Issues discussed in the material:
- Why can your eyes hurt after eyelash extensions?
- What to do if your eyes hurt after eyelash extensions
- When should you see a doctor if you have eye pain after eye extensions?
- What materials should a specialist use to prevent eyes from hurting after eye extensions?
Eyelash extensions are not complete without slight redness of the eyes that appears after it is completed (sometimes they even hurt). If the technology is followed, the redness and excessive tearing will stop after 2-3 hours. However, there are situations when the help of a doctor and drug therapy are required to eliminate the negative consequences. When your eyes hurt after eyelash extensions for 4 hours or longer, this indicates a specialist error or an allergic reaction to the materials used.
Why do my eyes hurt after eyelash extensions?
During an eye extension session, the eyes are exposed to physical and chemical effects for a long time (several hours). They may turn red and hurt a little even with a professionally performed procedure, with strict adherence to technology and using only high-quality materials and tools. Causes of eye strain leading to slight redness may include the following:
- They are closed and tense for a long time (during sleep, when closed, the muscles supporting the eyeball relax).
- The air coming from the fan causes the eyelids to become dry and irritated. A fan is needed to more quickly ventilate harmful fumes from the glue.
- There is discomfort from protective patches, especially when they are removed at the end of the procedure.
It is for these reasons that after eyelash extensions your eyes are red and sore. However, these symptoms should subside in about 2 hours.
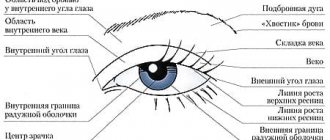
Symptoms of demodicosis of the eyes
With demodicosis of the eyelids, symptoms characteristic of this disease occur. Often the patient complains that even after minimal strain his eyes get tired. In addition, photosensitivity, burning and irritation of the eyes, itching, and heaviness of the eyelids appear.
Manifestations of demodicosis bring great discomfort to the patient. In this case, the edge of the eyelid usually becomes red, inflamed, accompanied by swelling, viscous and foamy discharge, which are localized in the corners of the eyes. Externally, scaly formations can be distinguished between the eyelashes.
If complications arise against the background of demodicosis of the eyelids, then the growth of ciliary hair is disrupted and atrophy occurs. Sometimes eyelashes simply fall out and their growth is disrupted. In addition, with this disease, ulcers, ulcers, plaque, and papillomas form along the edge of the eyelids. The eyelashes themselves are covered with sticky crusts.
How to determine the cause of redness
When, after eyelash extensions, the eye becomes red and painful, or, even worse, swollen, this may indicate an allergy. A reaction to the materials from which eyelashes are made can manifest as dry mucous membranes. An allergy to glue results in itching.
Microdamages will make themselves felt by the sensation of the presence of a foreign object in the eyes, which constantly hurt, profuse tearing and redness of the skin around.
A chemical burn appears as distinct red spots on the whites, and the eyes hurt when you move your gaze.
If there is inflammation, swelling or severe swelling will be noticeable. The eyes will hurt when moving, and a cloudy liquid will be released from them. It happens that a person cannot even move his gaze.
Recommended reading:
- How to make your face beautiful: main care rules
- Facial skin care after 25: how to maintain youth
- Why eyebrows fall out: 14 common causes and ways to combat them
First aid
According to statistics, the degree and depth of damage to the cornea is influenced not by the type of traumatic impact, but by the duration of its contact with the surface of the eye. That is why everyone, without exception, needs to know basic first aid measures.
Important! A quick and correct reaction is especially important in cases where there is a thermal or chemical burn to the cornea of the eye.
What needs to be done to stop or reduce the influence of traumatic factors
:
- rinse the eye with a stream of cool, clean water, preferably saline, but regular tap water will do;
- remove foreign bodies from the surface of the eye, especially if they are hot metal particles (molten polymers should not be touched);
- Place a gel or ointment with an analgesic effect in the conjunctival sac to relieve pain and prevent the development of shock.
In the first hours after the patient’s admission to the hospital, doctors must rinse the lacrimal canals and remove foreign bodies embedded in the membrane of the eye. To prevent infection, chemically neutral antiseptic solutions are used to wash the eye.
Important! It is strictly forbidden to wash off chemical reagents from the surface of the eye with other chemicals, for example, acids and alkalis and vice versa, as this can lead to additional damage. Experts note that treating a combined corneal burn is many times more difficult than a specific type of burn.
What to do if your eyes hurt after eyelash extensions
Pharmacy and home remedies will help relieve discomfort. It is not recommended to self-medicate if the redness of the eyes (and when they hurt) persists for more than two days. Contact a hair extension specialist first to remove artificial hairs, then go to a doctor for medical help.
1. Pharmacy products.
If your eyes hurt after eyelash extensions, and you are wondering what to use, decide on the symptoms. Conventional therapy includes antihistamines and medicated drops:
- to reduce the symptoms of allergic reactions, take tablets or drops of the antihistamine group (Tavegil, Suprastin, etc.);
What is the tear film and why is it necessary?
The tear film is a liquid, constantly renewed biostructure, which is part of the ocular surface, covers the cornea and performs important functions for the life of the eyes: optical, protective, immune, respiratory and nutritional.
The tear film is necessary for the proper, full functioning of the eyeball. Structurally, it is heterogeneous and consists of three layers. The tear film also has a very complex chemical composition, including water, numerous nutrients and special protective substances, all the necessary and balanced components for the normal functioning of the anterior surface of the eye. It also provides support for local immunity, antibacterial and respiratory functions. The tear film, leveling the surface of the cornea, provides its optical function and is a refractive medium, while having on its surface at the border with the air the highest refractive power of the order of 60D. In this regard, even minor disturbances in the tear film can greatly reduce visual acuity.
The amount of basic tear secretion per day is up to 2 ml, while the tear film has nothing in common with the tear produced by the lacrimal gland in a reflex state.
Need to know! The lacrimal gland provides only reflex lacrimation only for a protective purpose in response to physical or other irritation of reflexogenic zones (foreign body, volatile chemicals, thermal effects), as well as due to a psycho-emotional response.
The lacrimal gland is capable of secreting up to 30 ml of tears per minute, depending on the intensity of the irritating agent. Its secretion has a higher osmolarity and therefore moderately irritates the ocular surface and cannot replace the tear film.
Mucin layer of the tear film
The mucin layer is produced by goblet and granule cells, glands of Manz (limb) and crypts of Henle.
A gel consisting of mucin forms a smooth surface of the epithelium, facilitates the sliding of the eyelids along the cornea, cleanses and moisturizes the epithelium, and imparts hydrophilic properties to the epithelium.
The mucin layer makes up only 0.5% of the total thickness of the tear film. Its main task is to impart hydrophilic properties and adhesive ability to the primarily hydrophobic corneal epithelium. It is for this reason that the tear is held quite firmly on the cornea. In addition, mucin smoothes out all micro-irregularities of the epithelial surface and gives the cornea its characteristic mirror shine.
Aqueous layer of the tear film
The aqueous layer is the most prominent, produced primarily by the tear glands (95% of the aqueous component of the tear film), with the additional glands of Krause and Wolfring producing the remaining 5%. The aqueous layer consists of water-soluble electrolytes and organic low-molecular and high-molecular substances. Continuously updating, this layer ensures, on the one hand, the delivery of oxygen and nutrients to the epithelium of the cornea and conjunctiva, and on the other, the removal of carbon dioxide, metabolic products and exfoliated epithelial cells.
Lipid layer of the tear film
The lipid layer is produced by the Meibom glands located in the upper and lower eyelids. Normal meibomian gland secretion is formed from unsaturated fats, and its oleic acid content determines its melting point. When the amount of oleic acid decreases, the secretion hardens (compacts) due to an increase in the melting point of lipids and normal body temperature becomes insufficient to maintain lipids in a liquid state. Under the influence of body temperature, the meibomian glands become denser, causing secondary blockage of the excretory ducts, which leads to inflammation. The lipid layer prevents excess evaporation of the aqueous layer and gives the outer surface of the tear film a smooth appearance.
How to protect yourself from eye redness after eye extensions
To avoid dissolving the glue, do not wash your face for the first 2 days after eyelash extensions. You need to avoid places with high humidity and high temperatures for 3-4 days. You should also not use fatty creams or products with oils. We do not recommend swimming in sea water, as salt ingress can lead to irritation.
Do not rub your eyelids, curl or dye your eyelash extensions, or sleep face down. After washing, you should not rub your eyes with a towel; it is better to dry them with a fan.
If you follow these recommendations, you will avoid complications after extensions.
Also keep in mind:
- Since the home environment is far from sterile, it is better to carry out the procedure in a professional salon.
- It is important to choose the right specialist. Ask about his experience, certificates, diplomas, talk to his clients for whom he did extensions.
- Before the procedure, perform allergy tests. Do a test extension - glue a few hairs and observe the reaction for several days.
- The place where the procedure will be performed must be clean, and the instruments used in the work must be sterilized (or disposable).
- The extension specialist must have disposable gloves.
- Ask your specialist to use gel or silicone patches to protect your eyelids.
- It is safer for eye health to use hypoallergenic materials.
- It is very important to keep your eyelids lowered during the procedure and for at least 15 minutes after.
- Try not to speak during the session, as there is a risk of lifting your eyelids with facial movements.
After extensions, nothing should hurt, so if discomfort occurs, you need to stop everything and remove the artificial eyelashes.
Sometimes girls, planning to have extensions and knowing about the risk of allergies, take a course of antihistamines before and after the procedure (3 days). To do this, you must obtain permission from a doctor who will prescribe the correct medicine.
Do not forget that a lash maker, even if he is the most experienced, has completed courses and is certified, is still not a doctor. Therefore, if your eyes hurt after eyelash extensions the next day, he has no right to prescribe any drug or procedure to treat the consequences.
How to remove: what to do?
Before performing the extension, the specialist must provide recommendations on the means by which side symptoms can be alleviated. For this, both pharmaceutical products and self-prepared ones can be used. Each has its own advantages and disadvantages.
Folk remedies
If you feel pain in your eyes, then do not hesitate. Urgent action is needed. Timely help will quickly eliminate unpleasant symptoms.
The following recipes are usually used from folk remedies:
- A cucumber compress helps. One fruit is grated, and then the juice is squeezed out of the resulting product. The compress must be applied to the eyes for 15 minutes. Regular procedures can get rid of swelling and redness, as well as eliminate pain.
- Oatmeal (100 g) is brewed with boiling water. Then they must cool down. Then they are wrapped in a sterile gauze bandage and applied to the eye for 5 minutes.
- Calendula is great for relieving pain and inflammation. A decoction of chamomile, which is valued for its calming and antiseptic effect, also helps. Decoctions from plants are used to wash the eyes and as compresses. For 1 glass of boiling water, 1 tsp is required. herbs. The decoction is infused for half an hour. Then the solution should cool. The procedures are performed using a cotton pad.
- Aloe is a medicinal plant that quickly relieves pain and redness of the eyes. You need to instill 1-2 drops into each eye. Aloe leaf can also be used as a compress.
Folk remedies are effective as they quickly eliminate pain. A few procedures are enough to notice the first improvements.
Drug treatment
If after the procedure there is pain in the eyes, then medications can also be used. It is important to make sure that this is not an allergy, not a microtrauma or a chemical burn.
The following drops are the best.
Albucid
This drug can be used for adults and children, only the dosage differs. The product allows you to quickly eliminate pain and other unpleasant symptoms after extensions. Adults should instill 2-3 drops 4-6 times a day. For children, 1 drop 3-5 times is enough. If inflammation appears in one eye, this does not mean that it will not appear in the second. Therefore, instill Albucid into a less severely affected eye a little less often.
Visine
Eye drops are used 3 times a day. You should instill 3-4 drops at a time. After the symptoms disappear, treatment should be completed. To ensure that the product is evenly distributed throughout the eye cavity, after instillation you need to blink several times.
Vitabact
If the pain is associated with the penetration of bacterial microorganisms, then drops are applied 1 drop inside the conjunctival sac 2-6 times a day. The course lasts 10 days. Extension of treatment is prescribed by the doctor.
It is advisable not to instill eye products yourself. Otherwise, they may get on the glue on the eyelashes.
Any medications should be used after consultation with a doctor.
Not everyone can get eyelash extensions.
There are contraindications for eyelash extensions, which the specialist must pay attention to. He may refuse because you have:
- conjunctivitis at any stage;
- injuries, defects, damage accompanied by pus and redness;
- hyperemia;
- signs of seasonal allergies, manifested in redness of the eyes, puffiness, tearing, swelling.
Expert recommendations
Botulinum toxin and SSG
The use of botulinum toxin is not widespread among practicing ophthalmologists.
Botulinum toxin is more often used by fellow cosmetologists and neurologists. We are aware of studies that prove the effectiveness of temporary blocking of lacrimal openings and lacrimal canaliculi with botulinum toxin injections7. At the same time, there are safer and no less effective, and most importantly, simple to perform and therefore accessible to ophthalmologists methods for obstructing the lacrimal ducts6.It should be noted that even a successful attempt to block the outflow pathways for some time does not exclude the use of tear substitutes, the choice of which determines the severity of the xerotic process16.
It is preferable to prescribe a tear substitute that can restore all layers of the tear film and has a maximum moisturizing effect. These properties include, among other things, artificial tears based on hydroxypropyl guar in combination with hyaluronic acid.
What signs and symptoms does a patient with dry eye syndrome exhibit?
Main signs of Dry Eye Syndrome
Even before the formation of any clinical manifestations and symptoms of dry eye syndrome, patients experience various subtle signs, which are often not given due attention and, moreover, are not always associated with eye disease. Also, these signs do not prompt patients to seek professional ophthalmological help. However, in conversations with their friends and acquaintances, patients often note fatigue, heaviness in the eyes, rapid fatigue when working with a computer or simply when reading, and also note periodic blurred vision. These precursors are subjective signs of the presence of serious problems in the ocular surface and mark the beginning of the development of dry eye syndrome.
Main symptoms of Dry Eye Syndrome
During the course of the disease, pathological changes occur in the tissues of the ocular surface, which leads to the formation and occurrence of persistent symptoms and characteristic complaints of varying degrees of intensity. At first, they simply periodically distract the patient’s attention, but, gradually intensifying in accordance with the course of the disease, they become a real painful, debilitating obstacle in everyday life.
Common symptoms include:
- tension and feeling of heaviness in the eyes;
- redness;
- itchy feeling;
- feeling of sand;
- sensation of a foreign body inside the eye;
- burning;
- decreased visual acuity (temporary or permanent);
- discomfort in front of intense light sources (photophobia);
- feeling of increased eye fatigue;
- double vision;
- pain (in severe cases).
These symptoms can worsen, creating serious difficulties in daily life, and also affect the psycho-emotional state of patients.
Treatment of eye burns
Further therapeutic strategy is determined by the nature of the lesion and complications that have developed. In different situations, antibiotics and anti-inflammatory drugs, antioxidants and vitamin therapy, regeneration stimulants, detoxification measures, and analgesics may be prescribed. In more severe cases, surgical removal of necrotic tissue, partial or complete transplantation of the cornea and/or conjunctiva, plastic surgery in the presence of a disfiguring eyelid defect, etc. are necessary.
Radiation burns (sun, welding)
Ultraviolet radiation (powerful light with an ultra-short wavelength invisible to the eye) primarily affects the skin of the eyelids, the conjunctiva and the cornea; the latter is the most dangerous. When damaged by light radiation in the infrared (thermal) range, the destructive flow reaches the retina and blood vessels.
These types of burns are usually associated with visiting solariums, unprotected presence in the area of electric welding or the action of a quartz lamp, as well as prolonged exposure to intense sun in blinding snow (especially in the polar regions). Symptoms usually develop several hours after the actual burn.
Radiation damage to the retina is a typical result of careless handling of laser equipment or unprotected contemplation of solar eclipses. In such cases, it may take several days for specific symptoms and/or decreased vision to develop.
At what age does dry eye syndrome most often appear?
Dry eye syndrome can be detected in patients at almost any age. But most often it is diagnosed in patients over 40-50 years old. However, due to environmental changes, the widespread use of technology at work and at home, and the increasing use of contact lenses, the age of patients with detectable dry eye syndrome is becoming younger.
You need to understand! If everyday life is associated with the constant presence of risks or taking medications, the side effects of which disrupt the secretory function of the glands, then regular monitoring by an ophthalmologist is necessary in order to timely correct and take the necessary measures.
Is it possible to remove the feeling of sand in the eyes after contact lenses using folk methods?
Another way to compensate for the lack of moisture in the eyes is folk recipes. For home treatment of dry eye syndrome, fans of “grandmother’s recipes” offer honey drops, decoctions of medicinal herbs, and medicinal oils.
There are even tips for using regular onions to moisturize the eyeball. To activate the production of tears, it is recommended to simply start peeling or cutting the vegetable.
But ophthalmologists do not approve of all these home recipes. Firstly, homemade drugs are not clinically tested, which means they can be dangerous to health. Secondly, it is impossible to remove the feeling of sand in the eyes when treated with folk remedies, but you can easily develop an allergy or infection.
Treatment of dry eye syndrome should be aimed at eliminating the causes of the pathology, not the symptoms. No folk recipe can cope with this, unlike Delfanto® capsules. The product contains at least 35% antioxidants (polyphenolic anthocyanins), which is a record figure for such products. Delfanto® helps fight the effects of oxidative stress and restores the functioning of the lacrimal glands.
It is important to understand that the greatest danger of unprofessional treatment is the progression of the pathological process. In the absence of adequate treatment, dry eye syndrome leads to corneal perforation, which can lead to vision loss. To prevent this from happening, you need to pay attention to the problem in time.