Patients with different types of cuts require different types of sutures. Their purpose is to stop bleeding, close the wound, minimize the risk of infection, and reduce the scar.
The wound must be thoroughly cleaned before suturing begins. Interrupted stitches, or simple interrupted stitches, are used only for clean cuts. They close the wound very effectively. When a wound has ragged edges and contains dirt or foreign material, the edges of the wound should be carefully trimmed and all dirt removed before suturing. If there is significant damage to adjacent muscle tissue or other structures, absorbable sutures are used, which dissolve over time. The wounds can be closed either with a series of simple interrupted sutures or with a continuous suture under the top layer of skin. The last type of suture is also called a subcutaneous suture.
Subcutaneous suture
A subcutaneous suture using a continuous thread is often used by surgeons after surgery performed under sterile conditions. This is a quick way to close large wounds. In special situations, three other types of sutures can be used. Slit wounds are closed with either an upholstery suture or a vertical mattress suture. Tubular structures, such as the intestine, are closed with a "purse string" circular suture that can be pulled tight. Of the absorbable suture materials, the most commonly used is plain or chrome-plated catgut, produced from lamb or pig intestines. Silk, nylon, various polymers and wire are used as non-absorbable materials.
When to contact a healthcare professional:
Call your healthcare provider if you experience any of the following:
- temperature 100.4°F (38°C) or higher;
- chills (getting cold and shaking);
- any of the following symptoms in or around the wound: more redness or swelling, such as if the pink rim becomes wider than ¼ inch (6 mm);
- increasing pain or discomfort;
- skin that is hard, warm, or hot to the touch;
- bright yellow or green discharge;
- unpleasant odor;
- rash;
- blisters;
- drainage in an amount that saturates the bandage through and through;
- bleeding that does not stop after pressure has been applied to the wound area for 30 minutes;
to come back to the beginning
When a wound is left open
If more than six hours have passed since the skin injury before treatment began, or if the wound was caused by a blow or pressure, then in these cases it is better not to try to connect its edges in any way, but to actually leave the wound open. As a precaution, antibiotic treatment may be started to combat the infection. This does not replace cleaning the wound and removing foreign bodies and dead tissue. If the damage is not so severe that skin grafting is necessary, the wound will heal on its own, but it will take much longer than it would take after stitching. In addition, if the wound is not sutured, the risk of developing a rough scar and tightening of the skin is much higher.
Razor cuts can be quite deep and reach adjacent muscles. This entire area should be carefully inspected for any invisible damage. Then clean the wound thoroughly. Intermittent sutures are most suitable here, since the edges of the wounds are smooth.
Pain relief after the procedure
- You may experience pain or discomfort after the procedure. To relieve these symptoms, take acetaminophen (Tylenol®) or strong acetaminophen (Extra Strength Tylenol®).
- Do not take aspirin or nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen (Advil®) or naproxen (Aleve®). These medications make it harder for your blood to clot and may increase bleeding.
- Follow dosage directions on the package. If the recommended dosage does not relieve pain, call your doctor.
- If you are allergic to acetaminophen or have a medical condition that prevents you from taking it, ask your healthcare professional what medicine you can take instead.
- If you are participating in a clinical trial for cancer treatment, ask your oncologist (cancer treatment doctor) what pain medications you may take.
- You can also apply an ice pack to the wound to reduce pain, swelling, and bruising. Apply an ice pack to the wound for 15 to 20 minutes every hour or as directed by your healthcare professional.
to come back to the beginning
Closing the wound without suturing
The edges of the wound are joined to reduce bleeding, scarring and the risk of infection. However, they cannot always be sewn. If the wound is located in an area that is not affected by varying muscle tension and is not connected or is very superficial, then there are other ways to bring the edges of the wound together. These methods are especially useful when helping children, as they help avoid emotional and physical trauma.
- Closing a wound on the scalp by tying the hair growing on both sides is an effective way to treat superficial cuts.
- A non-damaging adhesive plaster (sterile strips) is often used. If you use it, the scar will be smaller.
- Special glue is an easy way to join the edges of small cuts. Apart from a slight burning sensation, it does not cause any pain. For children, this is less scary than stitches. After a few days, when the wound has healed, the glue is dissolved.
- Metal staples are used to hold wound edges together in most emergency departments, but not often.
Wound healing
A wound is a violation of tissue integrity due to mechanical stress (cuts, abrasions, bruises, bites). After damage, the body mobilizes forces to start the healing process. It can take different times depending on the characteristics of the wound and the ability of the tissue to regenerate. With infectious complications, the process may be delayed. You can stimulate the healing process of wounds and reduce the risk of infection with the help of special preparations, for example, cream for external use Argosulfan®.
Stages of wound healing
The wound healing process consists of several stages:
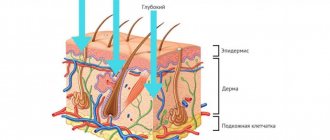
- Inflammation is a typical local reaction of the body to tissue damage and encounters with foreign substances. Blood flow to the wound site increases, leukocytes produce substances that trigger the inflammatory process necessary to cleanse the wound. As a result, its characteristic symptoms appear: redness and swelling. To control the situation, the adrenal glands begin to intensively produce corticosteroids and adrenaline, which have anti-inflammatory activity. This stage takes on average 4 days;
- Regeneration (direct healing) is the next stage, it usually lasts from the 4th to the 10th day. The body produces substances that stimulate cell division and metabolic processes in them, due to which young tissue (granulations) is formed at the site of damage, filling the wound;
- Scarring and epithelization are the final stage of wound healing, lasting from several weeks to several months. The wound is healed with young connective tissue, blood vessels and nerves grow inside it, blood circulation and innervation are restored, and a layer of epithelium is formed on the surface. There is always a trace of damage left on the skin, a scar or scar, the size and shape of which depends on the characteristics of the wound. The longer healing continues, the more connective tissue is formed in the wound, forming a scar.
The duration of each stage may vary, depending on the body's ability to regenerate and the characteristics of the wound itself.
Types of wound healing
There are three types of wound healing:
- Primary is possible only for wounds with smooth edges that are in close contact with each other. They should be free of germs, dirt, hemorrhages, and dead tissue. These are only postoperative wounds and those treated by a surgeon on the first day after their application. They heal with the formation of thin, barely noticeable scars;
- Secondary healing occurs if primary healing is not possible. Uneven or non-viable wound edges, gaping, and infection cause suppuration. Only after cleansing the wound and completing the purulent inflammation does it heal with the formation of a scar, sometimes rough;
- Healing under the scab is typical for superficial wounds. A scab is a crust formed from dried blood, lymph and intercellular fluid, released onto the surface of the wound when the skin is damaged. The scab protects the wound from infection and mechanical damage, and underneath it the wound heals quickly. There is no need to remove the crust unless there is suppuration underneath it - if events progress well, it will go away on its own.
Factors influencing the wound healing process
Reasons that slow down wound healing related to the condition of the whole organism:
- Age: the ability to regenerate tissue in older people is extremely low, so their wounds take longer to heal than in middle-aged patients and, even more so, in children;
- state of immunity: with congenital or acquired deficiency of the immune system, the body’s defenses are reduced, it takes more time to cope with foreign agents. The inflammatory stage is prolonged, infectious complications often develop, further increasing the duration of healing;
- Chronic diseases: with long-term illnesses, the body spends a lot of energy fighting them, so there are simply no resources left for healing wounds;
- Diabetes mellitus: glucose, which is too much in the blood during this disease, damages blood vessels, disrupting blood supply, tissue trophism and their ability to regenerate;
- Poor nutrition: If the body does not receive enough nutrients, wounds take longer to heal. First of all, this concerns proteins - they form substances involved in inflammation and new cells that restore tissue integrity.
Local causes affecting wound healing:
- Significant contamination of the wound and foreign bodies in it increase the duration of the inflammatory stage;
- Lack of primary wound treatment is the main cause of infectious complications;
- The location of the wound at the bend site, constant movements of its edges make regeneration and epithelization difficult
Basic rules for treating wounds
If the wound is properly treated immediately, the risk of infectious complications is significantly reduced, which means healing will take less time. It is important to remove dirt and foreign objects (splinters, rust, glass) from the wound surface, and then rinse it with antiseptic agents. After this, you can apply a bandage with an antibacterial agent.
Only superficial wounds can be treated on your own; in other cases, you need to consult a surgeon. To speed up wound healing, after treatment, local agents are used that stimulate cell division and prevent the development of infectious complications. An example of a drug that meets all these requirements is Argosulfan® cream for external use.
Argosulfan® for wound treatment
Argosulfan® cream is a local antibacterial drug with regenerating and antimicrobial properties. Its main component is silver sulfathiazole, which has a wide spectrum of antibacterial action against gram-positive and gram-negative bacteria. It dissolves slowly, due to which the concentration of active substances on the surface of the wound remains high for a long time.
Upon contact with skin, silver sulfathiazole breaks down into sulfathiazole and silver ions, both components fight microbes. Sulfathiazole prevents their growth and reproduction, and silver destroys them by destroying the shells. These substances stimulate tissue regeneration, wound healing, and reduce the risk of severe scar formation*.
Argosulfan® can be used to treat both dry, contracted and weeping purulent wounds. It can be applied openly or under a bandage: 2-3 times a day in a thick layer (2-3 mm). By keeping the surface of the wound moisturized, the cream makes dressings less painful. It is recommended to use the drug until the wound is completely healed, but not longer than 60 days.
Advertisement RUS-DRM-ARG-NON-08-2018-1265
* E.I. Tretkova, Complex treatment of long-term non-healing wounds of various etiologies, Clinical Dermatology and Venereology, 3 2013
Dressings for the treatment of non-healing wounds
When treating wounds of any nature, including chronic ones, the correct selection of dressing material plays an important role.
Dressing material for non-healing wounds should be:
•hygroscopic;
•"breathable";
•elastic and flexible – the bandage will have to be worn for a long time, so it should not interfere with movements.
Biotekfarm company offers a wide selection of dressings for the management of wounds of any complexity and at any stage. So, for wounds in which there are fragments of necrotic tissue or hemorrhage, a Parapran dressing with chymotrypsin is suitable - the drug included in the dressing helps to break down necrotic tissue, helping to cleanse the wound.
To moisturize “dry” chronic wounds (bedsores, trophic ulcers) and accelerate their healing, it is recommended to use the “GelePran” dressing with miramistin or colloidal silver. This soft transparent dressing, consisting of 70% water, moisturizes the surface of the wound, and the medicine it contains (miramistin or silver) disinfects and promotes regeneration.
For the treatment of infected wounds, bactericidal dressings Voskopran with Povidone-iodine ointment, antimicrobial dressings Voskopran with Dioxidin ointment, and anti-inflammatory dressings Voskopran with Levomekol ointment are suitable. Polipran dressings with Dioxidin are excellent for preventing infection of wounds at the granulation stage.
The Chitopran dressing based on chitosan nanofibers will help stimulate regeneration. It provides optimal conditions for healing - sufficient humidity, breathability and protection from damage, and promotes the rapid growth of its own cells. It is worth paying attention to the fact that this bandage does not need to be removed - it resorbs on its own as the wound heals.
Wound healing time and consequences
Healing a chronic wound is a long and complex process that can take from 1 to 3 months, depending on the depth and size of the wound. It should be borne in mind that epithelization of chronic wounds is very slow - no more than 1 cm per month. After complete epithelialization, the “new” skin increases its strength for another 6 months.
Recommendations for caring for the problem area are quite simple:
•protect the wound from compression and mechanical damage;
•change the bandage regularly (depending on the stage of healing and type of bandage);
•at the granulation stage - use dressings that accelerate healing.