Wounds, burns, inflammation, infectious diseases, operations - all this can lead to the formation of scars. Normally, these scars lighten over time and become less noticeable. but sometimes the scar tissue grows, a rough convex formation of a bluish-burgundy color appears - a keloid scar.
The most modern way to combat this defect is laser removal of keloid scars. In our clinic “BL” this procedure is carried out using the most modern equipment.
Keloid scar: what is important to know
There are areas of the body that are more prone to the formation of keloids than others: the chest, neck, upper shoulders and the nasolabial triangle area. This type of scar differs from other scars in that it grows larger than the original damage to the skin and overlaps with healthy tissue. Keloid scars are divided into young (up to 5 years) and old (5-10 years). A young keloid is red, with a glossy surface, an old one is paler, its surface is usually uneven.
Removal of keloid scars is carried out only after a thorough differential diagnosis - the tactics here are fundamentally different than when working with ordinary scars.
Surgical removal of scars and scars –
It is much easier to prevent the appearance of keloid scars by using special ointments or silicone patches than to treat scars that have already appeared.
Surgical treatment consists of excision of the keloid scar using a scalpel or surgical laser. Surgical removal of scars with a laser should not be confused with the procedure of laser resurfacing of scars. The latter is a conservative non-surgical procedure. However, for keloid scars, surgical treatment methods are quite risky, because the operation may cause the formation of a similar or even larger keloid in the place of the previous one. Therefore, if excision is nevertheless used, then immediately after the operation all possible preventive measures are used to avoid relapse -
→ special ointments for scars, → corticosteroid drugs, → long-term wearing of a pressure bandage or compression garments after surgery.
Excision of a keloid using a surgical laser: video
Treatment
Laser resurfacing of keloid scars is the gold standard. The effects of the laser are targeted and precise - it allows you not to affect the surrounding healthy tissue. As a result of the effect, the volume of scar tissue is reduced, the tissue is softened, and the difference between the new tissue and the surrounding healthy skin is equalized.
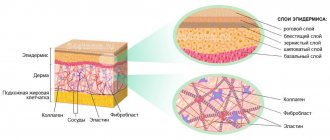
The effect of this procedure is cumulative - after treatment, the process of collagen and elastin production starts in the tissues, and continues for several months. As a result, new tissue with a healthy structure is formed.
Keloid and hypertrophic scar
Keloid and hypertrophic scar are: a benign growth of fibrous tissue that appears after trauma or wounding of the skin and represents a major therapeutic dilemma for the dermatologist due to frequent relapse; a proliferation of dense fibrous tissue that usually develops after damaged skin has healed. This tissue extends beyond the original wound, usually does not regress spontaneously, and tends to recur after excision.
The purpose of this study is to review the relevant literature and update information on keloids and hypertrophic scars that will help the clinician better understand and treat these lesions. The first description of keloids (recorded on papyrus) concerned surgical techniques used in Egypt in 1700. Subsequently, in 1806, Alibert used the term cheloide, derived from the Greek chele - crab claw, which referred to the lateral growth of tissue into unaffected skin.
Pathophysiology:
hypertrophic scars and keloids can be described as variations of normal wound healing. In a typical wound, 6-8 weeks after injury, a balance is established between anabolic and catabolic processes. At this stage, the strength of the wound is approximately 30-40% of the strength of healthy skin. As the scar develops, its tensile strength increases as a result of the progressive bonds of collagen fibers. At this point in time, the scar is usually hyperemic, but over the next months there is a tendency to change color - to natural, appearance - to softer and, thus, a regular mature scar is formed. When there is a mismatch between anabolic and catabolic processes, more collagen is produced than is degraded and the scar tends to grow in all directions. It is raised above the skin level and remains hyperemic. This excessive scar tissue is classified as a keloid or hypertrophic scar.
Kischer and Brody declared that the collagen knot is the structural unit of hypertrophic scar and keloid. This node, absent in mature scars, contains a high density of fibroblasts and unidirectional collagen fibers in a highly organized and varied orientation. In addition, keloid and hypertrophic scars differ from healthy skin in their rich vascular network, high density of mesenchymal cells and thickened epidermal layer. Attempts to separate keloid and hypertrophic scars in the early stages of their formation have proven difficult. Clinical differences become more significant as they develop. The most definitive histologic distinction is the presence of broad, pink collagen bundles in the keloid, which are not present in hypertrophic scars.
Keloid and hypertrophic scars, located in most areas, primarily cause a cosmetic problem. Some keloids or hypertrophic scars can cause contractures, which lead to loss of function if they cross a joint or disfigurement if located on the face. And keloids or hypertrophic scars can be painful or itchy.
Keloid or hypertrophic scars can be genetically related to leukocyte antigens: B14, B21, Bw16, Bw35, DR5, DQw3, and the second blood group. Transmission is possible both by an autosomal dominant and an autosomal recessive type.
Epidemiology:
keloid is often found among darkly pigmented races. The incidence of keloid is reported to be predominant in black and Hispanic populations and in a random sample of black Africans. The incidence of hypertrophic scar is possibly higher than that of keloid, but reliable information is lacking. Keloid can appear at any age, but develops more readily during and after puberty. Young individuals are more likely to be injured, and young skin creates more tension, while older skin is less elastic and more rigid. The level of collagen synthesis is also higher in young patients. Cosman et al found the mean age of onset of treated patients to be 25.8 (22.3 in women and 22.6 in men).
Race:
In Polynesians and Chinese, keloids form more frequently than in Indians and Malaysians. 16% of black Africans, in a random sample, suffer from keloids. In whites and albinos, keloid is much less common.
Floor:
The incidence of keloid in young women is higher than in young men, possibly due to the higher incidence of ear piercing among women. In other age groups, keloid affects both genders equally.
Age:
Keloid scars are most common in individuals aged 10-30 years. Keloid scars are less common in extreme age groups, although the increasing number of presternal keloid scars in older age groups is associated with an increase in the number of coronary artery bypass grafting operations.
Clinical part Keloid and hypertrophic scar present a major therapeutic dilemma for the dermatologist due to frequent relapses. A better understanding of the pathogenesis of keloids may lead to improved treatment by reducing its growth and eliminating regrowth. Although the optimal treatment for keloid has not been determined, successful treatment can be achieved through a multi-model approach. Regardless of the technique used, to exclude relapse, the observation period should be at least 2 years. Keloid and hypertrophic scar are abnormal wound reactions in susceptible individuals. (Fibrotic growth of connective tissue in response to injury, inflammation, surgery, or burn) Both a keloid and a hypertrophic scar are characterized by the accumulation of collagen and glycoprotein deposits. Separating a keloid from a hypertrophic scar can be difficult. Clinically, a keloid differs from a hypertrophic scar in that it extends beyond the wound and rarely regresses, whereas a hypertrophic scar remains within the wound and often regresses spontaneously. This fibrous growth often causes serious cosmetic and symptomatic problems. There are many treatment routes, and the reported effects also vary.
Story:
Keloid and hypertrophic scars are usually asymptomatic, but they may be firm, painful, itchy, or have a burning sensation. In addition to symptomatology, cosmetic concerns are the main reasons why patients seek medical attention.
Inspection:
Source of Damage A keloid is an overgrowth of scar tissue, usually in the area of a previous injury. The keloid extends beyond the damaged area and rises above the skin level, but rarely penetrates into the subcutaneous tissue. Hypertrophic scars remain confined to the injured area and spontaneously regress within 12-18 months, although regression may not necessarily be complete.
Keloid Clinic
Keloid ranges from soft and pale to red and hard. Keloids range from soft and pliable to hard rubbery. Recent research has demonstrated how to differentiate and classify keloids according to how they feel to the touch. Early lesions are often erythomatous. With age, the lesions become brownish-red and then fade. The lesions are usually devoid of hair follicles and other functioning adnexal glands.
The clinical course of keloid can vary. Most lesions continue to grow over weeks and months, others grow for years. Growth is usually slow, but sometimes keloids grow rapidly, tripling their size within a few months. Once the keloids stop growing, they usually become asymptomatic, unchanged, or slightly involute. Keloids on the ears, neck and stomach tend to be pedunculated. Keloids in the center of the chest and limbs usually protrude from the surface and its base is often wider than the top. Most keloids are round, oval, or oblong with regular edges, however, some have a clawlike configuration with irregular edges.
Most patients have one or two keloids, however, some patients, especially patients with spontaneous keloids, have multiple lesions, as do patients who develop keloids due to acne or chickenpox.
Frequency of damage areas
In white people, keloids tend to be present, in decreasing order of frequency, on the face (cheek and pinna), upper extremities, chest, presternal region, neck, back, lower extremities, breast, abdomen.
In blacks, in decreasing order of frequency, it tends to be present on the auricle, face, neck, lower extremities, mammary glands, back, abdomen.
In Asians, in decreasing order of frequency - auricle, upper limbs, neck, mammary gland, chest.
Etiology:
Factors that play a large role in the development of keloid are genetic predisposition combined with some forms of skin trauma. Various types of skin damage that can lead to keloid growth include: surgery, ear piercings, tears, abrasions, tattooing, vaccinations, injections, insect bites, burns and any processes that cause inflammation of the skin (smallpox, acne, folliculitis and H.Zoster) .
Skin or wound tension is also a critical factor for the development of keloids and hypertrophic scars. Tension can come from a variety of sources. Tissue deficiency (eg, following trauma, avulsion, or surgical excision) increases tension when wound closure is attempted. Also, constant tension is transmitted to the wound from the underlying bone and cartilaginous skeleton. Planned excision should be performed in such a way that the underlying muscles cause as little tension as possible on the wound. Keloid formation is associated with endocrine factors. Keloid formation is higher in those areas where the concentration of melanocytes is higher and less common on the palms and soles, where the concentration of melanocytes is minimal. Keloid often appears during puberty and goes away during menopause. Patients note the onset or enlargement of keloid during pregnancy.
No specific gene or set of genes has been identified as being responsible for keloid development, but the association of keloid incidence with skin pigmentation suggests a genetic basis or genetic link. Skin trauma, both physiological (ear piercings, surgery) and pathological (acne, smallpox) has been identified as the primary cause for the development of keloids.
Laboratory tests Diagnosis is usually based on clinical examination. A biopsy helps confirm the diagnosis in uncertain cases.
Histology:
When using a light microscope, the histopathological separation of a keloid and a hypertrophic scar may be difficult, but using a scanning electron microscope, a clear morphological separation between normal skin, keloid and hypertrophic scar can be made. Normal skin contains various collagen bundles, most of which are parallel to the epithelial surface. Collagen bundles are unsystematically connected to other collagen bundles through thin fibrillar trabeculae. In a hypertrophic scar, the collagen bundles (flatter) are less emphasized and the fibers are grouped in a wavy pattern, however, most bundles are still parallel to the epithelial surface. The ultrastructure of the keloid is represented by the same collagen bundles, but virtually nonexistent, and fibrillar strands are haphazardly connected, lose sheets and are randomly oriented to the epithelial surface. Ehrlich reports several morphological and immunological differences between a hypertrophic scar and a keloid. A keloid contains large, thick collagen fibers assembled from several fibrils packed together, in contrast to a hypertrophic scar, which contains thin, randomly organized collagen fibers, small vessels and fibroblasts. Only hypertrophic scars contain alpha-smooth muscle myofibloblasts, which secrete actin, which is an important element in the pathogenesis of contraction.
Immunology.
Some studies support the hypothesis that an immunological mechanism plays an important role in hypertrophic scar formation. Castagnoli et al. found genetically determined risk factors for hypertrophic scar formation localized in the HLA region. HLA-DRB-16, B-14, and BW-16 are related to keloid predisposition. Studies also show that IgG, IgA, and IgM have more deposits in keloid tissue. Autoimmune fibroblast antibodies were extracted from keloid tissue. These Antibodies have a stimulating effect on fibroblasts in the pathogenesis of keloid.
It is possible that intrinsic fibroblastic abnormalities associated with the immunological response may cause keloids. Experimental studies have shown that keloid fibroblasts clearly demonstrate an autonomous ability to synthesize large amounts of collagen, providing insight into the treatment of hypertrophic scar and keloid. There are 3 phases of normal skin healing: inflammation, fibroplastic phase and maturation. In the inflammatory phase, the capillaries expand and allow fluid to pass into the damaged area, fibrin clots isolate the wound. The released biochemical substances cause vasodilation and pain. Inflammatory cells are mobilized and move towards the damaged area. During this 1st phase, the epithelium grows rapidly through the sealed wound. In the fibroplastic phase, fibroblasts move towards the fibrin clot and begin to synthesize more new collagen. In this phase, wound tension increases rapidly. In the maturation phase, the nodularity and redness of the wound decrease, the scar becomes softer and more flattened. From a biochemical point of view, the processes of collagen synthesis and its degradation are combined. The tension of the wound gradually increases, and the end of the restructuring is the formation of a scar within 12 months from the moment of injury. Early forms of fibroblasts survive longer in a keloid than in a normal skin scar. In normal wound healing, connective tissue elements regress after the 3rd week, while in a keloid fibroblasts proliferate around the small vessels that have formed, creating dense masses of collagen. This process can continue for months to years, which determines the size of the keloid. Fibroblast proliferative activity was found to be significantly higher in keloids than in hypertrophic scars or normal skin. Oliver and colleagues and Babu and colleagues indicate that fibroblasts isolated from keloids are characterized by 4 times greater activity in the synthesis of fibronectin compared with fibroblasts from normal dermis and normal scar Fibronectin plays an important role in wound healing, promoting clot formation and the development of granulation tissue and reepithelialization.
The predominant types of collagen (Type I and III) are found in keloid, but small amounts of Types (IV and V) are also present. In normal adult skin, there are bundles of type 1 collagen, but 20 times less type 3 collagen.
Collagen synthesis in a keloid is 20 times higher than in normal undamaged skin and 3 times higher than in a hypertrophic scar. Type I and III collagen levels were significantly increased in keloid compared to other groups. Friedman and colleagues report two different mechanisms, one pretranscriptional and the other posttranscriptional, regulating the synthesis of type I collagen. He states that in keloid, neither mechanism functions efficiently to down-regulate type I collagen. Growth factors are now known to play a role in scar reduction. Transforming growth factor (TGF) and platelet-derived factor (PDGF) have been found to play a key role in the development of contraction in normal dermal fibroblasts. TGF clearly ensures the chemotaxis of fibroblasts in the area of inflammation and determines the onset of production of extracellular matrix proteins. TGF activity ceases when healing is complete. Dysregulation of TGF production or activity can lead to abnormal fibrosis. Younai et al showed that hypertrophic scar fibroblasts, compared with normal fibroblasts, have a highly elevated level of TGF secretion. Antibodies to TGF reduce matrix contraction by reducing fibroblasts and collagen synthesis. Tan et al found that fibroblast growth factor inhibits collagen production in keloids by decreasing gene expression, resulting in decreased transcription of the corresponding RNA.
Kischer et al report that most capillaries in hypertrophic scars and keloids are closed or partially closed in the presence of excess endothelial cells. Microvascular occlusion supports the theory that hypoxia is an important factor in the generation of hypertrophic scar. The formation of collagen in the inflammatory stage in keloids and hypertrophic scars takes significantly longer than in normal wound healing. Collagen fibers in granulation tissue are arranged in a whorled pattern. These nodes grow and are ultimately represented by thick, compact (dense), hyalinized bundles of collagen of a concentric structure. In a keloid, the collagen condensations are vaguely expressed, while in a hypertrophic scar, thick hyalinized collagen bundles gradually thin and are arranged so as to be parallel to the free surface of the skin.
Keloido therapy
It is important to understand the clinical differences between a hypertrophic scar and a keloid, which can help guide treatment. The clinical manifestations of keloid are extremely varied and reflect variations in the underlying injury.
A keloid may be present immediately after an injury, but may take months to develop. However, keloids have been known to appear spontaneously (especially in the sternum area). Traditional treatments that may be effective include a combination of surgery with steroid injection into the affected area or radiotherapy, silicone patches, pressure, cryotherapy. Some newer models presented as effective include pulsed dye laser, interferon alfa-2b, and cultured epithelial autograft. There is no single therapeutic model that is best for all keloids. The location, depth of the lesion, size, age of the patient, and response to treatment determine the type of therapy used.
The first rule when treating keloid is its prevention. Avoidance of unnecessary cosmetic surgery in patients predisposed to keloid formation, except in patients in whom the keloid is found or known only on the pinna. Closure of all surgical wounds with minimal tension. Incisions should not go through the surface of the joints. Avoiding mid chest incisions and creating incisions along skin folds whenever possible.
Treatment
Treatment of hypertrophic scars and keloids includes the use of occlusive dressings, compression therapy, intralesional corticosteroids, cryosurgery, excision, radiation therapy, laser therapy, interferon treatment, imiquimod 5% cream and other promising but lesser-known methods aimed at the synthesis process collagen.
Previous news
"Ellada" offers Kirov residents unique services
Next news
How to quickly heal joints?
How does the procedure work?
We treat keloid scars using the Dermablate MCL 30 erbium laser from the German brand Asclepion. Of all existing hardware techniques, this is the one that guarantees the best result. In addition, it is completely safe.
The area to be treated is cleaned, an antiseptic and anesthetic gel are applied. The doctor then directs the laser beam at the scar. Discomfort is minimal - to reduce discomfort, a cooling system is used (during the procedure, cold air is supplied to the treatment area). At the final stage, special medicinal compounds are applied to the skin. The doctor then makes recommendations for home care.
During the rehabilitation period, the skin should not be rubbed or damaged, and overheating (baths, saunas, long exposure to the sun) should also be avoided. In some cases, the use of hormonal ointments in courses is required. Also, sometimes injections of hormonal drugs are carried out directly into the problem area even before laser treatment. To reduce the likelihood of relapse and prevent the growth of scar tissue, the doctor may apply a special pressure bandage.
Laser benefits
The main advantage is the possibility of local impact only on scar tissue. Healthy skin is not damaged, and this makes it possible to shorten the rehabilitation period. Secondly, a significant advantage is high efficiency - even the most pronounced defects after the procedure are leveled out and become less noticeable. Finally, safety - unlike surgical excision and exposure to chemical acids, laser does not involve blood or deep damage.
To make an appointment for keloid scar removal in Moscow , call us or fill out the form on our website. Clinic “BL” is located within walking distance from the Oktyabrskoye Pole metro station, at the address: st. Marshala Rybalko, house 2, building 6.