Laparoscopic reconstructive metroplasty is a surgical procedure aimed at eliminating the incompetence of the uterine scar. The operation consists of excision of the existing pathological scar and the formation of a full suture, which leads to restoration of the integrity of the uterine wall.
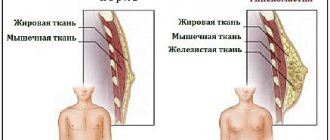
Normally, the wall of the uterus is made up of muscle tissue, which can stretch during pregnancy and contract during labor. But after damage to the wall of the uterus during diagnostic or surgical interventions, muscle fibers can be replaced by areas of connective tissue that are not able to stretch - in this case we are talking about an incompetent scar on the uterus; Most often it is caused by cesarean section. In case of repeated pregnancy, the presence of an incompetent scar is an indication for operative delivery, which quadruples the risk of complications compared to natural birth.
In our clinic, a woman with an incompetent uterine scar, after treatment, has the opportunity to give birth to a child through the vaginal birth canal thanks to reconstructive metroplasty. The operation is performed laparoscopically - all manipulations by the surgeon are performed through three small incisions on the abdominal wall, which after healing become invisible. Moreover, unlike open surgery on the uterine scar, which is accompanied by the risk of bleeding due to the numerous vessels located in this area, laparoscopy of the uterine scar is a low-traumatic surgical procedure and eliminates blood loss.
Find out the cost by phone: +7 (495) 782-50-10
Duration about 60-90 minutes
Time in hospital 3-4 days
Types of scars after cesarean section
By nature, scars after cesarean section are of two types:
- hypertrophic - a compaction that rises above the skin in the form of a roller and is colored pink;
- keloid - an elastic scar that protrudes significantly above the skin, has a purple color and an uneven surface, and can cause pain, burning, itching.
Depending on the intervention technique, scars are also of two types:
- horizontal - remain in 90-95% of cases, reach 10-12 centimeters in length, heal quickly and are more favorable for correction;
- vertical - performed along the midline of the abdomen only for special indications, they take a long time to heal, and are more difficult to correct.
Doctor's comment
Are you worried about the upcoming operation to remove an incompetent scar on the uterus? However, the proprietary technique used in our clinic excludes the development of any complications during the intervention. Thanks to the practiced methods of anesthesia and modern painkillers, the patient does not experience pain either during metroplasty or after removal of the uterine scar. The laparoscopic method used in our clinic also makes it possible to reduce the length of hospitalization to a minimum; after 1.5 months you can return to your usual physical activities. But the most important thing is that after treatment of the uterine scar, it becomes possible to carry and give birth to a child naturally. If you are just planning an examination, in our clinic you can undergo all the necessary procedures, after which treatment tactics will be selected taking into account the characteristics of your body. Do not delay treatment, because correct diagnosis and timely correction are the first step to happy motherhood!
Head of the surgical service at SwissClinic Konstantin Viktorovich Puchkov
How is the operation to remove a scar after a cesarean section performed?
Plastic surgery of scars and scars on the abdomen is performed under general or local anesthesia. The method of intervention is chosen individually, depending on the type of scar and on accompanying operations with which plastic surgery can be combined. As a rule, during correction, the surgeon excises the scar, aligns the edges of the wound and applies a cosmetic suture.
Often, scar plastic surgery after a cesarean section is combined with abdominoplasty - a tummy tuck, or liposuction - local removal of fat deposits. An integrated approach allows you to get rid of overhanging fat and skin tissue in the scar area.
Advantages of laparoscopic reconstructive metroplasty
- Low-invasiveness - thanks to the use of video endoscopic equipment, only the scar is excised, the surrounding tissues are minimally affected
- No blood loss
- Reliable suturing - thanks to the author’s technique used, pregnancy and childbirth naturally become possible in the future
- The use of anti-adhesive barriers during surgery on the uterine scar reduces the risk of formation of adhesions
- Short rehabilitation period and minimal hospitalization period
- Fast recovery after
- Excellent cosmetic result - only three barely noticeable marks remain on the skin.
FAQ
Do I need special preparation for laparoscopic reconstructive metroplasty?
A few days before surgery for uterine scar failure, a woman should, in consultation with her doctor, avoid taking medications that affect blood clotting. You also need to avoid foods that cause excessive gas formation. Metroplasty is performed on an empty stomach, with the last meal and water taken eight or more hours before.
How is laparoscopic reconstructive metroplasty performed?
During the operation, to prevent blood loss, atraumatic clamps block the blood flow, after which, under the control of video endoscopic equipment, the scar tissue is excised, while it is possible to visualize the boundaries of healthy tissue and layers of the uterine wall - which allows all manipulations to be carried out with high precision. When suturing the wound, absorbable suture material is used, and modern anti-adhesive barriers are used to prevent the formation of adhesions, which is important for preserving the patient’s fertility. Finally, the clamps from the vessels are removed, and blood flow is completely restored.
What to expect after laparoscopic reconstructive metroplasty?
Bloody discharge can last up to 10 days, in the first couple of days it is intense, it gradually becomes insignificant. In the first week, the temperature may rise to 38°C. Each patient is under the supervision of staff; the condition of the scar is also monitored by ultrasound specialists.
What types of reconstructive metroplasty are there?
There are several methods of performing the operation: transabdominal - through the anterior abdominal wall: the intervention can be performed by laparotomy (open method) and laparoscopy (through three small punctures), as well as transvaginally. Each technique has its own indications, but laparoscopic metroplasty is the least traumatic method.
Are there any disadvantages to laparoscopic reconstructive metroplasty?
The scar is located in an area with good blood supply, which is accompanied by the risk of intraoperative bleeding. If events develop in this way, it may be necessary to switch to an open method. In addition, the seam formed is less reliable. However, thanks to the use of the author’s technique in our clinic, such problems can be successfully eliminated.
How is the rehabilitation going?
Already on the first day the patient begins to get out of bed, on the second day light food is allowed. In the first days, anti-inflammatory and antibacterial drugs are prescribed. Discharge is possible on the third day. Showering is allowed 5-7 days after surgery. A week after the operation, an ultrasound is performed, and follow-up examinations are scheduled after 1, 3, 6 months. For better recovery, the patient is prescribed hormonal medications for a period of 3-6 months. In the first 4-6 weeks, physical activity should be avoided; normal activity is possible after 1.5-2 months. During the first month, it is also recommended to abstain from sexual relations and visiting the pool. It is better to plan pregnancy no earlier than 6-8 months after the end of treatment.
Management of pregnancy and childbirth in the presence of a scar on the uterus
Patients with a uterine scar should be registered at the antenatal clinic from the earliest stages of pregnancy. Each of them must be carefully examined to develop further obstetric tactics. The doctor is obliged to inform this woman about possible complications during pregnancy and childbirth, as well as about possible methods of delivery. During the examination, special attention should be paid to data that are essential when choosing tactics for managing pregnancy and childbirth. These include:
- indications that served as the basis for performing the first operation;
- gestational age at which the first cesarean section was performed;
- surgical technique;
- the course of the postoperative period and complications (if they occurred);
- features of menstrual function after cesarean section;
- data on generative function after surgery (number of pregnancies, their outcomes);
- the period of time elapsed from the moment of cesarean section to the onset of the subsequent pregnancy;
- surgical interventions on the uterus in the period after cesarean section.
It is advisable to familiarize yourself with an extract from the history of childbirth that ended in abdominal delivery.
Particular attention should be paid to pregnant women whose placenta is localized in the scar area.
Considering the causes of intrauterine fetal hypoxia in pregnant women with a uterine scar, it is necessary to assess the condition of the fetus.
The study should be comprehensive and dynamic in nature using ultrasound, Dopplerography, CTG at least 3-4 times during pregnancy. If signs of intrauterine fetal hypoxia are detected, it is necessary to begin timely corrective therapy aimed at improving uteroplacental and fetoplacental blood circulation.
Assessment of the condition of the uterine scar during pregnancy
Information about the condition of the postoperative scar on the uterus obtained from:
- based on anamnestic data and available documentation;
- methods of hysterosalpingography and hysteroscopy before the onset of real pregnancy;
- when examining a woman during a given pregnancy;
- when assessing the nature of the course of this pregnancy.
The scar most often fails in women who have undergone a minor cesarean section or cesarean section with a corporal incision.
After a cesarean section performed against the background of the onset of labor, the prognosis for the consistency of the scar is better than after an operation performed before the onset of labor. This is explained by the fact that the incision on the uterus during childbirth is usually made lower due to shortening or smoothing of the cervix and in the presence of a formed lower uterine segment. A lower location of the scar has less impact on the course of subsequent pregnancy and reduces the risk of possible uterine rupture.
It is more likely that there is a defective scar if inflammatory complications develop after a cesarean section, especially with a prolonged febrile course and suppuration of the abdominal wall. It should be borne in mind that a smooth course of the postoperative period does not guarantee a full-fledged scar. A decrease in the body's defenses in the postoperative period can disrupt normal tissue regeneration.
Unfavorable factors for the formation of a postoperative scar include uterine curettage. Abortions performed in the interval after a cesarean section before the onset of a real pregnancy also worsen its prognosis, since the wall of the uterus and its nervous apparatus are injured. The risk of scar failure increases by 1.5 times.
The indications for the first cesarean section and the accompanying diseases are of no small importance. Incomplete repair of the dissected uterine wall most often results from severe gestosis, previa and premature abruption of the normally located placenta, obesity, anemia, and chronic infectious diseases (as a result of immunodeficiency). Unfavorable factors are conditions associated with hyperextension of the lower uterine segment: clinically narrow pelvis, incoordination of labor, incorrect insertion of the fetal head.
When examining a pregnant woman, it is necessary to pay attention to the characteristics of the skin scar, taking into account its width, relationship to the underlying tissues, and pain on palpation. If the scar on the skin is thin, soft, and not fused with the underlying tissues, that is, there is reason to assume the presence of a full-fledged scar on the uterus.
Important information can be obtained by palpating the uterine scar through the anterior abdominal wall.
If the scar is defective, its thinning or pain in one of the areas is determined. It should be remembered that sometimes an aponeurosis defect can be mistakenly mistaken for a scar defect. To avoid mistakes, the scar on the anterior abdominal wall should be shifted slightly.
It is important to determine the localization of the placenta using ultrasound, since its location on the anterior wall in the area of the scar makes it potentially defective.
Certain information about the condition of the uterine scar can be obtained by ultrasound. The most optimal period of pregnancy for the study is from 28 to 37 weeks. It is during this period of time that the lower segment of the uterus is sufficiently formed, the presenting part is not yet pressed against the entrance to the pelvis, and the amount of amniotic fluid is optimal for the study.
Ultrasound allows one to evaluate the shape, thickness of the lower segment of the uterus, the echostructure of the myometrium in this section of the uterus, and the nature of the contour of its anterior wall.
The thickness of the full lower segment of the uterus on ultrasound is at least 4-5 mm. In the area of the former incision, as a rule, there is a homogeneous echostructure, corresponding in acoustic density to the normal wall of the uterus
A defective scar after a corporal cesarean section is defined as a defect in the muscle wall with a thickness of 1/2 to 1/3 of the myometrium. Much more difficult to diagnose is a transverse scar in the lower uterine segment, in which local thinning may also be observed.
The reliability in recognizing the condition of the scar is 56-76%. It is advisable to carry out an echographic examination with a full bladder.
Hospitalization of pregnant women with a scar on the uterus
Pregnant women with a scar on the uterus are subject to planned hospitalization in a maternity hospital at 35-36 weeks. The patient must have with her an extract from the outpatient card about the indications for the previous operation, the method of uterine dissection, the course of the postoperative period, examination data outside of pregnancy, the nature of the course of this pregnancy and examination data during this pregnancy.
In the hospital, the general and obstetric history is thoroughly analyzed. Particular attention is paid to inspection and palpation of the scar. In addition to general clinical research methods, it is necessary to conduct CTG and ultrasound with Dopplerography. The examination should be carried out fairly fully and quickly, drawing up a detailed plan for the management of pregnancy and childbirth, determining the method of delivery, taking into account possible complications and ways to prevent them.
Features of childbirth in women with a uterine scar
Delivery through vaginal birth canal
The most significant limiting factor in managing vaginal delivery in women with a uterine scar is the danger of uterine rupture along the scar and the lack of complete confidence in its usefulness.
Nevertheless, from 1/2 to 2/3 (30-70%) of pregnant women with a uterine scar after a cesarean section can potentially give birth on their own.
However, in 9-30% of cases during childbirth in the presence of a scar on the uterus, complications arise that force us to reconsider the tactics of labor management in favor of an emergency cesarean section. Most often, such complications include anomalies of labor, deterioration of the fetus, a clinically narrow pelvis, and the appearance of symptoms of incompetent scar on the uterus.
Conducting childbirth through the natural birth canal in the presence of a scar on the uterus is considered acceptable if a number of conditions are met, which are selection criteria for conducting such childbirth:
- one history of cesarean section with a transverse incision on the uterus in the lower segment;
- absence of obstetric complications that served as indications for the first operation (indications are not repeated);
- uncomplicated course of the postoperative period in the anamnesis;
- assumption about the usefulness of the lower uterine segment (based on the results of clinical and instrumental studies);
- localization of the placenta outside the scar on the uterus;
- cephalic presentation of the fetus;
- correspondence between the sizes of the mother’s pelvis and the fetal head;
- careful clinical and monitoring observation during childbirth;
- availability of conditions for emergency delivery by cesarean section, qualified medical personnel and appropriate equipment;
- the ability to perform an emergency caesarean section no later than 15 minutes after the decision to operate is made;
- management of childbirth in a full operating room.
Careful monitoring of the contractile activity of the uterus using monitor control is required.
Controlled by:
- duration of contractions;
- intensity of contractions;
- rhythm of contractions;
- duration of the interval between contractions;
- coordination of contractions;
- the presence of a dominant uterine fundus;
- duration of pain.
Features of the course and management of labor
In the presence of a full-fledged lower uterine segment, the preparatory period in these women does not differ from that in non-operated patients.
As a rule, contractile activity is in the nature of normal contractions. Childbirth proceeds according to the standard biomechanism characteristic of first- or multiparous women. The average duration of labor has also remained virtually unchanged. Average blood loss may slightly exceed that during vaginal delivery.
Most often, childbirth in women with a uterine scar is complicated by:
- untimely discharge of amniotic fluid;
- weakness of labor;
- clinical discrepancy between the sizes of the mother’s pelvis and the fetal head;
- manifestation of signs of threatened uterine rupture.
The frequency of postpartum hypotonic bleeding ranges from 1.5 to 10.5%, the pathology of placental separation is 0.5-4%, which is slightly higher than similar indicators in the general population.
These complications are explained by the fact that the operated uterus is characterized by slightly reduced contractile activity, and the previously mentioned changes in the anterior wall of the uterus contribute to deeper trophoblast invasion and more dense attachment of the placenta.
The onset of labor can be spontaneous or programmed, i.e. it is permissible to perform an amniotomy in the presence of a “mature” cervix. To prepare the body for childbirth and induce labor, it is permissible to use drugs in the form of a gel based on PGE2.
It is possible to use uterotonic drugs (oxytocin and prostaglandin preparations) during childbirth if it is necessary to induce labor after amniotomy or prenatal rupture of amniotic fluid (in the presence of a “mature” cervix), or for labor stimulation.
During labor and delivery, continuous cardiac monitoring of the fetal condition is necessary. Signs of deterioration in the fetus' condition may indicate incipient uterine rupture. Often this symptom is the first in this pathology.
Pain relief for labor in women with a uterine scar is carried out according to generally accepted rules, including the use of epidural anesthesia. The opinion that the use of this type of anesthesia smoothes out the clinical symptoms of incompetent uterine scars and complicates the diagnosis of the threat of uterine rupture has not been confirmed as a result of the studies. At the same time, there was no increase in the number of uterine ruptures, the frequency of emergency cesarean sections, or an increase in maternal and perinatal morbidity and mortality.
If the second stage of labor is prolonged or fetal asphyxia has begun, delivery must be accelerated by dissecting the perineum.
Manual examination of the uterus immediately after birth is mandatory, since the possibility of spontaneous uterine rupture along the scar cannot be ruled out. Signs of uterine rupture may appear a considerable time after delivery. In addition, it is important to have an idea of the condition of the uterine scar in order to decide on the tactics of labor management in the future. This operation must be carried out with extreme caution, since its rough execution is often the cause of uterine rupture.
Abdominal delivery. Possible complications
The vast majority of women with a uterine scar are delivered by repeat cesarean section.
The proportion of abdominal delivery due to the presence of a scar is 30-70%.
Until recently, there was an opinion about the advisability of delivering such patients 10-12 days before the expected due date, i.e. at the 38th week of pregnancy, which naturally simplifies obstetric tactics. This practice leads to a sharp deterioration in the prognosis for the fetus. Taking into account the peculiarities of the course of the newborn period after repeated cesarean section at 38 weeks, just as reasonable indications for abdominal delivery are required as in earlier periods.
It is necessary to take into account the fact that in children removed by repeated cesarean section at this time, with sufficient weight and length, signs of morphofunctional immaturity are often observed. The risk of respiratory diseases in these newborns is more than 35%, including respiratory distress syndrome and hyaline membrane disease.
In this regard, to improve the outcome of pregnancy, it is advisable to perform a repeat operation (if appropriate conditions exist) at a time as close as possible to the expected date of birth.
As planned, pregnant women are allowed to give birth ahead of schedule only with suspected failure of the uterine scar.
Before early delivery, it is advisable to prevent distress syndrome with steroid drugs (dexamethasone, etc.). It should be remembered that such prophylaxis can have a certain effect if it lasts 2-3 days.
In all cases, repeat caesarean section is an operation of particular complexity and risk.
The features of this operation include common difficulties with:
- dissection of the abdominal wall due to adhesions with underlying tissues;
- access to the lower uterine segment due to adhesions in the abdominal cavity;
- extraction of the fetus due to scar deformation of the anterior wall of the uterus.
When accessing the uterus, one of the possible complications is injury to the bladder.
In this regard, the parietal peritoneum should be opened as high as possible. The surgeon performing a repeat cesarean section must be proficient in the technique of suturing bladder wounds.
When the uterus is dissected in the lower segment, given its cicatricial deformation, the incision may extend into the area of the uterine vessels and cause injury to them.
One of the complications of repeat cesarean section is hypotonic bleeding as a result of impaired contractility of the uterus. Hypotonic bleeding can sometimes be associated with both the indications for surgery and the conditions for its implementation.
Repeated cesarean section is often accompanied by increased blood loss and increased duration of the operation, which increases the risk of developing postoperative purulent-inflammatory complications.
After a repeat cesarean section, there is a decrease in the adaptation of newborns, which dictates the need to include them in a high-risk group for the development of complications in the neonatal period. Perinatal losses during repeat caesarean section average 12-13%.
The prognosis for the next pregnancy after a cesarean section is determined by a number of factors:
- woman's age;
- the presence of concomitant diseases;
- the nature of the course and management of the previous and current pregnancy;
- indications for cesarean section;
- the technique of performing the operation and the quality of the suture material;
- course and management of the postoperative period.
Efforts to improve prognosis should be targeted immediately after the decision to perform a first cesarean section is made. The quality of scar healing is affected by:
- dissection of the uterus in the lower segment;
- creating a tight, hermetic and long-lasting connection between the edges of the wound on the uterus with a minimal inflammatory reaction from the surrounding tissues (this largely depends on the method of suturing the incision on the uterus and the quality of the suture material);
- adequate prevention of purulent-inflammatory diseases after cesarean section.