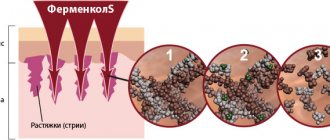
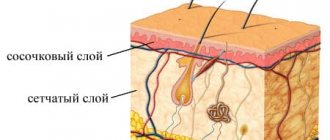
When the integrity of the skin is violated, the body reacts with a protective reaction, as a result of which new tissue is formed. If the depth of the damage is small (not lower than the papillary layer of the dermis), then complete restoration of the skin structure is possible, but with an increase in the depth of damage, the defect is replaced by a connective tissue patch - a scar.
Treatment methods for scars vary greatly depending on their type, so the correct classification of scars is very important:
1. Normotrophic - located flush with the skin, do not cause deformation of the skin and underlying tissues.
2. Atrophic - have the appearance of a thin, flat scar with translucent vessels. They form in places with undeveloped subcutaneous fatty tissue (the back of the hands, feet, the front surface of the legs).
3. Hypotrophic – located below the level of the surrounding skin (retracted).
4. Hypertrophic – protrude above the surface of the surrounding skin.
5. Keloid scars - protrude above the skin level and increase in all directions. They have a bluish-red color, accompanied by sensations of itching and pain.
Scar treatment
The most effective method for removing scars is currently laser. From laser exposure, zones of microdamage are formed on the area of skin with a scar, as a result of which scar tissue is destroyed and the production of collagen, a new connective tissue, is stimulated; the relief and color of the scar gradually aligns with the tone of healthy skin. This scar removal procedure is called laser resurfacing (dermabrasion).
To completely eliminate a scar, a complex of several procedures may be required.
Depending on the type of scar, its location, and timing, the following treatment methods are also used:
Intraruminal administration of drugs is the most effective method of reducing the volume of the scar, inhibits the growth and causes regression of keloid scars.
Separation of the bottom of the scar (skinbiogetting) and contour plastic surgery are an effective method for treating hypotrophic scars.
Bucky therapy is often used to prevent the growth of pathological scars.
Physiotherapeutic (electro-, phonophoresis with enzyme and corticosteroid drugs).
External scar treatment - ointments (contractubex, dermatix), silicone plates and coatings.
Surgical excision of the scar is most often used to treat extensive scars and cicatricial deformities. Surgical treatment can lead to the formation of scars of the same size or larger sizes. In all cases, after surgical excision, postoperative conservative treatment is mandatory.
How should you apply a suture to get a thin, invisible scar?
The main condition for proper healing of the suture is the absence of stretching. Our clinic uses a special suture technique. Its essence is as follows: the fabrics are sewn together in layers, so that all the tensile stress falls on the lower layers. The skin, on the contrary, is sewn together as freely as possible, without tension. When the suture is applied correctly, the upper layer of tissue does not stretch during healing, so the scar on the skin turns out to be very thin. Over time, it brightens and becomes almost invisible.
Scar mesotherapy
Doctor: Kwak Yu.V.
A high-tech biomaterial, type I collagen with a completely preserved native structure, COLLOST® stimulates the process of targeted tissue regeneration in the scar area. Under the influence of COLLOST® gel, the process of producing your own collagen fibers and replacing pathological scar tissue with healthy ones is activated. Collostotherapy makes skin defects invisible.
The course consists of 3-5 procedures with an interval of 2 weeks. Perfectly combined with laser resurfacing.
The cost of one procedure is 10,000 rubles.
The duration of resolution of inflammatory elements in acne correlates with the risk of scar formation. What aesthetic medicine methods will help avoid their formation, and which ones will help reduce post-acne marks?
One study found that 95% of patients experience some degree of scarring. According to other sources, resolution of acne elements with scar formation is 3.4–6.8 times more common in severe forms of the disease than in patients with milder forms of acne. In addition, it was found that in patients who did not receive adequate therapy in the first 3 years from the onset of the disease, scar deformities form 1.6–2.8 times more often.
The Global Alliance for Acne Treatment has proposed to combine the following phenomena under the term “post-acne”:
— cicatricial deformities formed during the resolution of acne rash elements; - post-inflammatory hyper- and depigmentation; - congestive erythema.
But if erythema and pigmentation disorders are temporary, then scar deformities remain forever.
There is still no clear answer to the question of what a scar is: a normal variant or a pathology. According to the classification proposed by A. E. Reznikova (1999), all types of scar deformities can be divided into two groups: normal (normotrophic and atrophic) and pathological (hypertrophic and keloid). This classification is based on the fact that the formation of normal scars occurs as a result of normal physiological protective reactions of the body in response to skin damage, while pathological scars are formed when these processes are disrupted.
Atrophic acne scars
The most common occurrence of atrophic scars can be observed, but hypertrophic and keloid scars also occur. However, the severity of scars does not correlate with the severity of the disease. The development of hypertrophic and keloid scars is observed in 10–20% of cases. Their formation is associated with insufficient activity of MMPs. They are localized mainly on the skin of the back and chest, rarely on the face. Keloid scars can develop spontaneously or long after injury.
Atrophic scars occur in 80–90% of cases and are formed more often on the face, less often on the body. According to modern concepts of scar pathogenesis, the evolution of inflammatory elements of acne resulting in an atrophic or hypertrophic scar is associated with an imbalance of metalproteinases MMPs (MMP-1, MMP-2, MMP-9, MMP-13, proMMP-1, proMMP-9), responsible for the architecture of the extracellular matrix and their tissue inhibitors TIMPs.
Post-acne scars are formed with the participation of peptidoglycan of the cell wall of P. acnes, which, through gene expression of the synthesis of proMMP-2, enhances the degradation of the extracellular matrix.
Atrophic acne scars.
M-shaped (Rolling) scars, 4-6 mm Stretched, sunken scars with sloping edges, giving the skin a wavy appearance.
V-shaped (Ice pick) scars, < 2 mm Sharp, deep, sunken scars, wide at the surface and tapering towards the base.
U-shaped (Boxcar) scars, 0.1-4 mm Superficial or deep, wide both at the surface and at the base, round or oval in shape with clear edges.
Forms of atrophic post-acne scars
There are various forms of atrophic post-acne scars: V-shaped (Icepick), M-shaped (Rolling), U-shaped (Boxcar). But since in clinical practice, as a rule, a combination of the listed types of scars is encountered, differential diagnosis between them becomes very difficult. In this regard, in 2006, D. Goodman et al. The Global Qualitative Classification of Acne Scars was presented (Table 1). This scale is quite simple and convenient for use in clinical practice, which allows you to more accurately determine treatment tactics and evaluate the results obtained.
Despite the high risk of developing scars due to acne, at the moment, modern standards of acne treatment do not indicate measures to prevent the development of post-acne scars. Although the need for preventive treatment simultaneously with the main one or as soon as possible after its completion is beyond doubt. To determine the tactics of preventive measures for the development of scar deformities, it is necessary to take into account the predictors of their development.
In this regard, the early start of acne therapy, adequate to the severity of the disease, an integrated approach to solving problems, joint work of related specialists, the right attitude of the patient, a sufficient degree of compliance in most cases are the key to a positive treatment result and preventing the evolution of acne elements with an outcome in scar.
Treatment of scars must be carried out using a properly selected method, for the selection of which an accurate differential diagnosis of the scar is important. And if it is usually not difficult to distinguish a normotrophic scar from a hypertrophic one, then the differences between a hypertrophic and a keloid scar are not always obvious.
Table 1. Global qualitative classification of acne scars proposed by D. Goodman and Baron (2006)
severity level of damage clinical manifestations points 1 Macular Erythematous, hyper- or hypopigmented flat scars that do not change the texture of the skin, but affect its color. 1 2 Weak Weakly expressed atrophic or hypertrophic scars, not visible at a distance of 50 cm or more, easily masked with cosmetics, on the chin in men - with the shadow of hair growing after shaving, in extrafacial localization - with naturally growing hair. 2 3 Average Moderate atrophic or hypertrophic scars, clearly visible at a distance of 50 cm or more, poorly masked by cosmetics, the shadow of hair growing after shaving or naturally growing hair in extrafacial localization; When the skin is stretched, atrophic scars on the face are smoothed out. 3 4 Pronounced Pronounced atrophic or hypertrophic scars, clearly visible at a distance of more than 50 cm, poorly masked by cosmetics, the shadow of hair growing after shaving or naturally growing hair in extrafacial localization; When the skin is stretched, atrophic scars do not smooth out. 4 For the differential diagnosis of hypertrophic and keloid scars, anamnestic data are of greatest importance. The development of a hypertrophic scar occurs within 6–10 months after injury, while keloid scars can occur spontaneously or several years after injury (Table 2). In patients with keloid scars, there is an increase in deep skin sensitivity; subjective itching in the area of the lesion may be bothersome. Subjective sensations of patients with hypertrophic scars are usually absent.
Additional methods for preventing scars include the use of methods aimed at improving tissue trophism, these include cryomassage, vacuum massage, electrophoresis, phonophoresis, microcurrent therapy, and magnetic thermal therapy.
Table 2. Differential diagnosis of normal and pathological scar deformities
normotrophic scars
hypertrophic scars
keloid scars
Formation 7–10 days after injury
Formation within 6–10 months after injury
Formation several months, years after injury or spontaneously
No family predisposition
Family history
Without subjective feelings
Increased deep skin sensitivity, itching
The localization of the scar corresponds to the area of injury
The scar extends beyond the injury At the same level with the surrounding skin or retracted Rise above the skin level
Spontaneously flatten
Possible flattening over a long period of time Do not flatten over the years Never ulcerate May ulcerate
Very rarely ulcerate
Normal skin color or hypopigmented Predominantly red, hypo- or hyperpigmented
How to get rid of atrophic scars? In choosing one or another method for correcting an already formed post-acne scar, the presence of inflammatory elements simultaneously with post-acne elements is of great importance, which significantly reduces the range of possible treatment methods. The main treatment of such patients should be supplemented with the use of laser techniques that are also effective against inflammatory elements of acne (PDL, Nd:YAG laser, diode laser with a wavelength of 1320 nm).
Provided there are no inflammatory elements, the World Acne Alliance for the correction of post-acne scars has approved certain types of skin resurfacing, surgical excision of an atrophic scar, the use of dermal fillers and deep peels.
Methods for correcting post-acne scars
Chemical peels When correcting more superficial scars and dyschromia, it is recommended to use mid-superficial and mid-level peels with 70% glycolic acid, 30% salicylic acid, 20–35 TCA or 40–70% pyruvic acid [3]. Due to its high efficiency, the technique of targeted application of deep TCA peeling (CROSS technique) has become widespread, especially in the correction of V- and U-shaped scars. A study by N. Khunger et al. noted an improvement of more than 50% in 93.3% of patients after 4 peeling treatments at a 2-week interval.
Surgical method A universal method for correcting deep atrophic scars are surgical techniques, which are recommended to be combined with one of the skin resurfacing techniques. Thus, in one of the studies on the effectiveness of the method for correcting M-shaped post-acne scars using surgical subcision and 100% TCA peeling in patients with phototypes III and IV (Fitzpatrick), it was revealed that the subcision method is more effective, causing fewer side effects. However, further reduction in the depth of the scar defect appears to be more pronounced with subsequent use of TSA.
A method for correcting M-shaped post-acne scars using surgical subcision.
Mechanical skin resurfacing The use of mechanical dermabrasion (resurfacing of atrophic scars) is justified in the presence of a large number of post-acne scars located close to each other. However, due to the fact that this method is very traumatic, painful for the patient, requiring long-term rehabilitation, with a high risk of developing side effects in the form of pathological scars and dyschromia, its use is very limited. Microdermabrasion is a more gentle method, but its effectiveness in correcting deep scars is less pronounced.
Similar to microdermabrasion is the method of needling using mesoscooters. According to some data, this method, by stimulating the synthesis of type I collagen, is more effective than IPL systems.
Intradermal stimulation of scar tissue (Skinbiogeting) This method is used exclusively for atrophic scars and involves separating the bottom of the scar from the underlying tissue. Technically, this technique is carried out with a simple needle with an injection of novocaine under the scar or with a special thread.
Mechanical separation of the scar from the underlying tissue causes aseptic inflammation due to injury with subsequent activation of fibroblasts. The resulting defect is filled with connective tissue, as a result of which the bottom of the scar thickens and, as a result, the depth of the defect decreases.
Dermal fillers Correction of scar deformities using dermal fillers (filling atrophic scars) has a large number of limitations: use only on atrophic U-shaped scars with a low density of scar tissue. In addition, depending on the chosen material, it has a short duration of effect – 3–12 months. The advantages of the technique are good patient tolerance and low risk of complications. Stabilized hyaluronic acid, collagen (animal or synthetic origin), and adipose tissue are used as fillers.
Mesotherapy The mesotherapy method is used for all types of post-acne scars. Vitamins and biologically active preparations that improve tissue microcirculation are used.
The use of this method is justified in combination with various types of resurfacing (peelings, dermabrasion, laser resurfacing) and in the early stages of scar formation.
Electrophoresis Electrophoresis with lidase is used only on hypertrophic and keloid post-acne scars in the early stages of their formation. 2 courses of 10 procedures are carried out daily or every other day. The break between courses is 1–2 weeks. The use of lidase is aimed at destroying the extracellular matrix, more precisely its polysaccharide component. Providing a “loosening” effect, it promotes the penetration of other medicinal substances. Since collagen is another important component of the extracellular matrix, the use of collagenase, especially in later stages of scar formation, is also pathogenetically justified. Electrophoresis with collagenase is carried out according to a similar scheme. It is possible to combine this method with electrophoresis of prednisolone or dexamethasone, since corticosteroids reduce the activity of fibroblasts, block enzymes involved in collagen synthesis, and also reduce the permeability of the vascular wall, which leads to inhibition of the growth of scar tissue.
Ultrasound therapy This method is based on the use of ultrasonic vibrations with a frequency above 16 kHz. Ultrasound has a defibrosing, anti-inflammatory effect on biological tissue and leads to acceleration of local blood circulation. It has been proven that new collagen and elastin fibers formed under the influence of ultrasound have greater elasticity.
When using low power - from 0.4 to 0.8 W - ultrasound has a stimulating effect on trophic processes in tissues. Such stimulation is indicated for the treatment of fresh scars. The course consists of 14–20 procedures with an interval of 2–3 weeks.
With increasing power, heat generation increases, and the defibrosing effect of ultrasound increases, which is necessary for the correction of old scars. The defibrosing, softening effect of scars is achieved in the range of 0.8–2 W/cm2. A regime of continuous generation of ultrasonic waves per zone for 3–5 minutes is recommended for a course of 10–15 procedures every other day.
Laser therapy Atrophic acne scars are also removed using laser therapy. As before, the gold standard in the correction of post-acne scars using laser techniques is the ablative method of CO2 laser correction. As observations show, this technique allows one to achieve clinically significant results (50–81%) after the first procedure. However, due to the fact that the CO2 laser generates high-density energy, has low selectivity to water, and creates additional zones of thermal tissue damage, the risk of side effects is quite high. Erbium laser resurfacing is a less traumatic ablative method due to its high affinity for water molecules. However, to achieve an effect comparable to a CO2 laser, several procedures are necessary.
The emergence of a new method of exposing the skin to a laser beam, fractional photothermolysis, has made it possible to reduce the trauma of ablative techniques; in addition, it has become possible to increase the depth of penetration of the laser beam with minimal trauma to the epidermis.
A feature of fractional lasers is that the radiation used when influencing biological tissue does not arrive in a continuous stream (as, for example, with broadband lasers), but pointwise, forming scattered multiple microthermal treatment zones 70–150 microns in diameter and 380–1600 microns in depth, around which intact tissue is preserved. This effect is due to a microlens matrix installed at the output of the light beam, while a high radiation density is provided in the focal spots (about 200 J/cm2).
Due to the fact that the total surface area of the lesion is only 15–20%, epidermal reepithelialization occurs quite quickly, with minimal risk of side effects.
Conclusion Thus, despite the wide range of methods for correcting post-acne scar deformities, the search for a method that provides a solution to all problems of treatment and prevention of scars has not yet been completed. Further observations may help to select the most optimal parameters for working with such patients, achieving good therapeutic and aesthetic results while reducing the risk of adverse events.
Larisa Kruglova, MD, PhD, Head. Department, Professor, Natalya Korchazhkina, Doctor of Medical Sciences Professor of the Federal State Budgetary Institution of Further Professional Education "Central State Medical Academy" of the Administration of the President of the Russian Federation; Polina Kolcheva, dermatologist, cosmetologist, Moscow Scientific and Practical Center for Dermatovenereology and Cosmetology, Moscow
How much does scar resurfacing cost?
The cost of laser scar removal usually depends on the size and complexity of the scar. You will find the prices of our clinic in the price list below.
You can ask any questions you are interested in, sign up for a scar removal procedure or a free consultation with a specialist by phone:
Sign up
Is it possible to perform a subcision procedure to remove atrophic scars on the face (post-acne), which are difficult to laser resurfacing? And what other methods are there to correct the defect?
- answers Dermatologist, cosmetologist, specialist in laser and injection techniques - Bagdasaryan A.A.:
Subcision is the cutting of the bottom of the scar with a thin needle, dense strands of connective tissue are cut and the bottom under the scar is filled with the drug.
We use the drug Collost (after a preliminary allergy test). It creates volume, smoothing the surface of the skin, and at the same time stimulates the production of its own collagen - the effect lasts for life. Not all scars are corrected by this method, only atrophic ones: retracted and rounded. During the consultation, the specialist will select the most suitable procedure. Go to the “Q&A” section
Why go to the Pirogov Clinic for the best results?
- The Pirogov Clinic was recognized as the best plastic surgery clinic
according to the national rating of private clinics in St. Petersburg by the medical portal “Doctor Peter” and the city portal “Fontanka.ru” in 2022; - qualified plastic surgeons with extensive experience in aesthetic surgeries;
- our doctors constantly exchange experience with foreign specialists, attract colleagues from Israel, which allows us to perform plastic surgeries using progressive world techniques;
- the opportunity to undergo all preoperative examinations in the clinic within one day;
- own laboratory: test results - quickly and with a guarantee of reliability;
- equipping operating rooms with the most advanced medical equipment from leading Western companies;
- attentive and responsible medical staff: a team of anesthesiologists, resuscitators, assistants and nurses coordinately and quickly resolves any issues around the clock;
- the highest standards of equipment sterility and patient safety, meeting the requirements of regulatory authorities;
- use of the latest generation of anesthesia that does not cause any discomfort after the intervention;
- modern comfortable hospital: you feel like you are in a European hotel room;
- the departments of medical cosmetology and laser dermatology carry out procedures for the fastest possible tissue regeneration, allowing you to start enjoying the results as soon as possible;
- interest-free installment payment for any transactions.
Sign up for a consultation - take the first step towards your new appearance!
Make an appointment
Price list:
Scar removal prices
| Fractional thermolysis of scars (1 sq. cm) | 1,000 rub. |
| Erbium resurfacing of scars (1 sq. cm) | 1,000 rub. |
| Erbium resurfacing of scars (more than 2 sq. cm) | 500 rub. |
| Laser (CO2) grinding (1 sq cm) | 2,000 rub. |
| Scar hormone therapy (Diprospan) | 1,300 rub. |
| Correction of retracted scars with Collost filler 7% - 1.5 ml | 13,000 rub. |
| Correction of retracted scars with Collost filler 15% - 1.5 ml | 18,000 rub. |
| Spherogel Lights 0.5 ml | 6,000 rub. |
| Spherogel Lights 1.0 ml | 11,000 rub. |
| Spherogel Medium 0.5 ml | 8,000 rub. |
| Spherogel Medium 1.0 ml | 15,000 rub. |
Scars after injuries. Who to contact?
If your suture was not applied in our clinic or even by a plastic surgeon, but urgently at the first trauma center you come across, we strongly recommend that you contact our specialist - O.A. Tsyganova. “You can resew a suture in the first 48 hours after an injury; if time is lost and more than 2 days have passed since the injury (or operation), you should consult not a surgeon, but a rehabilitation doctor - Irina Nikolaevna Ivanova or Olga Anatolyevna Tsyganova.
Need a consultation?
What results can you expect?
It should be understood that it is not possible to completely get rid of a scar, but it is possible to make it almost invisible. An integrated approach in the form of surgical correction, proper care of the p/o wound, laser treatment of scar tissue, drug therapy with the introduction of drugs into the scar tissue if indicated, wearing silicone patches and pressure bandages are today effective and reasonable methods in the treatment of pathological scars.