Botox is a drug based on botulinum neurotoxin type A, which is produced by Allergan (USA). This word is also used to refer to all analogues of the drug. The botulinum toxin injection procedure gained popularity at the end of the last century and has since remained the most popular non-surgical anti-aging technique.
Botulinum toxin: what is it and how does it help in the fight against wrinkles?
The effect of Botox is achieved due to the neurotoxin botulism type A. It is one of the most dangerous poisons in the world, but in cosmetology such microscopic doses of the substance are used that it is not at all difficult for a professional to control its effect and get a positive result.
Naturally, botulinum toxin is not used in cosmetology in its pure form. It is first stabilized and purified from protein impurities in the laboratory.
The effect of Botox is as follows: with an injection, it enters the muscle, blocking the transmission of nerve impulses in it. As a result, the muscle relaxes, its contraction stops, and as a result, the skin adjacent to it becomes smooth.
How does the drug work in neurology?
Botulinum toxin is administered to patients in minimal concentrations to block signal transmission from nerve to muscle. Thanks to this, the neurotransmitter acetylcholine ceases to be produced, and the muscle tissue relaxes. Botulinum therapy successfully treats tremors, spasms, headaches (pain syndrome is also relieved). Botox helps treat:
- blepharospasm;
- chronic migraine;
- strabismus;
- cervical dystonia, or spasmodic torticollis;
- spasticity after stroke;
- hemifacial spasm.
Indications for the use of Botox
Botulinum toxin can smooth out wrinkles in almost any area of the face. However, Botox shows the greatest effect in its upper third. So, the drug allows you to get rid of:
- horizontal and vertical wrinkles on the forehead and between the eyebrows;
- wrinkles around the eyes (so-called “crow’s feet”);
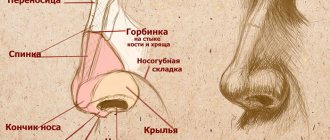
- folds on the back of the nose;
- so-called “marionette wrinkles” - labiomental folds;
- cords on the neck.
Botox is also used by highly qualified specialists for:
- correction of the shape of the eyebrows, their height position;
- narrowing of the wings of the nose and raising its tip;
- raising the drooping corners of the lips;
- visual lengthening of the chin;
- correction of facial asymmetry caused by blepharospasms and other spastic effects.
Botulinum toxin is also often injected into the feet, palms and armpits to reduce sweating. This procedure is indicated for people with hyperhidrosis, but it is often used by healthy patients on the eve of summer.
Side effects
After the session, weakness, local swelling due to fluid accumulation, numbness, and redness at the injection site may occur. Other possible side effects:
- weakness of adjacent muscles (lower eyelids, neck);
- double vision;
- influenza condition;
- nausea;
- gallbladder dysfunction;
- dry mouth;
- dyspnea;
- bleeding;
- temporary paralysis of adjacent muscles.
To minimize the risk of their occurrence, doctors examine the patient, making sure that he has no contraindications to botulinum therapy or hypersensitivity to the components of the drugs.
Procedure algorithm
It is very important that botulinum toxin injections are performed by a qualified cosmetologist or plastic surgeon. Handling this rather dangerous drug requires experience and special training. The correct volume of the drug and injection points are the key to a good effect from Botox. At this stage, you simply cannot make mistakes. Otherwise, the patient will have to pay with a damaged face for several months at best or serious health problems at worst.
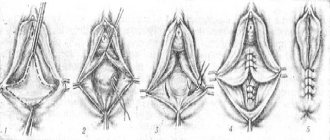
The procedure itself is carried out in several stages:
1. Cleansing. It is necessary to very carefully clean the skin of cosmetics, dust particles, etc., which can get into injection wounds and cause serious problems.
2. Marking and anesthesia. The doctor marks the points on the face where the drug will be injected and treats them with a local anesthetic. Despite the fact that the needle on the syringe is very thin and the doses of the drug are minimal, injecting Botox is painful, especially in sensitive areas near the lips and eyes. However, using a good anesthetic will significantly reduce the pain of the procedure.
3. Preparation of instruments and preparation. You have to wait up to half an hour for the anesthetic to take effect. During this time, the doctor prepares the drug - opens the package, dilutes it with saline, prepares syringes (one or several, depending on the number of facial areas being treated).
4. Injections. Next, the doses of the drug determined in advance are actually introduced into the points marked in the second stage. The patient needs to help the doctor at this stage by frowning or otherwise straining his facial muscles.
5. Antiseptic treatment. After all the injections have been administered, the doctor treats the skin with chlorhexidine and applies a cold compress to it, which will help reduce the severity of swelling and bruises that are sure to appear.
The procedure does not require particularly complex rehabilitation. You only need:
- in the first hours - do not take a horizontal position, strain the facial muscles to evenly distribute the drug in the tissues;
- in the first days - do not rub the injection sites, do not use cosmetics and care products, do not expose the skin to ultraviolet radiation;
- in the first weeks - do not go to the gym, sauna or swimming pool, do not drink alcohol or other products that retain water.
Spastic torticollis (SC) is the most common type of local muscular dystonia, which is manifested by pathological position of the head and/or violent movements in the neck muscles. The prevalence of the disease is 1 per 10,000 population. The disease debuts at any age, most often from 30 to 60 years. The etiology of KS has not yet been established; the disease is considered idiopathic. According to modern concepts, KS is the result of dysfunction of the basal ganglia and oral parts of the brain stem [9]. In addition to the central one, the peripheral (myofascial hypertonicity, joint cervical blockade) mechanism of the disease is also discussed [8].
For more than 20 years, botulinum toxin type A (BTA) has been used to treat muscle hyperkinesis. The action of botulinum toxin is based on presynaptic blockade of peripheral acetylcholinergic transmission at the neuromuscular synapse. Temporary chemical denervation of the muscle occurs with the development of muscle relaxation.
The clinical picture of KS consists of 2 main syndromes: pathological position of the head and violent movements in the neck muscles [3, 9]. The most common clinical variants of KS are torticollis (turning the head to the side), laterocollis (tilting the head to the side) and their combinations. Retrocollis (head tilting backward) and anterocollis (head tilting forward) are less common. Most patients with KS experience pain, which, along with abnormal head position and involuntary movements, significantly reduces the quality of life. There is an opinion that after botulinum toxin injections, the severity of pain according to the visual analogue scale (VAS) decreases [9]. Recent studies have shown the effectiveness of BTA in the treatment of not only muscle hyperactivity, but also pain syndromes: tension headaches, migraines, cluster headaches and myofascial pain syndromes of the neck, shoulder girdle and back [2, 7, 12].
The purpose of this study is to determine the nature of the pain syndrome in KS and assess its dynamics during treatment with injections of the drug BTA (Dysport).
We examined 53 patients (42 (79.2%) women and 11 (21.8%) men) with the idiopathic form of KS aged from 20 to 79 years (average 44±19 years), with disease duration from 1 month to 15 years (average 6 years).
Before treatment, all patients underwent a neurological examination aimed at identifying clinical manifestations of damage to the cervical segments, including the spinal roots and brachial plexus. The assessment of manifestations of KS was carried out using the West Toronto Spastic Torticollis Rating Scale (TWSTRS), which includes 3 subscales, each of which consists of signs assessed in points: a torticollis severity subscale (maximum 35 points), a disability subscale (maximum 30 points) and a pain subscale ( maximum 20 points) [4].
Dysport (Ipsen Biopharm Ltd., UK) was administered in an individual dose for each patient (from 500 to 1000 units) in accordance with the instructions for use. The most common injections were made into the sternocleidomastoid muscle (average 150 units), levator scapulae muscle (average 100 units), splenius muscles of the head and neck (average 250 and 100 units, respectively), scalene muscles (average 100 ED), less often - into the trapezius (on average 150 ED) and suboccipital muscles (on average 100 ED). The dynamics of changes in indicators on the TWSTRS scale and neurological disorders before injection and 1 month after botulinum toxin injection were assessed. The severity of KS and pain were assessed using the methods described above.
For statistical processing of the results, the Statistic program was used to calculate the weighted arithmetic mean, confidence interval, error, using nonparametric methods for assessing the sample (statistical significance level and Student's t-test for dependent samples) and determining the reliability coefficient p. Differences were considered significant at p
When assessing algic syndrome, palpation pain in the neck muscles and areas of pain according to the segmental pattern of innervation of the human body were taken into account. 8 (15.1%) patients had isolated laterocollis, isolated torticollis - in 13 (24.5%), retro- or anterocollis - in 6 (11.3%), combined (torticollis in combination with laterocollis) - in 28 (49.1%) patients. Head rotation in 30 (60%) patients was accompanied by shoulder elevation.
Isolated laterocollis resulted in more severe clinical manifestations on all TWSTRS subscales compared with other forms of KS (p
Algic syndrome was observed in 51 (96.2%) patients, mild pain was in 36.3%, moderate in 39.4%, severe in 24.3%. Most patients complained primarily of pain and, to a lesser extent, pathological posture of the head and neck. The most painful on palpation were the anterior scalene, sternocleidomastoid, levator scapulae, and splenius muscles of the head and neck. Soreness in most cases corresponded to a tense muscle. Patients presented a variety of complaints: from constant, monotonous pain with clear localization to painful and burning pain, with symptoms of dysesthesia and pain radiating to the arm. These complaints suggest the presence of a neuropathic component in the structure of the pain syndrome in patients with KS. 75% of patients with pain syndrome had signs of brachial plexopathy. According to international criteria, this type of pain corresponds to neuropathic pain [10].
Depending on the nature and location of the damage, brachial plexopathy manifests itself in a variety of clinical syndromes. In patients with brachial plexopathy, 45% had dysfunction of the lower trunk of the brachial plexus, which was manifested by weakness in the muscles of the forearm and hand and sensory disturbances on the inner surface of the forearm and shoulder. In 22% of cases, a proximal lesion of the brachial plexus was noted, manifested by dysfunction of the upper trunk of the brachial plexus, which was clinically determined by weakness of the proximal muscles of the upper limb on the affected side and impaired sensitivity on the outer surface of the shoulder and forearm, as well as a decrease in the biceps reflex. In 33% of cases with KS, a total lesion of the entire plexus was detected, in which mild paresis of the muscles of the entire limb with impaired sensitivity was determined. In 85% of patients with a neuropathic component of the pain syndrome, the duration of the disease did not exceed 5 years. It can be assumed that there is an additional mechanism of plexus compression in the early stages of SC formation and a change in the topographic “muscle-plexus” relationship during a longer course of the disease.
Nociceptive muscle pain was observed in 25% of cases, while 83% of patients with somatogenic pain had a duration of KS disease of 6 years or more. It can be assumed that pain in KS is a consequence of muscle spasm, i.e. pain syndrome is myogenic in origin. Prolonged spasm causes changes in the architectonics of contractile tissue, as well as in the structure of the receptor apparatus, which leads to afferent and efferent disorganization in the muscle. The mechanisms of inhibition of the flow of afferentation from the deformed muscle are weakened, and this in turn means the conversion of any peripheral signal into nociceptive, i.e. its qualitative change without increasing the overall level [7, 8]. The presence of a long course of the disease confirms the theory of the occurrence and persistence of myogenic pain. In 67% of patients the pain was of a mixed nature.
The largest number of observations of neuropathic pain was among patients with rare forms of KS (retrocollis and anterocollis) - 50%, as well as among patients with isolated torticollis - 42.86%, laterocollis - 40%. Less frequently, the brachial plexus was involved in the pathological process in the combined form of KS—31.25%. No significant differences were found in the dependence of the presence of plexopathy on the form of KS (p>0.05).
Before the introduction of Dysport, the severity of KS manifestations on the TWSTRS torticollis severity subscale ranged from 3 to 24 points (average - 14.8 ± 2.0 points), on the disability subscale - from 0 to 27 points (average -12.9 ± 2, 7 points), and the severity of pain on the pain subscale ranged from 0 to 18 points (on average 11.3±1.7 points). The total score on the TWSTRS scale ranged from 15 to 62 points (average 38.4±5.1 points). 1 month after the injection, the severity of manifestations varied from 3 to 17 points (average - 10.3 ± 1.9 points), disability - from 0 to 21 points (average - 7.1 ± 2.4 points), pain - from 0 to 15 points (average 5.1±1.0 points). The total score on the TWSTRS scale ranged from 5 to 58 points (average - 23.8 + 5.1 points). Thus, it is logical to state that after Dysport injections, the severity of pain, assessed on the TWSTRS pain scale, decreased in 100% of patients by an average of 6.2±1.2 points (55%, p
The decrease in pain syndrome in KS occurred earlier (on the 4th day after the injection) than the decrease in muscle tension (on the 7-8th day after the injection). If pain after Dysport injection according to TWSTRS was reduced by 55% (p
The most noticeable decrease in algic syndrome (15.0±1.0 points on the TWSTRS pain subscale on average before the injection, 5.33±1.4 points after, i.e. by 64.4%, p
Varying degrees of pain reduction can be explained by the hypothesis of early structural changes during chronic pain syndromes [1]. It has been shown that intense nociceptive impulses lead to the death of inhibitory gamma motor neurons in the spinal cord, which are normally in constant tonic activity and suppress nociceptive impulses. Thus, the balance between the nociceptive and antinociceptive systems is disturbed, and pain sensation can occur in the absence of a painful stimulus. An important mechanism responsible for the persistence of pain is central sensitization. Muscle spasm in KS leads to activation of neurons in the dorsal horn of the spinal cord. It is the formation of a hyperreactive structure in the dorsal horn with a simultaneous weakening of inhibitory processes due to complex neurophysiological processes in the muscle, segments of the spinal cord and suprasegmental structures that lead to the appearance of pain with any non-painful peripheral stimulation [7, 11].
Observation confirmed that pain is one of the main complaints of patients with KS [8]. It can be assumed that pain in KS is a consequence of muscle spasm, i.e. pain syndrome is myogenic in origin. Prolonged spasm causes a spatial change in the architectonics of contractile tissue, as well as in the structure of the receptor apparatus and leads to afferent and efferent disorganization in the muscle.
In addition, a local change in hemodynamics due to spasm leads to tissue ischemia, serotonin, prostaglandins and other inflammatory mediators are released, causing pain and subsequent reflex spasm. Thus, a vicious circle is formed: spasm-pain-spasm. Pain leading to local spasm is also possible due to pathological hyperreactivity of muscle spindles, in particular intrafusal ones [12].
According to the results of our observation, pain was often caused by involvement of the brachial plexus in the pathological process. In patients with KS, the involvement of the primary trunks of the brachial plexus, located in the area of the most frequently spasmodic muscles (the scalene muscles, directly adjacent to the trunks, the levator scapulae muscle, the sternocleidomastoid outward, etc.), is most likely to be involved. Thus, the trunks can be compressed by tonically tense muscles.
Several theories have been proposed for the analgesic effect of botulinum toxin-based drugs. The most obvious assumption seems to be that the weakening of muscle contraction breaks the vicious reflex circle, which leads to a decrease in the release of various substances that sensitize muscle nociceptors. There is probably also an indirect effect. Botulinum toxin affects the activity of intrafusal muscle fibers. Since muscle spindle afferents have important supraspinal projections, changes in their activity after botulinum toxin injections may alter the activity of sensory systems at the level of the central nervous system [7]. A number of authors [5, 6] have suggested a direct effect of botulinum toxin on the sensory system. The basis for this assumption was experimental data on the axonal transport of a radiolabeled toxin from the presynaptic region to the spinal cord. Recently, it was also discovered that botulinum toxin is able to modulate the expression of not only acetylcholine, but also other neurotransmitters, such as substance P and enkephalins, which are part of the antinociceptive system [5]. Thus, botulinum toxin has a retrograde effect.
Injections of the drug BTA (Dysport) in the treatment of KS significantly reduce algic syndrome in the treatment of KS by an average of 55%. The analgesic effect of botulinum therapy forms earlier than the muscle relaxant effect, reducing both the myogenic and neuropathic components of the pain syndrome. Since the effectiveness of Dysport is higher in patients with a shorter duration of the disease, it is advisable to start botulinum therapy as early as possible from the onset of the disease before the formation of persistent and pronounced dystonic and algic syndromes.
When does Botox start to work and how long does it last?
Already a couple of hours after the procedure, the first result is noticeable. After a few days, the effect is clearly visible visually. It will take about 2 weeks to form the final result.
If it is sufficient and satisfies both the cosmetologist and the patient, then no further manipulations are performed. Otherwise, for example, if minor asymmetry occurs, a correction session is performed with a small dose of botulinum toxin.
4-6 months is how long Botox can last. Gradually during this period, muscle and nerve fibers are restored. Six months after the injections, the procedure can be completely repeated.
It is noteworthy that several courses of Botox injections can increase the patient’s tolerance to botulinum toxin. This means that subsequent procedures will require a larger amount of the drug, and it will act in 1.5-2 times less time.
As a rule, tolerance increases if Botox is injected more often than once every 4 months. It is possible to restore the body's sensitivity. To do this, you should take a break from injections for at least 1 year.
How is the treatment carried out?
The course of treatment includes a minimum of three injections with an interval of 12 weeks. During one course, several dozen points are injected into the muscles of the head, face (frontal, temporal, occipital) and neck. The dose of the drug, the number of injections and injection sites are strictly defined. In some cases, due to the individual characteristics of the patient, it is necessary to expand the injection zone based on his condition.
Recommendations after the procedure
It is not recommended to rub the injection site for 2 hours after the injection. Overheating (visiting a sauna, bathhouse, solarium) is not recommended for a week after Botox injection After about 2-3 weeks, you need to visit a doctor for an examination and evaluation of the results.
Botulinum therapy is one of the most modern methods of treating migraine. You shouldn't be afraid of him. On the contrary, it has a lot of advantages over others. The main thing is to consult with a specialist who knows exactly how to use Botox, and then the results will not keep you waiting.
Compatibility of Botox with other procedures
As practice shows, the effect of botulinum toxin injections increases significantly if you combine it with preparations with hyaluronic acid. So, first, facial wrinkles are corrected with Botox, after which other facial irregularities are eliminated with fillers. By the way, both procedures can be performed in one session. However, this requires a very highly qualified cosmetologist.
One month before injections and for the same period after them, you should avoid any aggressive procedures such as peelings and plastic surgery.
Hardware techniques that restore connections between muscle fibers and nerve endings, such as magnetotherapy, microcurrents, galvanotherapy, ultrasound therapy or electrical stimulation, can significantly reduce the effect of botulinum therapy.
Safety
- Botulinum therapy is a branch of medicine that has existed for more than 20 years.
- Preparations based on it are used in more than 60 countries around the world.
- Before receiving official approval, all drugs undergo long-term clinical trials.
- Pharmacists agree that a course of injections is less harmful to the body than long-term use of certain medications.
- All possible side effects of botulinum toxin are transient and not dangerous to health.
- During the existence of the method, tens of millions of people have received treatment.
- Over the past 20 years, it has been possible to study not only short-term reactions to the toxin, but all possible long-term negative effects - there are none.
It is for these reasons that botulinum toxin injections are recommended by neurologists to treat a variety of conditions, from dystonia to muscle spasms and headaches.
Individual intolerance
Injections of this drug affect each person differently. If you notice that your health is suddenly deteriorating for no apparent reason, for example, your blood pressure is rising and the pain in your head is only increasing, then you are probably intolerant to Botox.
Symptoms of individual intolerance will not disappear on their own
You should call an ambulance and agree to hospitalization without hesitation. You will have to undergo medication treatment in the hospital.
When should you not worry?
If the needle enters a vessel, then Botox interacts with the capillaries: inflammation of the nerve fibers causes a headache, which quickly passes. You may also get a headache from the interaction of ethanol (alcohol) with the administered drug. When exposed to bright sunlight, a migraine can also begin, since you have to squint and thereby strain the muscles involved in the procedure.
All of the above symptoms will disappear after 3-4 days