The essence of reduction mammoplastyAfter surgeryContraindicationsSurgery techniqueMethodsRehabilitation
IndicationsAdvantagesFeedback from our clientsQ&A Who should I sign up for?Prices
The DOCTORPLASTIK clinic performs operations to correct large female breasts. Reduction mammoplasty is an operation to reduce the mammary glands while simultaneously tightening and improving the shape. Most often, such an intervention is carried out due to medical recommendations, as well as the patient’s dissatisfaction with the large volume of the breast.
Large breasts are not only a cause of psychological discomfort. It also causes physical discomfort, which can lead to health problems over time. Women with large breasts often suffer from pain in the thoracic and cervical spine. They find it difficult to choose bra and clothing sizes. There are also certain inconveniences when playing sports. However, there is a solution to this problem: our clinic in Moscow offers breast reduction surgery at an affordable cost.
All photos of breast reduction
The essence of reduction mammoplasty
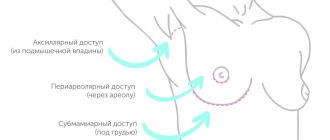
Surgery for breast reduction involves removing excess glandular breast tissue and subcutaneous fat. The nipple-areola complex is moved to a higher position.
Prices
| Professor I.V. Sergeev | Plastic surgeons | |
| Areola correction | 162 000 | |
| Breast reduction with vertical scar | 350 000 | 150 000 |
| Breast reduction with T-scar | ||
| 1 category | 445 000 | 300 000 |
| 2 categories | 499 000 | 350 000 |
| 3 categories | 554 000 |
Types of mastopexy
There are several types of mastopexy. During the consultation, after examination and conversation, the plastic surgeon offers you the lift option that he considers most effective in your case.
Mastopexy can be:
- periareolar (circular)
- vertical
- anchor (T-shaped cut)
- dermal
- endoscopic
All of them, as I said above, do not involve prosthetics. However, a combination of procedures is possible.
Today I will not talk in detail about each technique. This will be the subject of my next article.
Contraindications to breast reduction:
- severe pathologies of internal organs;
- diabetes;
- bleeding disorders;
- incomplete lactation;
- infectious and oncological diseases.
Reduction mammoplasty is not performed on persons under 18 years of age. It is not recommended for women planning pregnancy (as problems with lactation may occur).
Breast reduction: surgical technique
After a comprehensive examination and consultation with a mammologist, surgical tactics are developed to achieve the required result.
The main goal of reduction surgery is tissue resection to improve the shape and reduce the volume of the breast. The manipulation is performed under general anesthesia. Regardless of the chosen tactics, it includes the following steps:
- formation of surgical access;
- excision of excess skin and glandular tissue;
- movement (up) of the nipple-areolar complex while maintaining its trophism and innervation;
- installation of drains;
- suturing.
Need a consultation?
How to prepare for surgery?
Preoperative preparation for surgery includes a set of clinical and diagnostic measures, during which the patient’s general health condition and the absence of contraindications to the operation are assessed.
- Clinical and biochemical blood test.
- General urine analysis.
- Determination of blood group and Rh factor, coagulogram.
- Testing blood for antibodies to HIV, syphilis, viral hepatitis.
- Fluorography.
- Electrocardiography.
- Mammography, ultrasound of the mammary glands.
- Consultation with a mammologist-oncologist, therapist, anesthesiologist.
2-3 weeks before surgery, it is prohibited to take medications without a doctor’s prescription (especially hormonal drugs and blood thinning medications: Aspirin, Heparin), sunbathe, smoke and drink alcohol.
The operation is performed on an empty stomach, so the last meal in the form of a light dinner is allowed the night before.
Breast reduction techniques
Reduction mammoplasty is performed in two ways:
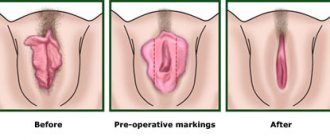
- with an anchor incision (in the shape of the letter “T”): with this surgical approach, you can achieve a dramatic reduction in breast size - to remove a large amount of tissue, an incision is made in the inframammary fold, then it goes up to and around the areola;
- with a vertical incision, shortened scar technique (M. Lejour method): used to excise a small amount of tissue, is less traumatic, after the operation there remains an invisible scar around the nipple and a scar going down to the inframammary fold.
Breast reduction surgery is performed under general anesthesia and lasts 1.5–2 hours. After surgery, the woman is in the hospital under medical supervision for 1 day.
Reduction mammoplasty surgery: introduction
The word reduction
(Latin reductio - retraction, return, restoration) in medicine means reduction, reduction. That is, reduction mammoplasty is an operation to reduce the volume of the mammary glands (MG). For the aesthetic surgeon performing this operation, it is important not only to achieve the desired reduction in breast volume, but also to create a new, beautiful breast shape with a correctly positioned nipple-areolar complex (NAC). In addition to this, try to make do with minimally extended incisions, which in the end will be unnoticeable.
In aesthetic mammoplasty, breast reduction is one of the most difficult and at the same time interesting operations (of course, after reconstructive operations). Of course, to perform reduction in large volumes, it is necessary to have decent experience in performing similar operations in small and medium volumes of resection of breast tissue. It is unspoken among surgeons that a reduction of more than 400-500 grams on each side is no longer “small”. This type of operation requires absolute knowledge of the characteristics of blood circulation in the mammary gland, in particular the blood supply to the SAH. And we will begin our photo report with a brief overview of the circulatory system of the mammary glands and its anatomical structure. In the future, this will help the inquisitive reader to correctly assess the amount of work carried out by the surgeon to recreate the shape of the female breast.
Blood circulation of the mammary glands (MG)
The SAH receives a double blood supply - directly from the adjacent parenchyma of the gland and through the subdermal (subcutaneous) plexus. To put it simply, the mammary gland is enveloped on all sides by the choroid plexus, like a cobweb. Large vessels coming from the depths pierce the deep muscular fascia along the periphery of the breast, in areas of minimal displacement of the skin and the parenchyma itself. In the area of SAH, where the displacement of the breast is maximum, all direct skin perforators from the periphery of the breast merge into the choroid plexus.
In 1998, E. Wuringer and co-authors described the supporting ligamentous system of the breast, within which they identified a very important structural unit - a horizontally oriented fibrous plate (septa). It originates from the fascia of the pectoralis major muscle (PVM) and runs along the 5th rib, crossing the entire thickness of the breast and reaching the nipple. Later, many surgeons began to call this connective tissue plate the “septa of Wühringer.”
The septa divides the breast into two parts - upper (cranial) and lower (caudal) and is a kind of internal “bra” that supports the entire weight of the tissue of the upper half of the mammary gland. In addition, the diagram clearly shows that the main vessels feeding the SAC pass through the Wühringer septum. And today, thanks to the modern understanding of the blood circulation of the breast, there are methods of reduction mammoplasty with preservation of only the isolated central feeding vascular pedicle (that is, the Wühringer septum), which provides the most guaranteed blood circulation. But you need to take into account that the heavier the breast, the more the septum and the vessels passing through it stretch. This means that blood circulation through the septal arteries in the area of the SAH is impaired to some extent. Therefore, a surgeon planning a significant reduction of the breast must correctly assess the initial condition of the breast and choose the most reliable (in terms of maintaining adequate blood circulation to the SAH) method of operation.
So, the main “technical” tasks facing a plastic surgeon:
1)
choose the most optimal option for the formation of a “feeding leg” responsible for the blood circulation of the SAH;
2
) select an option for remodeling the parenchyma (breast tissue);
3
) determine the type of excision of excess skin “cover”: using only a circumareolar suture
,
a combination of periareolar with a vertical (in various modifications) or inverted T-shaped (“anchor”) suture.
Circumareolar suture
Vertical seam
J-stitch
Inverted T-stitch with short horizontal component
Inverted T-stitch with matching horizontal seam
In choosing the method of operation and the “cut” method, the surgeon relies on his professional experience and skills. And, as you know, the best method is the one that the surgeon knows, if not perfectly, then at least very well. After all, regardless of the surgical method chosen by the surgeon, the external result may look equally good (or not so good) regardless of which feeding “leg” or which cut of the skin “cover” was used during the operation.
Feeding “legs” of the SAC
So, relying on knowledge of anatomy, you can choose 2 ways to preserve blood circulation in the SAH.
First
the path involves the blood supply to the SAH due to the parenchyma of the gland adjacent to the areola, through which the perforating arteries pass. This is the so-called “central leg”, which includes the Wühringer septum with vessels and nerves passing through it. With this type of operation, it is possible to completely separate the SAH from the skin, crossing the skin to the full depth along the perimeter of the areola. At the same time, according to the author, there is no need to be afraid of crossing the entire vascular network of the subdermal plexus. However, among most surgeons this method of operation has not found wide clinical use due to the technical complexity of its implementation.
Second
the path is the formation of a dermoglandular feeding “leg”. With this option, blood circulation is maintained both through the subdermal plexus and due to the parenchyma underlying the SAH with perforating arteries passing through it. Today, the following types of dermoglandular pedicles are distinguished: upper, lower, medial (internal), lateral (external) and combined.
Each of the listed feeding legs has certain advantages and disadvantages:
Upper "leg"
provides maximum blood circulation to the SAH. It is preferable for moderate and moderate reductions; it allows resecting the central and lower part of the breast. It is possible to maintain SAH sensitivity, but lactation may be disrupted.
The lower “leg” is possible for large reductions, as it provides good blood circulation to the SAH (including due to the septal blood supply), allows maintaining lactation and sensitivity of the SAH (with small and medium reductions). Among the disadvantages, in the long term, sagging of the lower slope of the breast may be observed due to the preservation of the lower and central parts.
Lateral "leg"
used only for moderate resections, blood circulation only from the lateral thoracic artery (septal blood supply is not preserved), sensitivity and lactation may be preserved.
Medial "leg"
can be used for any volume of resection, provides the best blood supply due to the upper direct perforators, allows resection of the central and lower part of the breast, and there is a high probability of maintaining the sensitivity of the SAH. The disadvantage is that lactation is disrupted.
There are several dozen options for reduction mammoplasty using one or another feeding “leg”. Of course, we will not dwell on all the known methods of this type of operation, since this information will cause unnecessary overloading of the already difficult-to-understand material. But several of the most popular techniques (which are well-known among forum readers) will be touched upon.
Weiss technique
(R. Wise, 1956) is based on the formation of the lower feeding “leg”. This is one of the methods of reduction mammoplasty most often mastered by plastic surgeons. Preoperative markings are absolutely templated, with clear dimensions (without deviations or “fantasies”) and have the appearance of a “keyhole”. The tissue of the upper and lower lateral (outer and inner) segments of the breast is resected. As a result, the operation always ends with the formation of an inverted T-shaped suture.
Scheme (left) of the isolation of the lower feeding “leg” of the nipple-areolar complex (a) in the form of a “pyramid” (b), c - a vertical section of the isolated complex. Preoperative marking according to the Weiss scheme. Preoperative markings (right).
Also, with standard marking according to Weiss, you can use the upper feeding “leg”. In this case, the lower and lateral parts of the breast are subjected to resection, the wound is sutured to form a characteristic inverted T-shaped suture.
If we talk about vertical reduction mammoplasty, the most popular method is the Madeleine
Lejour
(M. Lejour, 1990). With this technique, the blood supply to the SAH is provided by the upper feeding “leg”.
The marking pattern around the areola resembles the dome of a mosque. Liposuction of subcutaneous fatty tissue in the lower and lateral parts of the breast is first performed. The tissue resection area is the lower central block and lower lateral parts.
Next, a tunnel is formed by detaching the breast tissue from the muscular fascia to the level of the 2-3 ribs, where the parenchyma is pulled up and fixed (essentially a plication) with non-absorbable threads. The lateral “columns” of the lower segment of the breast are sutured together. To avoid an additional horizontal inframammary seam, the author suggests gathering the skin at the lowest point of the vertical seam, in the hope that the skin will gradually straighten and the folds will move away. But, unfortunately, this does not always happen and the so-called “dog ear” is formed, which may require additional surgical correction. The peculiarity of this operation is also that at the end of the intervention the upper part of the gland has a convex shape, and the lower part is flat (“humpbacked chest”). Over time, under the influence of gravity and its own weight, the breasts take on a natural teardrop shape.
In the id of the breast immediately after surgery using the Lejour technique: the upper slope (B) is “humpbacked”, overcrowded; lower (H) – short and tucked. The vertical incision (P) practically does not reach the level of the inframammary groove.
In 1999, Elizabeth
Hall-Findlay
(E. Hall-Findlay - another great female plastic surgeon!) proposed her method of vertical mammary reduction, slightly different from the Lejour method. First of all, this technique uses the medial feeding “pedicle”.
Tissue resection is carried out in the upper, outer and lower quadrants of the breast, after which the medial leg is rotated (turned) clockwise, and its lower part forms a lateral medial (inner) “column”, which is sutured with separate interrupted sutures to the lateral (outer) “column” " The edges of the skin wound around the areola are vertically sutured with 2 rows of separate interrupted sutures and a continuous intradermal suture. If necessary, liposuction of excess fat folds in the area of the submammary fold is additionally performed. According to the author, the medial “leg” allows for adequate vascularization of the SAH - there is no likelihood of torsion or compression of the “leg” (unlike a vertical, especially very long “leg”) and it is possible to resect fairly large volumes of breast tissue without difficulty.
But, as they say, “every sandpiper praises his swamp.” There are no ideal methods that would guarantee 100% absence of problems and complications after surgery. And the emergence of more and more new methods of operations or their modifications once again confirms that the search for an “ideal” technique suitable in each specific case continues to this day.
Reduction mammoplasty according to Dennis Hammond ( D.
Hammond , 1999)
Which he called “Short Scar Periareolar Inferior Reduction (SPAIR).” This is a vertical short-scar mammoreduction on the lower feeding “leg”. It is quite a difficult technique to master if you do not have experience in performing at least a vertical lift or a small reduction according to the above-mentioned author. At our winner of the promotion, we will try to describe in detail the main points of the operation using the SPAIR method.
This is not a public offer! There are contraindications. Before use, consultation with a specialist is required.
Our patient is 40 years old, height 170, weight 86 kg, breast size 85/E (according to her), she has three beautiful children. Her wish is to have breasts no larger than size 3 after the operation.
True, so far none of the patients have explained to me specifically what a 3rd or 3.5th breast size is. How to measure this? If with the palm, then whose? If it’s a cup, then which brand’s bras can serve as a standard? In general, at least for myself personally, I cannot yet select any specific criteria when determining specific bust sizes...
It’s not only the unsightly appearance of the mammary glands (ptosis, asymmetry), but also physical pain in the back, constant marks from the indentation of bra straps, etc. that are troubling. The “mistresses” of such a luxurious bust are well aware of all its “charms”. Before the operation, we discussed in detail all the nuances of the upcoming intervention, and came to the general opinion that, after all, breast size 3 (taking into account body type, height, weight) may look a little inharmonious and too “modest”.
Next we proceed to marking
. This is a very important detail before the operation and you must follow all the recommendations of the author of this technique.
We will not describe our marking maneuvers in detail, since everything will become more clear when commenting on intraoperative photographs. In short, there is moderate asymmetry: the left breast is larger than the right, turned outward; ptosis of the 3rd degree. The shaded areas are areas of tissue resection. The remaining lines around the areolas are the boundaries of the skin incision.
The operation is performed under general (intubation) anesthesia. Position the patient on her back with her arms slightly spread to the side.
We use a special areolar marker (in the upper right corner) to mark the future size of the areola. In this case, its diameter should not be less than 42-46 mm. Otherwise, there will be a very large gathering and corrugation of the skin around the areola at the end of the operation. A gauze tourniquet is applied to the base of the chest in order to stretch the relaxed skin as much as possible in the area of future incisions.
All intended incisions are infiltrated with saline solution with the addition of lidocaine and adrenaline. This allows not only to make an accurate skin incision strictly perpendicular, but also to significantly reduce bleeding during surgery; detachment and de-epidermization will be easier.
A skin incision is made around the boundaries of the “new” areola, and then along all the outlined lines. We believe that it is preferable to use a scalpel for this rather than an electric or radio knife or laser. Still, for good healing of the edges of a skin wound, it is better not to use such “newfangled technologies”. But deeper, for bloodless, gentle and fast work with tissues, you definitely need to have modern electric knives in your arsenal (we are deliberately not talking about the name so that there is no hidden advertising).
The skin incisions are completed (a) and de-epidermization of the area of the lower feeding “leg” around the areola is carried out. It is very important not to damage the dermis itself (whitish in color), since it is necessary to preserve the integrity of the choroid plexus running underneath it around the SAH. We wrote about this when discussing the feeding “legs” and blood circulation of the breast. The left crescent-shaped area of skin with underlying parenchyma will be subsequently resected by us as a single “block” of tissue.
A special electric knife comes into play, with the help of which we perform tissue resection almost bloodlessly and quickly. A small strip of dermis is left along the edges of the skin incision - a “border” about 5-6 mm wide (a), which will help to hold the tissue more tightly when suturing the edges of the wound (the thread will cut through the soft fatty tissue). Resection proceeds along the outer edge of the skin incision, to the entire depth of the breast parenchyma to the fascia covering the pectoralis major muscle (PM). In the photo we see that the gland is mainly hypertrophied (enlarged) due to adipose tissue and, to a lesser extent, due to the parenchyma of the gland itself (b). Parenchymal (glandular) tissue differs in structure, color, and density from fatty tissue.
The thickness of the remaining gland tissue in the upper slope (a) should be approximately 5-6 cm (in the photo between the thumb and middle finger of the right hand). The same thickness should be along the inner edge of the breast, and along the outer edge the thickness should be no more than 1 cm. Therefore, it is very important to carry out correct tissue resection, in one block and without unnecessary movements. The stage of intersection of the parenchyma of the upper edge of the future resected “block” has been completed, which, as can be seen, is still connected with the lower dermoglandular “leg” of the SAH (b). The “leg”, about 8 cm wide, starts from the inframammary groove and continues upward; at its top the SAC “proudly” lies. The boundaries of the pedicle are marked on the skin by parallel vertical lines, retreating from the meridian (midline of the breast) by 4 cm. The branches of the arteries, which are very important for the blood supply, lie inside this pedicle.
The stage of resection of a block of breast tissue with preservation of the Würinger septum, with arteries and branches of the sensory nerve passing through it (see the anatomical structure of the breast above). It is very important to leave a dermal “border” about 1 cm wide around the areola on the feeding “leg”.
Tissue resection is complete. The “leg” that feeds the SAH is displaced downward, its base is wide, attached to the pectoral fascia and includes the horizontal septa of Wühringer. The color of the nipple and areola is good, without signs of ischemia (circulatory disorders). And this always means that the vascular nutrition of the SAH is adequate and this fact brings constant joy to the operating team.
Next begins the most exciting moment for the surgeon, called “breast remodeling.” To put it simply, the stage of “assembling a piece-by-piece construction kit.” To achieve a good result, the surgeon is required to perform almost exactly all the maneuvers recommended by the author of this technique.
a
b
V
The assistant pulls the “leg” up (a), while the surgeon brings the inner and outer edges of the skin incision together until they close (b). The task is to form a closed “ring” around the areola. A temporary staple is applied to the closed edges of the skin using a stapler (c). In this case, the outer diameter of the “ring” should exceed the diameter of the areola, but not more than 1.5-1.6 times. Otherwise there will be very strong tension on the wound edges around the SAC.
View of the right breast after bringing together the edges of the skin around the areola (a). Next, it is necessary to determine how much excess skin needs to be removed in the lower part of the breast. To do this, the skin of the lower slope of the mammary glands is matched so that it covers the collected breast (b).
This is not a public offer! There are contraindications. Before use, consultation with a specialist is required.
Preliminary view of the right collected breast tissue in comparison with the “intact” left breast muscle after applying staples with a stapler (a). The patient is transferred to an orthostatic position (“sitting”) and the surgeon uses a marker (in this case, potassium permanganate) to mark with horizontal lines how the skin will be compared (b); the final look after marking the skin of the lower slope of the breast and excess skin around the areola to give it uniform roundness. Since there are significant differences in breast shape in the supine and standing positions, it is very important to evaluate all parameters of the “collected” breasts in the patient’s orthostatic position. After all, this is how the patient will evaluate the result of the operation in the future.
This is not a public offer! There are contraindications. Before use, consultation with a specialist is required.
In the orthostasis position, the surgeon makes a final assessment of the shape and size of both breasts (shape, size). Below in the photo is the removed tissue of the right breast, its weight was 271 grams. In my opinion, this amounts to a decrease in breast size of approximately 2 haberdashery cup sizes.
Next, the temporary staples are removed and excess skin will be excised according to the intended pattern shown in the diagram. Vertical parallel lines (c) are the boundaries of the lower dermoglandular “leg”, triangles marked with a cross along the upper outer boundaries of the “leg” are the zones of additional resection of skin and breast tissue. Final view of the remaining feeding “leg” of the SAC (d).
The above diagram of the stages of the operation is shown in the intraoperative photographs. In our case, the excess skin and gland tissue along the lateral (outer) edge of the “leg” is much larger than the small triangle in the diagram (central image). In the “leg” area, the skin is not excised to its full depth; it is de-epidermized in order to preserve subdermal blood circulation.
This is not a public offer! There are contraindications. Before use, consultation with a specialist is required.
Final view of the right breast compared to the left breast after removing excess skin and applying internal sutures (before suturing the skin).
Some technical nuances of the operation were not described in detail, since they are quite difficult to clearly reflect in photographs. These include: fixation of the base of the lower feeding “leg” to the fascia of the pectoralis major muscle in a new position, plication of the tissues of the upper slope of the breast for greater fullness, etc. But these are the “little things” that matter more to professional surgeons.
The reduction of the left mammary gland is carried out in a similar manner.
The image shows the completion of the resection stage of the left breast tissue; the weight of the removed fragment was 313 g. The feeding lower dermoglandular “pedicle” is shown.
View of the mammary glands in the position of orthostasis after preliminary “assembly”, on the left - still with staples applied with a stapler.
Also, to obtain an even circumference, excess skin around the areola is removed, then a circular suture (along the entire circumference) is applied to the edges of the skin around the SAC using a non-absorbable Gore-Tex 4/0 thread on a straight needle. The outer diameter should be slightly smaller than the diameter of the “new” areola, in our case - about 4 cm.
Next, a circumareolar Hammond blocking suture is placed between the areola and the outer edges of the skin incision.
For this reason, at the beginning of the operation, we left a strip (“border”) of dense dermis, inside which the thread will be passed. The purpose of such sutures (circular and circumareolar blocking) is to relieve tension on the edges of the wound around the areola and prevent stretching of the areola in the postoperative period. Rubber strips (drains) are left in the wound to prevent the accumulation of wound discharge and the formation of hematomas.
A
b
The stage of suturing the edges of the wound with an intradermal suture using an absorbable monocryl thread 4/0 (a); final appearance of the breast at the end of the operation (b).
In some cases, at the end of the operation, to prevent circulatory problems, we inject papaverine directly under the areola. Local application of papaverine leads to dilation of small arteries and improves blood flow to the SAH. After applying internal sutures, some authors recommend applying a special medical acrylic glue to the skin to seal the edges of the wound. In our opinion, this disrupts the natural release of a small amount of ichor between the sutures, so we do not use it. We smear the chest with a mixture of Traumeel S and Bepanten ointments, apply semi-alcohol bandages (with 10-20% dimexide possible) and put on compression garments.
This is not a public offer! There are contraindications. Before use, consultation with a specialist is required.
This is not a public offer! There are contraindications. Before use, consultation with a specialist is required.
In the days following the operation, dressings are performed. To improve blood circulation, reduce swelling, quickly resolve hematomas, hemorrhages, physiotherapy is performed (microcurrent lymphatic drainage with homeopathic medicines, magnetic therapy, phototherapy). The drains are removed 2-3 days after surgery. The seam is treated with a strong solution of potassium permanganate. The photo shows the patient’s view on the 5th day after surgery.
In the postoperative period, patients wear a support top for 3-4 weeks; heavy physical activity, active sports, and hot procedures (baths, saunas) are excluded. Swelling and bruising may persist for several weeks.
The final shape of the breast can be assessed by 3-4 months, sometimes by six months.
At first, the breast has a slightly overcrowded upper slope and a flattened lower slope; the nipple seems to be “sadly looking” down. Subsequently, under the influence of gravity, the breast acquires a natural, teardrop-shaped shape, the nipple begins to look “proudly and cockily” straight or slightly upward. The skin folds (assemblies) around the areola and along the boundaries of the vertical seam gradually diverge over 3-4 weeks. To communicate with patients who have undergone breast augmentation, lifting or reduction, come to our forum in the Mammoplasty
Rehabilitation after breast reduction
For a month after reduction mammoplasty, wearing compression garments is recommended. In the first few days after the intervention, a slight increase in body temperature is possible.
During the recovery period after breast reduction, it is necessary to exclude active physical activity, as well as visiting the pool, sauna and bathhouse. You can resume your normal schedule and return to work in 7–14 days. The final results of the operation can be assessed after six months.
Possible complications of reduction mammoplasty include:
- pain and discomfort when moving at the early stage of rehabilitation;
- decreased sensitivity in the operated area;
- hematomas;
- decreased/increased nipple sensitivity;
- hypertrophic scars at the incision sites;
- asymmetry of the mammary glands.
Why do women want breast reduction?
Among the reasons why women decide to reduce their breasts are dissatisfaction with their large size and congenital asymmetry of the mammary glands. In addition, large breasts can lead to health problems, including:
- poor posture;
- curvature of the spine due to uneven load;
- dysfunction of internal organs as a consequence of problems with the spine
- headaches, back pain, muscle pain due to the load on the cervical spine;
- disturbance of gait, balance;
- difficulty breathing when lying down, sleep disturbance.
- increased sweating under the mammary glands, maceration (diaper rash)
After operation
The results of breast reduction depend on factors such as weight fluctuations and changes in the hormonal balance of the patient's body. If these parameters remain constant, then the effect of mammoplasty lasts for many years.
Not only Moscow residents can undergo breast reduction surgery. Patients come to us from Volgograd, Voronezh, Yekaterinburg, Kazan, Krasnoyarsk, Nizhny Novgorod, Novosibirsk, Omsk, Perm, Rostov-on-Don, Samara, Ufa, Chelyabinsk and other cities of Russia.
We use innovative plastic surgery techniques and guarantee results that meet your expectations. Make an appointment with a surgeon online or by phone.
Advantages of performing surgery at the SPIC clinic
The high qualifications and extensive practical experience of surgeons at the SPIC clinic allow them to successfully perform breast reduction operations, combining minimal trauma, the absence of complications with modeling a beautiful breast shape.
The price for breast reduction includes all expenses: consultations with a surgeon, preparation for the operation, the operation itself, anesthesia, stay in the ward with meals, postoperative care.
For out-of-town patients, service packages are offered, including transfers around St. Petersburg and special prices for accommodation in comfortable rooms in the clinic’s partner hotels.