Clinical manifestations of rosacea
The disease begins after 25-30 years. First, there is a tendency to frequent redness of the face, less often the neck and décolleté. “Burst blood vessels” (telangiectasias) appear. Then the redness in some areas becomes persistent. Subsequently, inflammation, peeling, and rashes (outwardly resembling pimples) may develop at the site of persistent redness. Without treatment, the number of such elements increases. Dryness and redness of the eyes often develop. In a small proportion of patients, with age, the so-called rhinophyma develops, a thickening and growth of the skin of the nose (“bumpy nose”).
Types of rosacea: A - Erythematotelangiectatic rosacea, B - papulopustular rosacea, C - rhinophyma, D - ocular rosacea. Photo: Dermatology Reports / Open-i (CC BY-NC 3.0)
The cause of rosacea is impaired vascular tone of the face and inflammation in the vascular wall. They can be caused by various factors: hormonal disorders, characteristics of psycho-emotional status, diseases of the cardiovascular or digestive system, microbial factors. A doctor must understand the possible causes of the development of rosacea in a particular person and analyze the degree of influence of a particular health feature. The main task is to minimize external and internal factors that aggravate rosacea, and to directly affect the blood vessels of the face. Treatment regimens are chosen by the doctor; they are strictly individual in nature.
Photo: Dermatology and Therapy / Open-i
Age-related changes in facial skin in men
Services Doctors Results Reviews
Expert tested
Natalya Borisovna Zhmurina Director, Chief Physician of “A Clinic” Dermatovenereologist, cosmetologist
Publication date: March 06, 2022
Review date: November 22, 2022
External manifestations of age-related changes in men in the period from 27 to 35-37 years are practically invisible. This is due to the structural features of male skin. Men's skin has more intense blood circulation. It has more hair follicles, sebaceous and sweat glands, which contributes to good protection and nutrition. In general, thanks to these factors, greater thickness and higher content of collagen types IV and VI, signs of skin aging in men are invisible for a very long time.
But with the onset of 40-43 years of age, precisely because of the thickness and density, the changes that occur are expressed more clearly. The wrinkles that appear are prominent and have the appearance of “deep furrows.” Unlike women's wrinkles, men's wrinkles are much more difficult to correct and require longer treatment.
In addition, with age, a more pronounced change in the oval of the face occurs, Jowls form, the formation of hernias of the upper and lower eyelids, skin folds and bags under the eyes is observed. The face begins to “float”. This process is called gravitational ptosis, and it is caused by changes in the density and quality of collagen fibers in the skin.
One of the key reasons for changes in men's skin with age is the gradual, starting from the age of 35, and accelerating towards the age of 40-45, a drop in the level of male sex hormones. Since they stimulate the sebaceous and sweat glands, men's skin becomes significantly drier with age. There is also an increase in the fragility and fragility of blood vessels, as a result of which the sensitivity of men's skin increases significantly with age. As a result, with constant shaving, irritation from skin damage and inflammatory processes last longer and are more difficult to treat.
By the age of 35-40, the weakness of the walls of small vessels of the facial skin becomes noticeable. A persistent vascular network appears on the face, which gives the face an unhealthy, red-violet tint. This process is enhanced by the systematic consumption of strong alcohol. At its maximum, this process is called rosacea.
After 45-50 years, all of the above processes intensify. Skin density begins to decrease due to changes in collagen composition. The skin becomes flabby and loose. Hernias of the upper and lower eyelids, bags under the eyes develop or intensify, and a double chin appears or increases in size. The volume of fluid retained by the body also increases, so the face becomes swollen and puffy. An uneven decrease in the secretion of sebaceous and sweat glands causes local dryness in combination with local oily skin.
What happens in the skin?
Redness, no matter what causes it, represents increased blood flow to the skin. The vessels dilate greatly and contract with difficulty. Some of the fluid from the overcrowded vessels can seep into the surrounding tissues - swelling occurs.
Proteins and blood cells may also leak out. The condition of connective tissue fibers and muscles that help blood vessels contract and drain blood and lymph from the skin deteriorates. Stagnation and low-grade inflammation occurs in and around the vascular wall. Opportunistic and pathogenic microorganisms can join this inflammation, which weakens the skin’s defenses.
Rosacea treatment
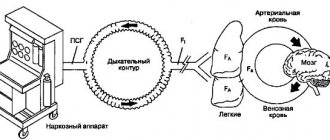
Treatment of rosacea using intense pulsed light (IPL) technology.
Photo: BioMed research international / Open-i (CC BY 3.0) Therapy for this disease depends on the totality of manifestations and characteristics of a particular person. There is a classic treatment regimen for rosacea, accepted in dermatology. These are antibiotics, metronidazole, retinoids, antihistamines, local therapy.
Creams, gels, ointments containing azelaic acid, metronidazole, retinoids, pimecrolimus, and antibiotics are used topically. Treatment lasts several months. As prescribed by a doctor, various combinations of medications and their alternation can be used. Historically, ointments and pastes with ichthyol, tar, sulfur, and salicylic acid were widely used. Often they are still used today due to their low price, but all these products irritate the skin.
The main treatment should be aimed at eliminating provoking factors and restoring the normal state of blood vessels. Triggers vary from person to person, but the clear leader is excessive emotional reactions.
Burning neck: causes, diagnosis and treatment
The pain is localized in the back of the neck and can spread to the right or left side. Turning the head is accompanied by sharp pain.
Causes of burning in the neck
The most common cause of this symptom is cervical osteochondrosis.
This indicates degenerative changes in the cervical spine.
Causes of osteochondrosis:
- Genetic predisposition.
- Previous spinal injuries.
- Excess body weight.
- Infectious diseases.
- Hormonal disorders (more often in women).
- Poor nutrition.
- Sedentary lifestyle.
- Uncomfortable bed and pillow.
Classification:
- Visceral pain.
- Somatic superficial and deep.
Depending on the affected part of the nervous system:
- Central
- Neuropathic
Because of:
- Associated with damage to the spinal column (osteochondrosis, vertebral hernia, arthrosis, whiplash, protrusions).
- Other etiologies: infectious diseases, endocrine disorders, tumor processes.
Diagnostics
When a patient consults a doctor with complaints of a burning sensation in the neck, he is prescribed a number of the following diagnostic procedures:
- X-ray - allows you to identify some degenerative changes in the spinal column, detect pinched nerves or the spinal cord.
- Computed tomography (CT) is a series of layer-by-layer images of the internal parts of the neck.
- Magnetic resonance imaging (MRI) - an image is obtained using a magnetic field and radio waves.
- Electromyography – used to measure the speed of nerve impulses. It is carried out by piercing the muscle through the skin and delivering impulses.
- Ultrasound diagnostics (ultrasound) - used to check the condition of the vascular bed and nearby soft tissues.
- Electrocardiography (ECG) is necessary to exclude myocardial infarction.
- Blood test - to identify infectious processes.
Which doctor should you contact?
In addition to a burning sensation in the neck, there are a number of other symptoms indicating osteochondrosis. Compression of the neck vessels may develop, which disrupts the blood supply to the head and brain. As a result, a number of the following symptoms occur:
- Blood pressure surges.
- Nausea and vomiting.
- Regular and severe headaches.
- Feeling of spots before the eyes.
- Dizziness and fainting.
If you have these symptoms, it is recommended to consult a general practitioner and neurologist.
Symptomatic treatment
The main methods of treatment are the combined use of medications and non-drug treatment (massages, physiotherapy).
Medicines
Mandatory part of treatment. The use of drugs helps relieve inflammation and relax muscles.
Types of drugs:
- Anti-inflammatory - Diclofenac, Ketoprofen, Meloxicam.
- Muscle relaxants – “Mydocalm”, “Sirdalud”, “Baklosan”.
- Neuroprotectors – “Berlition”.
- Chondroprotectors – “Teraflex”, “Arthra”, “Stoparthrosis”.
Massage
An important part of the treatment of the cervical spine is massage.
Basic massage techniques:
- Massage of the collar area - this procedure is not difficult and does not require special equipment. The patient should squat and lean forward. The body should be completely relaxed. The person performing this procedure for you should rub and stroke the neck muscles in the problem area with gentle movements.
- Acupressure – this manipulation should be performed by a professional. The essence of this massage technique is to massage individual points of the skin. This type of influence, when performed correctly, leads to the proper therapeutic effect.
- Self-massage – this massage option is the simplest and most accessible. No special training or outside help is needed. You must massage the problem area of your neck yourself. Movements should be smooth, soft, neat.
Physiotherapy
Along with drug treatment, physiotherapy is an important component.
This method includes the following manipulations:
- Electrophoresis is the introduction of drugs into the body by exposure to electric fields and currents. Helps relieve pain and muscle spasms.
- Magnetotherapy - a method based on the use of constant and alternating magnetic fields. The main effect is a reduction in inflammation and elimination of pain.
- Ultrasound – the impact of ultrasound on problem areas helps relieve pain and reduce inflammation.
- Laser therapy is carried out using a special laser that affects the nerve roots of the spinal cord and the paravertebral part of the affected areas. Reduces pain and eliminates inflammation.
- Balneotherapy is based on the use of therapeutic mud. The substances contained in the mud affect the receptors of nerve endings and contribute to a speedy recovery of the patient.
Prevention
To avoid a burning sensation in the neck area, you must follow a number of rules:
- Quitting bad habits (smoking, alcohol, etc.).
- Lead a healthy and active lifestyle.
- Avoid excessive physical activity.
- Eat a balanced and healthy diet.
Conclusion
If you notice a similar symptom, consult a doctor as soon as possible. A timely visit to a specialist will help get rid of this problem and avoid further complications.
The doctor will prescribe specialized treatment, which includes: massage, medications and physiotherapy.
It is also worth following the basic rules of prevention to avoid the occurrence of such a problem.
Author: K.M.N., Academician of the Russian Academy of Medical Sciences M.A. Bobyr
Physiotherapy has all these qualities.
The first stage of therapy, the longest, is to reduce swelling and inflammation in and around the vascular wall. Two methods are suitable for this. Laser-magnetic therapy is a combination of red and infrared laser radiation with a constant magnetic field. A powerful anti-edematous and anti-inflammatory effect on the vascular wall promotes the outflow of excess blood and lymph from the face.
Mens therapy, better known as microcurrent . A mild anti-inflammatory effect, restoration of normal tone of the neuromuscular system that regulates vascular contraction, normalizes vascular reactions to external influences.
Both procedures are prescribed 2 times a week, a total of at least 12-20 procedures are required. Depending on the prevalence of specific symptoms, you can start with microcurrent (redness and hot flashes predominate) or laser-magnetic therapy (swelling and inflammation predominate). For optimal results, it is advisable to use both methods. The procedures are inexpensive and painless, but require regular visits to the doctor (2 times a week for 30-40 minutes). The earlier treatment is started, the more effective and shorter it will last. After the procedures, maintenance therapy is prescribed.
In addition to physical therapy, medications may be prescribed that are selected individually. Efficacy is assessed as treatment progresses; drugs may be changed or combined.
Second phase. After stabilization of the situation, persistently dilated vessels that cannot be eliminated by therapeutic methods are removed.
One of the most effective and gentle methods for removing “vessels” is the use of a neodymium laser with a short powerful pulse. Delivery of such a pulse with an absorption spectrum in oxyhemoglobin (a blood component) promotes the removal of blood vessels without damaging the surrounding tissue.
Cheeks are burning and blushing. What do rosy cheeks tell the doctor?
A ruddy complexion has long been considered an indicator of good health. But is it only the blush on the cheeks that can signal this? Why does he appear?
How's normal?
The facial area is rich in blood vessels of different diameters. Usually small vessels are not clearly visible, and therefore the complexion is pale or slightly pinkish.
The reason for the appearance of blush on the cheeks and redness of other areas of the face can be exposure to the cold. Blushing occurs at elevated temperatures, in a stuffy room. Drinking red wine or hot pepper will also add redness to our cheeks.
Could blush be a sign of pathology? It turns out yes. Let's briefly look at some of them.
Increased body temperature. Of course, not every infection is accompanied by fever, but, for example, for widespread colds, this symptom is not uncommon. Do you see the blush on your cheeks? Measure your body temperature - perhaps the cause is a feverish state. In this case, there are often other manifestations: general weakness, deterioration or lack of appetite, body aches, cough, runny nose, as well as other symptoms characteristic of a particular disease.
Read the material on the topic: What is ARVI?
Scarlet fever. A relatively rare infectious pathology today. The group A streptococci that cause it secrete a special toxin that leads to diffuse redness of the skin with a pinkish-red tint. With scarlet fever, fever, skin rashes, and a crimson-red color of the tongue are noted.
Remember that elevated body temperature can indicate not only infectious diseases: it also occurs in diseases that are not in any way related to infections.
Another cause of facial redness is overheating .
An unhealthy blush may indicate an allergy .
Rosacea. With this disease, the vascular network grows, the skin on the face thickens. In addition to redness, nodules and pustules appear on it, itching is noted, and the secretion of sebum increases. One form of this disease is rhinophyma, when the skin on the nose thickens significantly.
The facial skin also turns red with various dermatitis and acne.
Itsenko-Cushing syndrome . Develops with excessive release of glucocorticoids (a type of hormone) - for example, a neoplasm of the adrenal gland, a lipid cell tumor of the ovary; prolonged administration of drugs containing glucocorticoids (in this case, drug-induced Itsenko-Cushing syndrome occurs).
Manifestations of pathology include obesity; rounding the contours of the face; red-violet “stretch marks” on the skin of the abdomen and thighs; increased blood pressure and a number of others.
Systemic lupus erythematosus (SLE). It develops when cells and tissues are attacked by their own antibodies and immune complexes. The manifestations are varied. In addition to the “butterfly” flush of the cheeks, joint pain, fever, malaise, damage to the oral mucosa, and often widespread or local hair loss are noted. An increase in various groups of lymph nodes is often observed (especially in children and young people); in 10% of patients, an enlargement of the spleen is detected.
Read the material on the topic: What diagnostics do you need to undergo before planning a pregnancy?
Damage to the cardiovascular, bronchopulmonary, nervous, digestive systems, kidneys, and hematopoiesis is also possible. In addition, women can have early and late miscarriages. During pregnancy, the disease may worsen.
Mitral stenosis . One of the heart defects. The cause is rheumatic fever. The basis of this disease is a narrowing of the opening between the left atrium and the left ventricle.
High blood pressure . In addition to an objective increase in blood pressure and other symptoms, one of the signs may be redness of the skin of the face.
Read the material on the topic: For what reasons does blood pressure increase?
Diabetes. This disease affects a large portion of the population around the world. Symptoms include: increased thirst, increased frequency of urination and the release of large amounts of urine, general weakness, and fatigue. Sometimes there is an increase in appetite. Possible weight loss, nausea, vomiting, blurred vision. Wounds heal worse, and there is a predisposition to bacterial and fungal infections. Redness of the cheeks is also common.
Read the material on the topic: How to determine diabetes?
Hypothyroidism . A syndrome that develops when there is a lack of thyroid hormones in the body, or a decrease in their biological effect at the tissue level.
Manifestations of hypothyroidism are usually nonspecific. Some of them: increased body weight (even obesity), brittle hair, snoring at night, a feeling of chilliness, swelling under the eyes in the morning, decreased heart rate, constipation, deterioration of memory or attention, depression, depression. In women, the menstrual cycle may additionally be disrupted.
In laboratory tests - an increase in cholesterol levels, a decrease in hemoglobin levels.
Menopause . Due to hormonal changes, among other things, so-called hot flashes may occur, with warming and redness of the skin (especially the face, head and neck).
Polycythemia vera . Chronic pathology of the blood system, which is based on an increase in the total mass of red blood cells. In addition to facial redness, there are symptoms such as general weakness, headache, dizziness, blurred vision, fatigue and shortness of breath. Itching is often observed, especially after a hot bath; enlarged liver, in > 75% of patients - spleen.
Theoretically, facial redness can also occur with increased formation of red blood cells of a different origin.
Erythrophobia (blushing syndrome, erythrophobia, stress flushing of the face) . A type of neurosis characterized by a pathological fear of blushing in the presence of people. This fear itself can cause the skin to become red. It is based on dysfunction of the autonomic nervous system.
Read the material on the topic: Vegetative-vascular dystonia: diagnosis or fiction?
Carcinoid syndrome . It develops when there is a carcinoid in the body - a tumor from a certain type of cell of the neuroendocrine system. There is a rush of blood to the face and neck caused by emotional stress or ingestion of food, hot or alcoholic drinks. Complaints of abdominal cramps and diarrhea are common. There may be a deficiency of vitamins and proteins, and anemia due to deterioration of absorption processes in the small intestine. Damage to the heart valves and the appearance of murmurs are possible; weakened sexual desire and erectile dysfunction.
Taking certain medications can also cause facial redness
What to do?
We have listed some of the possible reasons for this manifestation. To find out what kind of disease a blush on the cheeks and other areas of the face may be a sign of, you must definitely seek medical help. If the situation is not an emergency, you can first consult a general practitioner or therapist. Depending on what diagnosis is made or suspected, consultation with related specialists may be necessary.
Since pathologies relate to different organs and systems, the range of prescribed studies may also be different.
Text: Enver Aliyev
Differences between rosacea and rosacea
Cuperosis.
Photo: evgeniasheidt / freepik.com Cuperosis is the appearance of “bursted” blood vessels (telangiectasia) on the face and body. This may be the initial manifestation of rosacea or an independent disease. The difference from rosacea is that there is no progression in the form of inflammation and the appearance of rash elements. The concern is not so much the persistent diffuse redness as the presence of “vessels”. If rosacea is mild, manifested by single vessels, then treatment is limited to their removal. If the presence of “vessels” is accompanied by “hot flashes” to the face, heaviness and swelling in the legs, etc., you should consult a doctor to have a consultation and find out whether there are signs of rosacea or, if the “vessels” are located on the legs, varicose veins.
The editors thank the specialists of the BioMI Vita clinic for their assistance in preparing the material.
Rosacea: aspects of classification and diagnostic search for transient and persistent facial erythema
Summary. Rosacea is one of the most common facial skin diseases. The clinical picture of rosacea is characterized by redness of the central parts of the face, hot flashes, telangiectasias, less often papules and pustules, and phymatous manifestations. Dermatologists, allergists, therapists, and family doctors deal with redness of the facial skin. In typical cases, diagnosing rosacea is not difficult, but facial redness and hot flashes can be accompanied by many diseases, both benign and malignant. Most cases are caused by very common benign conditions such as rosacea, which are easily diagnosed after a thorough history and examination. However, in some cases, an accurate diagnosis requires further laboratory, radiological or histopathological studies. For example, carcinoid syndrome, pheochromocytoma, systemic mastocytosis, dermatomyositis, systemic lupus erythematosus, anaphylaxis must be excluded by laboratory tests. The article describes the main diseases that must be taken into account when diagnosing transient or persistent erythema in rosacea.
Rosacea is a chronic inflammatory disease of the facial skin, widespread in the population. Rosacea is diagnosed in all races, but most often affects people with white skin (more than 10% of the adult population) [1]. This skin disease is manifested by a complex of various anamnestic and clinical signs, mostly affecting the protruding parts of the face (central part of the forehead, nose, medial part of the cheeks, chin).
The classification of rosacea is based on clinical (phenotypic) features. In the 2002 classification, the variety of clinical signs of rosacea was grouped into 4 subtypes (erythematotelangiectatic, papulopustular, phymatous, ophthalmic rosacea) and 1 variant of rosacea - granulomatous, and also identified the main and additional diagnostic criteria for the disease. The main criteria included unstable erythema, persistent erythema, telangiectasia, papulopustules. The presence of one or more basic criteria indicated rosacea [2].
However, this classification is not specific enough (especially for the erythematotelangiectatic subtype of rosacea), does not take into account the duration of hot flashes, unstable facial erythema, and when using such a basic criterion as “unstable erythema”, differential diagnostic difficulties arise in other conditions accompanied by transient facial erythema (for example, carcinoid syndrome, mastocytosis, connective tissue diseases), or conditions against which telangiectasia develops on the face (for example, mitral valve disease) [3].
In addition to the lack of clearly accurate diagnostic criteria specific to rosacea, one patient may have signs of several of its subtypes, which complicates diagnosis and epidemiological and statistical studies [3].
In 2022, the American National Rosacea Society (Table 1) [4], and in 2022, the International Consensus on Rosacea (ROSacea COnsensus, ROSCO) stated that the classification needs to be updated, to move away from division into subtypes and move on to a phenotypic classification, which specifies the clinical features of rosacea.
Description of clinical signs of rosacea according to ROSacea COnsensus [5]
Diagnostic criteria:
- persistent erythema (centrofacial erythema that periodically worsens in response to triggers);
- phymatous changes (thickening of the facial skin due to fibrosis, hyperplasia of the sebaceous glands, the skin of the nose is most often affected).
Main features:
- hot flushes/transient erythema (temporary increased redness of the central part of the face, which may be accompanied by a sensation of warmth, heat, burning and/or pain);
- papules and pustules (usually in the central part of the face);
- telangiectasia (vessels in the centrofacial area, and not just in the area of the wings of the nose).
Additional symptoms include subjective burning sensations, heat, swelling, and dry skin.
To make a diagnosis of rosacea, one diagnostic criterion or 2 or more basic signs are required.
Diagnosis of erythema
Clinical manifestations of rosacea become complaints more often in the third or fourth decade of life, which prompts the patient to consult a doctor [6]. There are no laboratory markers to confirm the diagnosis (with the exception of a biopsy, which is used in case of diagnostic difficulties), and when making a diagnosis, doctors rely on the clinical picture and anamnestic data. With typical manifestations, clinical diagnosis is usually not difficult.
Despite its high prevalence and typical clinical manifestations, diagnosing rosacea can be challenging, especially during the stage of transient erythema. Having suspected a diagnosis of rosacea in a patient with complaints of hot flashes or clinical manifestations of erythema on the face, it is necessary to carefully collect an anamnesis of life and disease, find out concomitant pathology and its treatment, and in some cases refer the patient to related specialists to exclude systemic or clarify concomitant diseases [6, 7]. In fact, the diagnosis of “rosacea”, based only on a symptom such as transient facial erythema (flushing), should be a diagnosis of exclusion, that is, made only after excluding systemic or concomitant pathology, at the same time it is necessary to understand that rosacea is more common in people with diseases of the cardiovascular, endocrine and nervous systems, gastrointestinal tract, autoimmune pathology [6, 7].
Transient erythema
Transient erythema (hot flashes) is a sharp reddening of the face, accompanied by subjective sensations from warmth to heat and burning on the skin; all this can be caused by heterogeneous pathogenetic mechanisms and various vasodilating factors (Table 2) [6].
Physiological skin flushing is a coordinated thermoregulatory response to hyperthermia, which is accompanied by transient vasodilation. The typical physiological localization of skin redness on the face, neck, upper chest and shoulders is associated with a physiologically increased volume of superficial vessels in this area and characteristics of vascular tone compared to other areas.
Vasomotor innervation of skin vessels is carried out by nerve endings with a vasoconstrictor or vasodilator effect; in most areas of the body one type of action will predominate over the other. The vessels supplying blood to the skin of the face are mainly innervated by vasodilator fibers in the trigeminal nerve, emanating from the brain stem.
Flushing results from increased cutaneous blood flow resulting from vasodilation and is a synchronized physiological response of cutaneous vascular smooth muscle to various vasodilatory stimuli. Redness of the skin can be short-term or long-lasting. Prolonged episodes of redness lead to the development of telangiectasia, a burgundy with a bluish tint to the skin, which is associated with the growth of larger intradermal vessels containing slowly flowing deoxygenated blood.
The smooth muscle fiber of the vascular wall responds to both autonomic innervation and circulating vasoactive agents; changes in any of these factors can result in a high tide. Autonomic nerves also innervate the sweat glands. Thus, disorders of the autonomic nervous system tend to cause vasodilation accompanied by sweating ("wet" flush), whereas vasoactive substances, both endogenous and exogenous, tend to cause only flushing ("dry" flush) (Table 2) [ 6].
Autonomic nerve fiber-mediated flushing syndromes can be divided into:
- thermoregulatory hot flashes (fever, menopause, physical activity, drinking hot drinks, etc.);
- emotional tides;
- hot flashes associated with a disorder of the central nervous system (neoplasms compressing the third ventricle of the brain, spinal cord injuries, multiple sclerosis, Parkinson's disease, auricotemporal syndrome (Frey's syndrome), trigeminal neuralgia, migraine).
Hot flash syndromes mediated by direct vasodilators result from exposure to various exogenous substances that have a direct effect on vascular smooth muscle, or a number of systemic disorders associated with excess production of vasoactive agents.
The most common vasodilatory effects are drugs, alcohol, spicy foods containing capsaicin, nitrate and/or monosodium glutamate, and food histamine liberators (Tables 2 and 3) [6, 7].
It has long been thought that MSG in food causes the flushing reaction as part of MSG syndrome or Chinese restaurant syndrome. However, randomized, placebo-controlled studies have not demonstrated a skin flushing response to MSG at levels used in food. When ingested in large doses, MSG causes an increase in levels of the acetylcholine-like substance, which can cause hot flashes in susceptible people.
Alcohol can cause redness due to the direct dilation of blood vessels in the skin under the influence of ethanol or its metabolite, acetaldehyde. Acetaldehyde causes the release of catecholamines from the adrenal medulla and sympathetic nerves. In addition, some alcoholic drinks, such as wine, contain vasoactive substances (tyramine, histamine and sulfites), which contribute to flushing.
Alcohol is oxidized to acetaldehyde in the liver by alcohol dehydrogenase. The speed of this reaction is a key factor in determining whether flushing will occur. In addition, aldehyde dehydrogenase enzymes, including acetaldehyde dehydrogenase, are also involved in alcohol metabolism and are responsible for the breakdown of acetaldehyde. Acetaldehyde dehydrogenase deficiency, often seen in people of Asian descent, results in severe flushing after drinking alcohol due to the accumulation of acetaldehyde.
Many medications combined with alcohol can increase the hot flush response. Disulfiram inhibits alcohol dehydrogenase and can cause severe flushing, nausea, vomiting and hypotension. It is well known that taking sulfonylureas (especially chlorpropamide) with alcohol causes redness that usually begins around the eyes and extends to the forehead. Other medications that may cause flushing when taken with alcohol include metronidazole, ketoconazole, griseofulvin, cephalosporins, antimalarials, and topical calcineurin inhibitors.
A detailed history and physical examination are important when evaluating a patient's facial erythema. The presence of sweating associated with flushing suggests an autonomic-mediated etiology for hot flashes and distinguishes it from a vasodilator etiology. Some etiological factors for hot flashes, such as alcohol intake, spicy foods, physical and emotional stress, menopause or fever, are widely known. Others (tumors, certain medications, neurological diseases, mastocytosis, anaphylactic reactions) are not so obvious to patients and doctors and require a careful history, physical and laboratory examination.
Patients should be advised to keep a diary of flushing reactions for two weeks, recording associations with food or medication intake, exercise or emotional stress, and symptoms including headache, bronchospasm, abdominal pain, diarrhea and urticaria, increased blood pressure or hypotension [ 7].
Most systemic disorders accompanied by hot flashes have typical accompanying symptoms. When the history and physical status and diary do not provide an obvious diagnosis, the patient should be recommended to evaluate for carcinoid syndrome, mastocytosis, and pheochromocytoma, as these are the most common systemic disorders causing hot flushes. Initial laboratory evaluation should include complete blood count and chemistry panel, 24-hour urine for 5-hydroxyindoleacetic acid (carcinoid syndrome), serum tryptase (systemic mastocytosis), and 24-hour urine for catecholamines and fractionated metanephrines (pheochromocytoma) (Table 4) [6].
Persistent erythema
Persistent facial erythema with rosacea is characterized by location in the central part of the face (nose, medial part of the cheeks, chin, central part of the forehead), unclear border and intensification when exposed to trigger factors (alcohol, temperature, etc.). Telangiectasia is characteristic, but not obligatory (Fig. 1).
This skin condition is most often differentiated from systemic lupus erythematosus, seborrheic dermatitis, dermatomyositis, etc. [8].
Systemic lupus erythematosus (SLE) manifests as erythema on the face in approximately half of cases and can start with skin manifestations without systemic pathology. Erythema in SLE is characterized by moderate swelling of the skin, red with a purple tint, localization on the cheeks and nose in the shape of a butterfly; insolation can be a provoking factor [8]. To confirm SLE, the ACR (1997) and SLICC (2012) diagnostic criteria are used, which, in addition to clinical symptoms, contain laboratory diagnostic indicators such as leukopenia (< 4.0 × 109/l at least once), lymphopenia (< 1. 0 × 109/L at least once), thrombocytopenia (< 100 × 109/L at least once), hemolytic anemia, immunological criteria (high levels of ANA, Anti-dsDNA Anti-Sm, antiphospholipid antibodies, low complement C3 and C4).
Dermatomyositis is a systemic disease of connective and muscle tissue, which manifests itself in muscle weakness of skeletal and smooth muscles of varying severity and characteristic symptoms on the skin, including the face. In some cases, skin rashes occur before muscle symptoms appear. Skin manifestations are characterized by Gottron's symptom - red nodules, plaques, spots on the skin in the area of the extensor surfaces of the joints (usually interphalangeal, metacarpophalangeal, elbow and knee) (Fig. 2); heliotrope rash - purple or red spots or papules on the upper eyelids and the space between the upper eyelid and eyebrow (purple glasses symptom), as well as papules and spots on the face (Fig. 3), chest and neck (V-shaped) (Fig. 4 ), upper back and upper arms (shawl symptom), abdomen, buttocks, thighs and legs. Often, changes in the skin of patients appear like tree branches (livedo arborescens) of a burgundy-bluish color in the area of the shoulder girdle and proximal limbs (Fig. 5) [8]. When diagnosing dermatomyositis, attention is paid to characteristic symptoms, namely increasing symmetrical weakness in the proximal muscles of the limbs in combination with increased creatine phosphokinase, typical skin lesions and systemic manifestations (fever, arthritis/arthralgia, increased ESR and C-reactive protein).
Rashes on the facial skin with seborrheic dermatitis are characterized by spots, red papules with peeling on the surface, the lesion most often affects folds (nasobuccal, retroauricular, etc.), the area of the eyebrows and beard in men (Fig. 6). In addition to rashes on the face, other areas rich in sebaceous glands are often affected - the scalp, sternum area, and interscapular area [8].
Conclusion
The differential diagnosis of transient and persistent erythema on the skin of the face is extensive and covers many benign and malignant diseases and conditions. Most of them, including rosacea, are benign. However, it must be remembered that erythema on the face can be a sign of severe life-threatening (malignant tumors, anaphylaxis, systemic mastocytosis, dermatomyositis, systemic lupus erythematosus), neurological, cardiovascular diseases, or be a consequence of treatment for concomitant pathologies.
CONFLICT OF INTEREST. The authors of the article have confirmed that there is no conflict of interest to disclose.
CONFLICT OF INTERESTS. Not declared.
Literature/References
- Berg M., Liden S. An epidemiological study of rosacea // Acta Derm Venereol. 1989; 69: 419-423.
- Wilkin J., Dahl M., Detmar M., et al. Standard classification of rosacea: report of the National Rosacea Society Expert Committee on the Classification and Staging of Rosacea // J Am Acad Dermatol. 2002; 46: 584-587.
- Wang YA, James WD Update on Rosacea Classification and Its Controversies // Cutis. 2019; 104: 70-73.
- Gallo RL, Granstein RD, Kang S, et al. Standard classification and pathophysiology of rosacea: The 2022 update by the National Rosacea Society Expert Committee // J Am Acad Dermatol. 2018; 78 (1): 148-155.
- Schaller M., Almeida L.M.C., Bewley A., Cribier B., et al. Recommendations for rosacea diagnosis, classification and management: update from the global ROSaceaCOnsensus 2022 panel // Br J Dermatol. 2020; 182, 1269-1276.
- Izikson L., English JC, Zirwas MJ The flushing patient: Differential diagnosis, workup, and treatment // J Am Acad Dermatol. 2006; 55 (2): 193-208.
- Sadeghian A., Rouhana H., Oswald-Stumpf B. Etiologies and management of cutaneous flushing // J Am AcadDermatol. 2017; 77: 391-402.
- Olazagasti J., Lynch R., Fazel N. The Great Mimickers of Rosacea // Cutis. 2014; 94: 39-45.
T. A. Sysoeva*, 1, Candidate of Medical Sciences I. E. Frolova** E. K. Murakhovskaya*, Candidate of Medical Sciences A. S. Bisharova*, Candidate of Medical Sciences I. B. Mertsalova*, Candidate of Medical Sciences
* Federal State Budgetary Educational Institution of Further Professional Education RMANPE of the Ministry of Health of Russia, Moscow, Russia ** Medical, Moscow, Russia
1Contact information
Rosacea: aspects of classification and diagnostic search for transient and persistent facial erythema / T. A. Sysoeva, I. E. Frolova, E. K. Murakhovskaya, A. S. Bisharova, I. B. Mertsalova For citation: Sysoeva T. A ., Frolova I. E., Murakhovskaya E. K., Bisharova A. S., Mertsalova I. B. Rosacea: aspects of classification and diagnostic search for transient and permanent erythema of the face // Attending Physician. 2021; 5 (24): 52-56. DOI: 10.51793/OS.2021.36.75.011 Tags: facial skin, redness, telangiectasia, transient erythema