasal septum using proven methods. Septoplasty requires extensive knowledge in ENT surgery, as well as sufficient experience in carrying out this type of correction.
We strongly recommend that in case of disturbances and impossibility of nasal breathing, you immediately take measures - seek help from qualified specialists.
Septoplasty is the surgical correction of a deviated nasal septum with its reconstruction.
Synonyms: submucosal resection of the nasal septum, correction of the nasal septum.
Surgery on the nasal septum is performed to restore the physiological shape of the nasal septum, normalize breathing through the nose, and eliminate factors that contribute to impaired ventilation of the paranasal sinuses and middle ear.
Indications for surgery:
- deviated nasal septum with impaired nasal breathing through one or both halves of the nose;
- deviated nasal septum in combination with chronic or recurrent (recurring) sinusitis or otitis media;
- deviated nasal septum in combination with chronic dacryocystitis, impaired outflow of tear fluid;
- deformations of individual parts of the nasal septum, complicating intranasal surgical access to the paranasal sinuses, base of the skull and lacrimal sac.
The deformity itself, accidentally discovered, is usually not an indication for surgery. However, if a young man without complaints of difficult nasal breathing is diagnosed with a sharp curvature of the nasal septum, then it is better to perform an operation for preventive purposes, since over time, pathological nasal breathing will inevitably lead to the formation of complications in the form of chronic inflammatory diseases of the upper or lower respiratory tract, middle ear, development of snoring, obstructive sleep apnea syndrome, etc.
Contraindications
There are no absolute contraindications. Relative (temporary) contraindications include old age, pregnancy, blood coagulation disorders, arterial hypertension, acute respiratory and other infections.
With concomitant seasonal (intermittent) allergic rhinitis, septoplasty is contraindicated during the dusting season of plants that cause allergic rhinitis.
Preparing for surgery
A standard scope of examination is required as for any planned operation: clinical, biochemical blood tests, hemostasis study, consultation with a therapist, anesthesiologist (place a list). It is advisable to perform a computed tomography scan of the nasal cavity and paranasal sinuses, which, firstly, allows you to obtain more complete information about the shape of the nasal septum and the geometric relationships in the nasal cavity, and secondly, to identify concomitant diseases (chronic sinusitis, paranasal sinus cysts) that may be cured with a one-stage operation.
Anesthesia. Septoplasty can be performed under general anesthesia or local anesthesia.
To visualize the surgical field, a headlight or endoscopic control is used.
There are several methods and many varieties of techniques for correcting the nasal septum. The surgeon chooses the most appropriate surgical method depending on the nature of the existing deformity.
Septoplasty technique
An incision is made in the mucous membrane inside the nose and the mucous membrane is peeled off from the osteochondral frame of the nasal septum on both sides. Then the curved cartilaginous and bone sections of the nasal septum skeleton are removed, they are straightened using a special press and reimplanted to preserve the supporting function of the nasal septum and prevent the development of perforation. The intervention is usually performed with miniature instruments, without the use of a hammer or chisels. The operation is completed by applying through sutures to the nasal septum and to the incision line. After such an operation, nasal packing is usually not required. If correction of the nasal turbinates is performed simultaneously, elastic tampons with air tubes are inserted, making it possible to breathe through the nose after the operation for a period of one day. Removing tampons is almost painless. Nasal breathing after surgery is restored gradually within an average of two weeks. This is due to swelling of the mucous membrane and the formation of crusts in the nasal cavity in the postoperative period.
Technique of endoscopic surgical interventions on the nasal septum
Non-traumatic deformities of the nasal septum are usually represented by spines, ridges, local curvatures or thickening of the nasal septum and can be easily eliminated by minimally invasive endoscopic intervention. In this case, careful submucosal removal of the curved fragment of the nasal septum skeleton is performed, followed by reimplantation of the straightened fragments of cartilage and bone or without it.
In some cases, endoscopic septoplasty can also be used for repeated interventions on the nasal septum. At the end of the operation, the mucosal flaps are fixed by introducing several pieces of a hemostatic sponge or a small elastic tampon.
If there are several local deformations of the nasal septum (ridges, spines and thickenings), various intervention options can be performed simultaneously.
Endoscopic shaver septoplasty
Endoscopic shaver septoplasty (Powered Endoscopic Nasal Septum Surgery) uses a shaver/microdebrider, which can be used to “shave” the cartilaginous and bony protrusions on the nasal septum, including the premaxillary ridges. This reduces the operation time, makes it less traumatic, and allows you to avoid using a chisel and hammer.
Laser septochondrocorrection
This method is based on the ability of cartilage tissue to change its shape under the influence of high-energy laser radiation. It can be performed on an outpatient basis and is virtually bloodless. The method has very narrow indications: only small C-shaped curvatures in the anterior (cartilaginous) part of the nasal septum; such cases account for less than 10% of all types of deformities. Laser septochondrocorrection often leads to the formation of secondary deformations and perforation.
Repeated operations on the nasal septum (reseptoplasty)
Repeated operations on the nasal septum are technically complex and require extensive surgeon experience. A feature of repeated operations is the absence of part of the skeleton of the nasal septum (cartilaginous and/or bone). In these places, the opposite layers of the mucous membrane grow together to form scars. This creates technical difficulties when peeling off the mucous membrane. Scars are cut sharply. Sutures made of absorbable material are placed at the edges of mucosal ruptures (if they occurred during the intervention). The curved fragments of the cartilaginous and/or bone skeleton left by the previous surgeon are removed, aligned using a press and, as during the primary operation, inserted into place between the layers of the mucous membrane to preserve the supporting function of the nasal septum and prevent the development of perforation. Silicone plates (splints) are sewn to the nasal septum with through sutures to protect the mucous membrane. They are usually removed painlessly a few days after surgery. For repeated operations on the nasal septum, endoscopic techniques can also be used.
Postoperative period
It consists of cleaning the nasal cavity from blood and fibrin clots and crusts, which is done by the doctor in the first days after the operation, and in irrigating the nasal mucosa with a 0.9% sodium chloride solution by the patient himself.
For 3 weeks after surgery, it is recommended to avoid physical activity, air travel, sudden climate changes, hypothermia, overheating (bath, sauna).
Possible complications. Surgeries on the nasal septum are relatively safe and are rarely accompanied by complications. The most common complication of operations on the nasal septum is the formation of perforation (hole). With excessive removal of cartilage in the upper sections, subsidence of the nasal dorsum is possible, the so-called saddle nose deformity.
PHOTO GALLERY:
| Right nasal septum ridge | Endoscopic resection of the nasal septum ridge |
| Correction of subluxation of the caudal edge of the cartilage of the nasal septum allows you to restore the normal shape of the nasal valve and improve nasal breathing (1st day after surgery) | Correction of the cartilaginous part of the nasal septum in some cases leads to an improvement in the shape of the nose (1st day after surgery) |
| Septoplasty using a head light | |
| A patient with difficulty in nasal breathing and recurrent right-sided maxillary sinusitis. Septoplasty was performed with correction of subluxation of the caudal edge of the cartilage of the nasal septum (1st day after surgery) and endoscopic surgery on the right maxillary sinus: the block of the natural sinus anastomosis was removed, it was combined with an additional anastomosis. — 1 photo | Preoperative computed tomography of the paranasal sinuses – 2 photos |
Contraindications
Contraindications to aesthetic correction are divided into absolute and relative. Absolute contraindications include:
- chronic infections;
- severe cardiovascular diseases;
- autoimmune processes;
- oncological diseases;
- immunodeficiency states;
- diabetes;
- impaired blood clotting;
- respiratory failure;
- pregnancy;
- dysmorphophobia - an imaginary cosmetic defect, exaggerated due to the patient’s unhealthy mental state.
Laser rhinoplasty is relatively contraindicated in the following cases:
- local purulent inflammation;
- acute sinusitis;
- current diseases.
The operation is carried out after appropriate treatment and restoration of the body. If there are age restrictions (up to 18 years and over 50 years), surgery can only be performed for medical reasons.