Referring to many years of experience, I can say with confidence that augmentation mammoplasty is consistently among the most popular aesthetic surgeries - and for good reason. With its help, women not only improve their figure, but also get rid of complexes and gain self-confidence. However, in fairness, it is worth noting that any surgical intervention involves risks. In this material we will talk about one of the possible problems - implant rotation . Yes, this, unfortunately, happens, but, looking ahead, I will say that it does not pose a threat to health.
Reversing a round implant
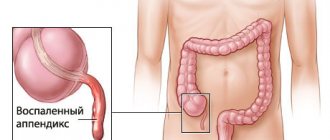
As you probably already know, round and anatomical implants . Both can turn around. In the first case, the change in position, as a rule, goes unnoticed, since there are no visual manifestations and the patient does not experience any discomfort. The only exception is the case when the product does not unfold, but turns over like a coin: with the back of the side, convex - towards the chest. As a result, the shape of the breast changes, asymmetry appears, but it is insignificant.
Reasons for crown mobility
In most cases, the mobility of the prosthesis has nothing to do with the qualifications of the implantologist. Among the main reasons are:
- Loosening of the screw connection between the abutment and the prosthesis
. This is possible if products from different brands were used. For example, the implant is Nobel Biocare, and the superstructure is Osstem. It is important to use original products of the same brand, which are developed as a whole, otherwise the likelihood of failure of all components is too high. - Loss of properties of the cement composition
. As a rule, this occurs due to high chewing load on the tooth, adherence to too hot or cold foods. The prosthetic system is fixed to the abutment with a soft cement composition; under unfavorable conditions, it begins to collapse, is gradually washed out, and the crown becomes loose.
The crown can be reattached in the clinic where the implantation was performed. The orthopedist will tighten the screw with an implantation key and secure the prosthesis. With the cement method of fastening, the crown will be cleaned of the remnants of the old composition and “set” on the cement again. Things are different if not only the crown, but the implant along with it is loose. It is very difficult to independently determine whether the implant crown is loose or the fixation of the intraosseous element is weakened. This requires a medical assessment of the clinical picture and a diagnostic examination.
Nature of the problem
I hasten to reassure you: reversing the implant does not pose a health hazard . This is purely an aesthetic problem. In other words, repeat surgery is not strictly necessary. The patient must simply decide for herself whether she is satisfied with such breasts, or whether she still wants to adjust the shape and make it ideal. By the way, a slight reversal often goes unnoticed; it is successfully disguised as the natural asymmetry that all women have before and after surgery.
What treatment methods are used
Treatment for mobility of the structure depends on the cause of the problem. If the implant crown is loose and the intraosseous element itself is motionless, it is again secured with a screw or cement. When the entire structure is wobbly, including the artificial root, treatment tactics are selected according to the clinical picture. The most favorable option is that the implant wobbles slightly, there is no inflammation around it, and the gums do not hurt.
In the second scenario, loosening of the artificial root occurs against the background of inflammation and pain in the jaw. Treatment includes:
- Cleaning the implant and nearby tissues - opening abscesses (if any), ultrasonic cleaning of plaque in the subgingival area.
- Osteoplasty using osteoplastic material and barrier membranes (according to indications).
- Antibacterial, antihistamine, anti-inflammatory agents.
- Treatment of the oral cavity with antiseptic compounds.
- X-ray control at each stage of treatment.
After the inflammation is eliminated, the prosthesis is again fixed to the implant. If the intraosseous element is rejected, it is removed from the socket, necrotic tissue is removed, and bone grafting is performed. Re-implantation is possible only after 6-8 months, when the bone mass has taken root and the tissue has recovered to its parameters.
How often does implant rotation occur?
Every representative of the fair sex wants the operation and rehabilitation period to go well, without complications and other unpleasant surprises. Therefore, during the consultation, patients are asked many questions, including the following: does implant rotation ? In my opinion, yes. We are, of course, not talking about tens of percent, but also not about isolated cases. The fact is that an implant is a foreign body. During the operation, the surgeon creates conditions for its 100% engraftment. However, each organism is unique, and the reaction is not always predictable.
Rejection symptoms
Rejection of the intraosseous element is a serious complication leading to the loss of the metal pin. Usually, implant rejection is accompanied by quite eloquent symptoms:
- Swelling of the gums, which does not decrease within 5 days after the intervention, but, on the contrary, increases.
- Reddened mucous membrane around the artificial root.
- Severe pain that intensifies with any load on the structure.
- Bleeding of the gums around the implant for more than 4-5 days after implantation.
- Purulent discharge from a wound.
- The appearance of a putrid odor from the implantation area.
- Excessive mobility of the artificial root, exposure of its neck, subsidence of the gums.
- Deterioration in general health, increase in temperature.
A loose implant crown is a reason to urgently go to the dentist. Rejection is rarely treated. With such symptoms, the best option is to remove the implant from the bone with further drug therapy aimed at restoring the body and regenerating bone tissue.
Reasons for implant reversal
Rotation of the implant can result from mechanical damage caused by a fall from a great height, in a car accident, etc. But such situations occur extremely rarely, and I sincerely wish you never get into them. As for the more real reason, this is the work of the pectoralis major muscle. With each contraction, it strives to smooth out the uneven contour beneath it. The influence of the pectoral muscle is especially great in the first months after surgery, then its tone decreases and reversal of the implant becomes unlikely.
Over time, the difference in breast shape with round and anatomical implants is practically erased. This means that the latter should be given preference only if there are indications, when the aesthetic effect they provide exceeds the risk of reversal.
Plastic surgeon Andrey Valentinovich Firsov says:
As in the old joke about the “lecture on love with slides,” today we will talk about revolutions and displacements. So, there are different types of revolutions, but in this article we will deal exclusively with the behavior of breast implants.
Let us immediately make a reservation that we will not consider the situation of the asymmetrical position of the implants due to their installation, since this is an error during the operation and nothing more.
Implant displacements can be very diverse.
Offset up
, as a rule, occurs under the action of the pectoral muscles with a fully axillary position and is accompanied by the appearance of a waterfall effect - the formation of the so-called double-bubble (photo 1, 2). This, I’m not afraid to say, vicious technique allows you to hide the implant more deeply in the tissues and in a calm state the breast looks quite decent, but when the muscles are tense, all the beauty comes to naught.
Photo 1: squeezing the implant up and double - bubble with fully axillary placement
Photo 2: waterfall effect when moving the implant upward
Or under the pressure of the implant capsule with capsular contracture (photo 3, 4):
Photo 3: bilateral capsular contracture with upward displacement of implants
Photo 4: implant displacement upwards and to the side with right-sided mammary fibrosis
Move to the sides or down
, below the natural submammary fold, usually occurs with a large implant volume. On average, the risk increases with a volume above 360-400 ml; and/or an artificially low submammary fold (photo 5, 6).
The submammary fold is perhaps the most stable and durable component, which should not be destroyed unnecessarily. And if this needs to be done, then it must be reshaped with seams. True, as with any rule, there are exceptions, and when installing implants with polyurethane foam coating, there is no need to additionally form and strengthen the fold.
Photo 5: displacement of the implant down to the right, below the inframammary fold
Photo 6: displacement of both implants downwards, below the inframammary fold
Lateral displacements are also observed
, all kinds of flips and rotations of implants, which is more relevant when placing anatomists (photo 7, 8):
Photos 7, 8: rotation of the anatomical implant on the right
There is a myth that round implants are not afraid of revolutions.
But it is not so. Indeed, rotation of such an implant does not lead to deformation, but there are also upside-down turns when the implant turns over like a pancake in a frying pan, and then the breast loses its shape (photo 9):
Photo 9: revolution, overturning of a round implant
The reasons leading to direct displacement, rotation or flip of implants can be divided into 3 main groups.
These are factors that must be taken into account when planning an operation; directly questions arising during the operation; and factors that influence in the postoperative period.
Factors that can lead to displacement or inversion of the implant include its shape. It's no secret that anatomical implants rotate more often. This occurs due to a displaced center of gravity, especially with high-profile implants with a truncated base.
Poor surface texture of implants contributes to poor tissue fixation and can lead to future inversion or displacement (photo 10). The most reliable in terms of fixation are polyurethane foam-coated implants, which are so intimately fixed in the tissues that the frequency of displacement tends to zero.
Photo 10 (from left to right): smooth implant without texture, textured, with polyurethane foam coating
It is also necessary to take into account the elasticity and turgor of tissues. In women with severe ptosis, multiple stretch marks, thin skin and a significant decrease in the volume of the mammary glands after breastfeeding or after weight loss, the risk of weak fixation and subsequent displacement of the implant is higher. Therefore, planning for tightening the “skin cover” must be adequate and fit as tightly as possible and stabilize the implant (photo 11, 12).
Photo 11: severe ptosis, multiple striae, decreased turgor and tissue elasticity
Photo 12: pronounced atrophic ptosis, reduced turgor and tissue elasticity
There are tricks during surgery aimed at stabilizing the position of the implant. For example, two-plane placement of implants, when the upper part of the implant is located under the gland and under the pectoralis major muscle, and the lower third is only under the gland (photo 13):
Photo 13: two-plane implant placement
This approach allows you to avoid “animation” of the breast when the muscles of the chest wall are tense (photo 14), and also allows you to best hide the upper pole of the implant in the tissues and, most importantly, stabilize the position of the implant by pressing it from above, receiving an additional degree of guarantee against its inversion .
Photo 14: axillary setting, animated distortions of the mammary glands with tension in the pectoral muscles
For some types of implants, the seat must be tight or, more correctly, exactly match the size and shape of the implant, so as not to give the implant the slightest chance of moving. This primarily applies to high-profile anatomical implants with a truncated base, filled with a highly cohesive gel.
When forming a larger bed than necessary, the percentage of displacements and revolutions increases, but if the bed is insufficient, situations may arise when the implant is under-stretched, somewhere the edge is bent or pressed in from one of the poles (photo 15), which, in turn, leads to aesthetic deformations. We can say that the golden mean is good here too.
Photo 15: insufficient bed, unformed lower pole
When replacing implants, the old capsule should be removed as much as possible, since the capsule is a smooth, glossy surface, and fixation of the implant in the old bed is very unreliable.
There are situations when two capsules are formed: one is directly adjacent to the implant, and the second remains in the tissues. Between these capsules there is always a small amount of serous fluid and a semblance of an articular surface is formed. The implant in such an improvised joint can rotate completely freely and, as patients say, “the breast changes shape several times a day.”
An additional factor that can lead to implant displacement in the future is the high traumatic nature of the operation and a large amount of wound fluid in the implant bed. Therefore, during repeated operations, in case of high bleeding during surgery, drains are necessarily used so that the tissues “embrace” the implant as quickly and tightly as possible.
But that's not all. The postoperative period and restrictions in the first 2-3 months after surgery are also important. In the early period, everyone is required to wear compression stabilizing garments for the period of primary fixation of implants, which takes 2-3 weeks (photo 16).
Photo 16: compression garments
During the same period, you cannot bend your torso without supporting underwear. The restriction of physical activity is longer, up to 2-3 months. This is the period of capsule formation, adaptation of the pectoralis major muscle and healing of wound surfaces. During this period, there is a high risk of traumatic ruptures of not yet healed tissue and possible displacement of the implant. In the future, there are no restrictions and the frequency of flips and displacements of implants decreases. But still, in the long term, implant overturns occur, which are often associated with excessive physical stress on the upper shoulder girdle.
Unfortunately, there is no 100% guarantee against a coup, but there are very few such cases with proper planning, the use of modern techniques and following the rules after surgery.
To communicate with patients who have undergone breast augmentation, lifting or reduction, come to our forum in the Mammoplasty
The implant fell out, what should I do?
In rare cases, the implant becomes unscrewed from the bone and may fall out. This occurs when the size of the socket and the intraosseous element do not match, as well as due to the weakness of the jaw bone. Such situations, when the implant loses its fixation and falls out, but there is no inflammation or other signs of rejection, can occur against the background of systemic diseases in which tissue regeneration is impaired (osteoporosis, diabetes mellitus). The problem is solved by reinstalling the structure using regenerative membranes (enriched with growth factors) that accelerate osseointegration, and prescribing a course of vitamin therapy.
Prevention
The best treatment is prevention. The positive outcome of the operation is influenced by:
- Professional approach
– you need to take the choice of a clinic and an implantologist seriously, since the success of treatment depends 90% on the professionalism of the doctor. - Quality of diagnosis and preparation
- you need to prepare seriously for the operation, eliminating all contraindications. To do this, you need to undergo tests and not hide health problems from the surgeon - the more the doctor knows about the patient’s health condition, the more accurately he will select the implantation protocol, and the better the implantation of the artificial root will be. - Oral hygiene
– at the preparation stage, all dental problems should be eliminated and the quality of hygiene procedures performed should be improved.
After implantation, be sure to follow medical recommendations regarding care, nutrition, and physical activity. Do not skip control and preventative examinations.
Signs of rejection and healing after implantation
The symptoms of implant rejection are similar to the symptoms that appear in the first weeks after installation of the structure, so you need to take into account the duration of their course. Minor pain in the area where the prosthesis was placed, swelling and redness of the gums, and ichor for 5-7 days are normal, as is an increase in body temperature up to 38 degrees. You should immediately consult a doctor in cases where:
- acute painful sensations do not go away within 1-2 weeks;
- swelling intensifies and spreads to other areas;
- the temperature persists for several days in a row and is difficult to control with antipyretic drugs;
- bleeding lasts longer than 2 days;
- the ichor is secreted for more than a week;
- pus discharge and an unpleasant odor appear;
- the structure has become mobile and falls out.
Sometimes implantation complications can occur without significant symptoms, but this is extremely rare. How do you know that the installation of implants was successful and the prosthesis has taken root? Complete implantation of the structure occurs within 2-5 months, depending on their type and method of implantation, but you can understand whether the operation was successful in 1-2 weeks, after the swelling and pain have passed. If the prosthesis has taken root, there should be no discomfort when pressing on it, mobility, discharge from the wound in the area of the sutures should completely stop, all unpleasant symptoms should go away.
How does an implant normally take root?
After installation of the implant, a period of osseointegration with the bone tissue of the jaw begins, which goes through three stages:
- Initial (3-4 weeks) Spongy bone tissue begins to form around the implanted implant. Until it is mature and has a low density, it is better to avoid chewing loads so as not to disturb the position of the implant in the jaw.
- Formation of mature bone (16-18 weeks) Spongy tissue is replaced by denser (lamellar) tissue. Completely fills the space between the implant and the jawbone. Provides stability sufficient to load the implant with a prosthetic structure.
- Final (up to one and a half years) The implant finally fuses with the bone tissue. After completion of this period, the success of implantation is determined. If the patient follows the rules of care and use, nothing should happen to the artificial root.
After engraftment, the implant becomes a full-fledged part of the dental system and can last a lifetime .