Plastic surgery to improve the appearance of the mouth comes in two types. Aesthetic allows you to improve external data that initially falls under the normal variant.
The reconstructive direction helps to solve more complex problems when the anatomy of the zone has congenital abnormalities or is damaged as a result of trauma (failed plastic surgery, accident, accident, attack, etc.).
Plastic surgery of a lip defect requires more skill and experience from the surgeon; it is more difficult to carry out - there may be a lack of tissue, and asymmetric deformations may be observed. But even with this, a good specialist will form harmonious and natural contours.
Lip surgery after injury
The problem may lie in the presence of irregularities, dents, asymmetry, lack of tissue, scars, etc. The surgeon has several approaches at his disposal to correct the deficiencies.
- Implantation of the patient's own fat (lipofilling).
- Installation of fillers.
- The surface can be smoothed with Botox or hyaluronic filler.
- In case of serious tissue deficiency, classic surgical lip defect repair is used.
- Injections of collagen preparations.
- Scar tissue is removed by laser resurfacing.
Lip surgery after injury gives excellent results. The shortcomings 10 years ago, which were considered hopeless, are now being successfully corrected. The techniques can be combined with the task of increasing volume. Also, a plastic surgeon is able to eliminate cysts, benign neoplasms, age-related sagging of the lower lip or their transformation into a “string”.
How are sutures removed after surgery or Caesarean section?
There are two options for sutures after Caesarean:
- Horizontal. Most often, a horizontal cosmetic suture is used. It is performed using self-absorbing threads. There is no need to remove the stitches. The threads dissolve completely after 2-3 months. The seams are treated as usual, using an antiseptic.
- Vertical. This incision is rarely used, in this case the suture is vertical. It starts at the navel and ends at the pubic area. This seam is sutured using the interrupted method. Each stitch is tied with a knot. Such suture materials are removed 5-10 days after the intervention. The doctor cuts the stitches and uses tweezers to remove the threads.
How are sutures removed after surgery or Caesarean section?
Elimination of congenital characteristics
Plastic surgery for cleft lip (cleft palate and upper part of the mouth) and cleft palate (cleft palate with access to the nasal cavity) is not just a fad. This is an opportunity to return the child the necessary quality of life: the ability to speak clearly, eat, drink, and look. The earlier the correction is carried out, the greater the chances of completely eliminating the congenital pathology.
Cleft lip plastic surgery is usually performed at the age of six months, which allows children to avoid psychological problems.
Cleft lip - symptoms and treatment
A multidisciplinary team is involved in the treatment of patients with clefts, since even a well-performed operation does not guarantee the absence of other complaints. Team members: pediatrician, dentist, orthodontist, plastic or maxillofacial surgeon, nutritionist, speech therapist, ENT, ophthalmologist and neuropsychiatrist. The ENT doctor works to prevent concomitant pathology of the middle ear, which often develops with clefts, and, if present, treats it. Orthodontists make orthodontic structures (obturators), thanks to which the child can eat normally. Obturators are prosthetic devices that close a cleft and can be used for children of all age groups.
Dentists Hubener D.V. and Liu J.R. classified means for orthopedic treatment of the cleft into preoperative and postoperative, active and passive, extraoral and intraoral [14]. There was a long debate about how these methods affect the growth of facial bones and whether they worsen the prognosis, until naso-alveolar plates were invented, which were made first of acrylic, then of rubber. The plates closed the cleft, and the child could suck normally; in addition, the pressure of the plate helped support the wings of the deformed nose, improved the ratio of the lengths of the columella, the cleft parts of the lip, and gently moved the triangular bone [11].
Many types of surgical treatment have been described for the treatment of cleft lip and palate, although the possibility of performing such operations has arisen relatively recently.
Since early times, people have tried to find a way to get rid of this defect. They tried to connect the crevice with sharp sticks, then they used metal needles that were wrapped with thread. Due to the lack of means for pain relief, the operations were primitive and ineffective. Since the 16th century, they have tried to use special caps for external impact on the cleft, trying to cause the edges to stick together. The protruded premaxillary bone in the case of bilateral clefts was simply cut off, which most often led to worsening deformation of the midface.
Surgery to correct a cleft lip is called cheiloplasty . With the beginning of surgical corrections, cheiloplasty methods began to change and improve. The first operations were perceived as a miracle; they created a linear incision. Over time, they began to make incisions of increasingly complex configurations in order to correct associated deformities and prevent the appearance of new ones. Now, in order to correct the complex deformity that occurs in the midface area and create conditions for the normal development of the facial part of the skull, it is necessary that the operation fulfill the following conditions:
- Was safe for young children.
- I corrected the maximum in each specific case in 1 stage.
- Formed the correct line of the red border and Cupid's bow.
- Correct formation of the filtrum is desirable.
- Provided sufficient depth of the vestibule of the oral cavity.
- It eliminated improper attachment of the fibers of the orbicularis oris muscle and created a continuous layer of muscle, which will help in the correct formation of the bones of the facial skull.
- Lengthened the short medial part of the cleft lip.
- Corrected the shape and position of the nasal cartilage.
In 1938 A.A. Limberg described and in 1952 expanded the method of unilateral cheiloplasty. This method became the leading method in the USSR for a long time, because in most cases it made it possible to correct the concomitant deformation of the nasal wing on the cleft side.
In 1952, Tennyson C.W. in the USA and in 1955 Obukhova L.M. in the USSR they described a cheiloplasty method of a more complex configuration. The method is still used today; in addition, cheilorhinoplasties have been developed on its basis to reduce the likelihood of developing associated deformities. The techniques are interesting primarily for their historical significance: for the first time, complex-shaped incisions began to be made and the lip was lengthened. However, lengthening the lip on the cleft side was also a limiting factor because it itself created a recognizable deformity. Techniques are now being used to solve this problem.
The most used technique for suturing unilateral clefts in the world now is the Millard technique and its modifications. In our country this is a modification of I.A. Kozina.
Millard cheiloplasty involves simultaneous restoration of the continuity of the upper lip and correction of the nasal cartilage. On the medial fragment of the upper lip, point 1 is marked - the center of the cupid's bow. On the healthy half of Cupid's bow, look for limiting point 2 (apex of the arc), located approximately 2-4 mm from the midline. This distance is laid on a white roller on the shortened side, obtaining point 3. The length of the lateral fragment of the lip on the healthy side is measured between the limiting point 2 and the commissure of the mouth (point 6). The resulting distance (approximately 20 mm) is laid on a white roller on the damaged side of the commissure (point 7) and a limiting point 8 is obtained. Point 8 will be the top of the cupid's bow on this side; it should connect to point 3 on the medial segment. Measure the distance from point 2 to the base of the nasal wing of the healthy side (point 4), the same distance is set aside from point 8 to the base of the nasal wing of the affected side (point 10). On the shortened side, from the middle of the base of the columella (point 5) to point 3, an arcuate rotational incision is made, symmetrical to the arc of the philtrum on the healthy side. If necessary, extend the incision to point x (reverse incision towards the healthy philtrum). On the lateral (side) fragment, according to the length of the section x-5-3, point 9 is found medially from the base of the flattened wing of the nose. Modifications are mainly used to expand the intervention to the nose, with secondary cheiloplasty, hidden and incomplete clefts.
The advantages of this method of primary cheiloplasty:
- maximum tissue preservation;
- moving all elements of the upper lip to the correct position;
- formation of the bottom of the vestibule of the nasal cavity and the deep vestibule of the mouth.
The method simultaneously corrects the position of the deformed wing of the nose, and some modifications are supplemented with one-stage rhinoplasty. In addition, the arcuate scar is hardly noticeable and can be used for corrective cheiloplasty in adulthood.
Closure of a bilateral cleft can be one-stage or two-stage. This depends on the volume of the cleft, the experience and confidence of the surgeon in his techniques. Each option has its pros and cons, but it is believed that with the help of one-step closure of the cleft, it is more likely to fully create a sphincter of the orbicularis oris muscle.
Sometimes it is practiced to connect the edges of the cleft. This is not a full-fledged cheiloplasty, but only the transfer of a complete cleft into an incomplete one in the expectation that the pressure of the connected part of the lip will have an orthopedic effect on the edges of the cleft, which will lead to their convergence. In most Western countries, the Millard method of cheiloplasty remains the leading one [12].
With a two-stage closure, one side of the cleft is first closed using any method, and after some time the other side is closed.
The debate about at what age to perform surgery still continues to this day. There are those who urge treatment to be carried out as early as possible. Even operations on the fetus are offered, due to the lack of scarring in the prenatal period. Many insist on surgery in the first days and even hours of life. On the one hand, there are advantages to this (parents are not afraid of the child’s appearance, there are no intra-family conflicts, there are no problems with nutrition), but there are also disadvantages (imperfect thermoregulation of newborns, high sensitivity to blood loss, very small anatomical basis). In the 60s of the last century, a large-scale analysis of the results of operations performed in the maternity hospital in the first days of life was carried out. The result showed in almost all children much worse results than in patients who were operated on as adults [1]. N.M. Mikhelson, in one of the oldest Russian manuals on plastic surgery, advises performing the operation at the age of 5-6 months, when the child is sufficiently strong and developed. He believed that cosmetic success was easier to achieve during this period. It is also described that such operations should be performed under local anesthesia, due to the danger of anesthesia [10]. Now there are safe drugs for anesthesia, so it is difficult to imagine performing an operation on young children under local anesthesia. Most surgeons believe that primary cheiloplasty is indicated at the age of 6-12 months.
The extent of the operation depends on the degree of the cleft. Many modern authors believe that in case of a complete cleft, primary cheiloplasty (when only the cleft is sutured) should be used in exceptional cases, since it does not correct the condition of the nose. Therefore, now the primary rhinocheiloplasty technique should be used, when, together with suturing the cleft, the position of the alar cartilages, septum, and vomer is corrected. The quality of the primary operation should be maximum, since repeated corrections are more difficult to perform in conditions of soft tissue deficiency and extensive scarring [4].
Complications during surgery
When performing surgery, the danger is aspiration (inhalation by the patient) of blood and mucus, which can cause asphyxia. To prevent this, you should prevent bleeding and carefully suck out the contents of the oral cavity (blood, saliva, mucus). Possible complications also include collapse, shock, laryngospasm and other conditions.
Mortality on the operating table and shortly after surgery is usually associated with improper selection of patients. You cannot operate on malnourished and premature children, those who, even before surgery, suffer from inflammatory conditions of the respiratory system, hearing, and decompensated abnormalities in the development of the brain, heart, and blood vessels. Also, surgery is prohibited in the presence of thymic-lymphatic status (enlarged thymus). The possibility of surgery should be decided together with the pediatrician.
Complications after surgery
In the coming days after surgery, stenosis (narrowing) of the larynx, bronchitis, pneumonia, urinary retention and other somatic complications may occur, the prevention and treatment of which should be carried out with the participation of a pediatrician. The most common local early complication is suture dehiscence, which is usually associated with technical errors in the operation:
- excision of a significant amount of tissue in the area of the edges of the cleft;
- insufficient tissue preparation;
- incorrect layer-by-layer suturing of the wound;
- tissue tension in the wound area, inflammation and swelling in the operation area.
Sometimes the sutures come apart due to injury (a child’s fall, an accidental blow to a hard object), infection, or the child’s illness with ARVI, rhinitis and other inflammatory pathologies. If the sutures diverge, the issue of applying secondary sutures is decided according to the patient’s condition.
When examining a patient who has undergone surgery, the height of the upper lip, the degree of its deformation, the depth of the vestibule of the mouth and its tightness (the presence of oronasal anastomoses and palate defects) are checked. You should pay attention to lip mobility, phonation, and changes in the structure of the dental system. The integrity of the orbicularis oris muscle can be tested by having the patient stretch his lips into a smile and purse his lips into a tube [1].
Severe psychological trauma is caused by scar changes after an unsuccessful first operation. One of the most unpleasant long-term complications of cheilorhinoplasty is deformation of the upper lip, nose and upper jaw, which can occur for various reasons [9].
After surgery, the patient may have a lack of soft tissue of the upper lip, its lengthening or shortening, stiffness due to extensive scarring, or an aesthetic defect. Alveolar cleft leads to the formation of crowding of teeth, the growth of dystopic (improperly positioned) and supernumerary (extra) teeth, which can support inflammation or, due to their location, form an oronasal fistula (an opening between the oral cavity and the nasal cavity). In general, such a fistula can also be due to excessive tension, cutting sutures, a defect in suturing, etc. Through it, the discharge of liquid part of food into the nasal cavity can persist, which in turn helps to maintain chronic rhinitis, sinusitis, etc.
Possible insufficiency of the muscle ring of the orbicularis oris muscle, which develops with defects in muscle alignment or insufficient separation of muscle fibers from the pyriform opening. Deformation of the vestibule of the mouth in the form of its flattening complicates further orthodontic treatment, which is so necessary for patients, and aggravates the retrusion of the midface (backward displacement). Deformations of the external nose and septum lead to a significant deterioration in the aesthetic result and disruption of nasal breathing, and breathing through the mouth in such patients aggravates the deformation of the facial skeleton.
How to remove surgical sutures at home?
Time frame for suture removal:
- 12 days - for amputation
- after 6 days - during surgery in the area of the skull and head
- after 7 days - after shallow intervention in the peritoneum and 9-12 - after deep surgery
- 10-14 days – for breast surgery
- 14 days - for surgical intervention of elderly people, patients with weak immunity and cancer patients
- 7-10 days - after cesarean section
How to remove surgical sutures at home?
For more information on how to remove suture material yourself, watch the video.
How are surgical sutures removed from a finger?
Stitches are also often placed on the fingers. In these places the seams are very small, since the finger area is small.
Features of removing sutures on fingers:
- First, remove the bandage. After this, the wound is disinfected.
- After this, it is worth sterilizing all instruments. Using tweezers, pull the end of the thread towards you.
- Run the scissors through the loop and cut it. When using tweezers, carefully remove the suture material.
- Treat the scar with brilliant green.
How are surgical sutures removed from a finger?
Possible complications
Cheiloplasty is considered a fairly simple operation. After it, complications occur extremely rarely. The most common problem is severe swelling and hematomas. For several days the patient may experience difficulty eating and drinking.
If hygiene rules are not followed during the rehabilitation period, a bacterial infection may occur. The main symptoms of which are increased swelling, increased body temperature, severe pain, and separation of purulent masses in the operated area. However, this is not possible if all the above recommendations are followed.
How are surgical sutures on the leg removed?
The stitches on the leg should be removed a little later. Usually this is 9-12 days after the intervention. In these places, the skin slowly regenerates and grows together. In addition, the timing of removal of suture materials depends on how well everything is with the wound. If it is clean, the suture material is removed faster.
Features of removing stitches from the leg:
- Most often, the wound is stitched using silk or synthetics. Such threads are strong and ensure rapid healing of the wound edges. They are very easy to remove.
- You need to pull the edge of the thread, and when you see a loop and a knot, cut the thread.
- Gently pull the thread with tweezers, holding the skin. If the wound is large, the stitches are removed in two steps with an interval of several days. Stitches are removed one at a time.
- Often staples or wires are used instead of threads. It is better to remove them at the clinic. This is due to the rigidity of the material and the possibility of repeated damage to the epidermis.
How are surgical sutures on the leg removed?
How are surgical sutures on the lip removed?
The skin on the lips is quite delicate and thin. In this area, neat cosmetic sutures are applied. It is worth noting that such sutures are not made with self-absorbing threads, as they can tighten the skin.
Features of removing sutures from the lip:
- There is a mucous membrane in the lip area. Sutures are removed on the 8th day after their application.
- To begin with, the wound is treated with an antiseptic. After this, the seams are cut and the threads are carefully removed.
- It is necessary to hold the skin to prevent it from stretching and the seams from coming apart.
- After the manipulation, the scar is processed. By the time the stitches are removed, the swelling should disappear.
How are surgical sutures on the lip removed?
How are sutures removed after eye surgery?
The technique for removing stitches in front of the eyes is completely different from stitches on the body. The fact is that the mucous membrane is very sensitive. After surgery for astigmatism, the sutures are removed no earlier than after 3 months.
Features of suture removal after eye surgery:
- The sutures are removed directly from the eyeball no earlier than after 3 months.
- It all depends on the patient’s well-being. You can definitely say about the advisability of removing sutures after examination by an ophthalmologist.
- Ideally, sutures are removed from 3 to 12 months after the intervention. Further, the threads dissolve on their own, but can cause a lot of inconvenience.
- If the threads break, irritation and tearing may occur.
How are sutures removed after eye surgery?
How are surgical cosmetic sutures removed?
After lacerations or cuts, cosmetic surgical sutures are often applied. How carefully you remove the stitches will determine how the scar will look.
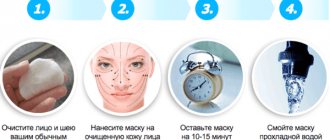
The procedure for removing sutures after surgery:
- First, remove the bandage; do not tear off the patch or gauze that has dried. Pour peroxide over the dressing and wait until everything gets wet. Carefully remove the bandages.
- Now, using tweezers, gently pull the thread, when the suture material is taut, insert the nail scissors and cut the thread.
- Now use tweezers to carefully remove the threads. Hold the skin with a napkin so that it does not stretch. Otherwise, the seam may come apart.
How are surgical cosmetic sutures removed?
Preparing for surgery
To exclude possible contraindications, a set of studies is prescribed:
blood and urine tests, tests for coagulation and infections;
Fluorography or x-ray of the chest organs;
ECG;
Duplex scanning of the veins of the lower extremities.
Test for COVID-19
The therapist's conclusion based on the examination results
Especially for patients of Azimova Early, a 10% discount is provided on all necessary tests, except COVID-19 and fluorography. Valid in a specific medical center.