According to established social moral traditions, a girl should lose her virginity in the arms of her beloved guy. This is an ideal option for starting sexual activity, but real life is somewhat more prosaic, and therefore sometimes circumstances are such that a girl has to say goodbye to her innocence in the gynecologist’s office through a simple procedure called “surgical defloration.”
Why and who needs surgical defloration
There are five reasons why a girl may decide to lose her virginity surgically rather than naturally:
- Pathologies of the hymen. Some women are born with an overly thick or overly elastic hymen. The integrity of such a hymen is very difficult to break during normal sexual intercourse, and of course it is absolutely impossible to do this painlessly. It is important to clarify that the hymen cannot “harden” with age, as is stated in some “folk” myths.
- Atresia of the hymen. Another rare pathology in which the hymen is completely overgrown, including the channels for the outflow of vaginal secretions or menstrual flow. Most often, atresia occurs against the background of inflammatory diseases of the vagina after childbirth or gynecological operations, but sometimes the overgrowth of the hymen is congenital. This problem can only be eliminated through surgery.
- Hemophilia. A rare congenital disease in which the coagulation process (blood clotting) is disrupted. For girls with this problem, natural defloration is deadly due to the risk of high blood loss. It should be noted that in severe forms of hemophilia, surgical defloration is also contraindicated.
- Phobias. Psychological fears (phobias) are a common reason for a girl’s desire to lose her virginity surgically, without having sexual intercourse with a man. The main phobias of this kind include primaisodophobia (fear of sexual activity), hematophobia (fear of the sight of blood) and algophobia (fear of pain in any form).
- The desire to hide inexperience. Sometimes the desire to undergo surgical defloration is dictated by the desire to conceal the fact of virginity. This happens when a girl has avoided sexual contact for a long time or has not had the opportunity to begin sexual activity (for example, due to illness), and is now embarrassed by her “inexperience.”
About contraindications
Surgical defloration cannot be performed during the menstrual period, or in the presence of the following pathologies:
- oncological or inflammatory diseases of the pelvic organs;
- infectious and colds in the acute phase;
- acute cardiac, hepatic or renal failure.
How to understand if everything is okay
So, nothing works because of the pain. There are several options before you: go to a doctor or figure it out on your own; the second option is much simpler. Take a mirror, spread the labia minora apart and just look.
If there is no hole in the hymen, then this is an obvious pathology, but it is usually detected before the onset of menstruation, because then the menstrual blood will have nowhere to go and pain will occur.
A more common situation is presented below, when there is a small hole, it is quite enough for menstrual function, but breaking during sex is extremely difficult. Sometimes there is a kind of septum in the hymen, which does not rupture, but only stretches, causing acute pain every time you try to initiate sexual activity. This type of structure is quite rare compared to others, on average in 1 in 2000 women.
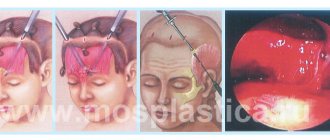
General procedure for the operation
Removing the hymen is a simple operation and takes no more than 10-15 minutes. Having placed the girl on the gynecological chair, the doctor gives her local anesthesia (less commonly, full anesthesia is used), after which he excises the hymen partially or completely. Then the edges of the wound are coagulated and treated with antiseptic agents.
Usually, after surgical defloration, patients are advised to rest for 1-2 hours in the hospital, and then avoid sexual intercourse for seven days, but if the operation was performed with the Surgitron device, then a recovery period is not required.
There is no need to be patient. Consult a doctor
In such situations, they resort to a safe, painless and simple operation - surgical defloration.
The reason for this may also be the congenital structural features of the hymen; its tissue can be very strong; doctors call this condition a dense hymen. In this case, the natural path through pain may end in severe bleeding. At an age not very typical for the onset of sexual activity, the hymen undergoes degenerative changes and also loses its qualities. In this situation, the sexual partner may also not be able to cope; it is especially difficult, for example, at the age of 30 to explain one’s innocence. What is an advantage at 18 is often seen as a disadvantage later in life.
The easiest and most painless way to get rid of the problem is to undergo surgical defloration.
Contraindications to surgical defloration
- Poor blood clotting;
- The presence of inflammatory processes in the body;
- The presence of infections in the body;
- Exacerbation of chronic diseases;
- Acute diseases of internal organs;
- Heat;
- Oncology;
- Menstruation;
- Venereal diseases;
- HIV;
- Mental disorders.
Author: Demin Sergey Anatolyevich Plastic surgeon, Candidate of Medical Sciences Author of more than 20 scientific papers on aesthetic and general surgery. Winner of the Crystal Lotus Award in the nominations “Best Plastic Surgeon for Abdominoplasty” and “Best Plastic Surgeon for Lipolifting”.
Intimate plastic surgery
Anesthesiology and resuscitation
| Service code | Internal code | Name | Price, rub |
| B01.003.004.007 | 37.1.1 | Spinal anesthesia lasting up to 1 hour | 8 000 |
| B01.003.004.006 | 37.1.2 | Epidural anesthesia lasting up to 1 hour | 14 000 |
| B01.003.004.008 | 37.1.3 | Spinoepidural anesthesia lasting up to 1 hour | 20 000 |
| B01.003.004.009 | 37.1.4 | Total intravenous anesthesia up to 20 minutes | 6 000 |
| B01.003.004.009 | 37.1.5 | Total intravenous anesthesia from 20 minutes to 60 minutes | 12 000 |
| B01.003.004.010 | 37.1.6 | Endotracheal anesthesia from 1 hour to 2 hours | 20 000 |
| B01.003.004.010 | 37.1.7 | Endotracheal anesthesia from 2 hours to 3 hours | 26 000 |
| B01.003.004.010 | 37.1.8 | Endotracheal anesthesia from 3 hours to 4 hours | 34 000 |
| B01.003.004.010 | 37.1.9 | Endotracheal anesthesia from 5 to 6 hours | 58 000 |
| B03.016.011 | 37.1.10 | Express analysis of blood gases and electrolytes | 2 000 |
| B03.016.011 | 37.1.11 | Advanced express analysis of blood gases and electrolytes | 2 500 |
| B03.016.011 | 37.1.12 | Artificial ventilation for 12 hours | 7 200 |
| B01.003.004.010 | 37.1.13 | Endotracheal anesthesia up to 1 hour | 14 000 |
| B01.003.004.010 | 37.1.14 | Endotracheal anesthesia from 4 to 5 hours | 40 000 |
| B01.003.004.002 | 37.1.15 | Conduction anesthesia of the 1st category of complexity | 4 000 |
| B01.003.004.005 | 37.1.16 | Infiltration anesthesia (large volume or area) up to 30 minutes | 3 000 |
| B01.003.004.005 | 37.1.17 | Infiltration anesthesia up to 15 minutes | 1 400 |
| B01.003.004.004 | 37.1.18 | Application anesthesia | 1 000 |
| B01.003.004.009 | 37.1.19 | Drug sedation with hemodynamic monitoring | 3 000 |
| B01.003.004 | 37.1.20 | Prolonged regional anesthesia (days) | 8 000 |
| A11.12.001 | 37.1.21 | central vein catheterization | 10 000 |
| A11.23.002 | 37.1.22 | TAP TEST | 12 500 |
| A11.23.001 | 37.1.23 | Diagnostic spinal (lumbar) puncture | 3 500 |
| B01.003.004.007 | 37.1.1.2 | Spinal anesthesia from 1 hour to 2 hours | 14 000 |
| B01.003.004.007 | 37.1.1.3 | Spinal anesthesia from 2 hours to 3 hours | 17 000 |
| B01.003.004.007 | 37.1.1.4 | Spinal anesthesia from 3 hours to 4 hours | 20 000 |
| A11.23.003.001 | 37.1.2.1 | Placement of an epidural catheter | 8 000 |
| B01.003.004.006 | 37.1.2.2 | Epidural anesthesia from 1 hour to 2 hours | 17 000 |
| B01.003.004.006 | 37.1.2.3 | Epidural anesthesia from 2 hours to 3 hours | 21 000 |
| B01.003.004.006 | 37.1.2.4 | Epidural anesthesia from 3 hours to 4 hours | 24 000 |
| B01.003.004.006 | 37.1.2.5 | Epidural anesthesia from 4 hours to 5 hours | 28 000 |
| B01.003.004.008 | 37.1.3.1 | Spinoepidural anesthesia from 1 hour to 2 hours | 22 000 |
| B01.003.004.008 | 37.1.3.2 | Spinoepidural anesthesia from 2 hours to 3 hours | 26 000 |
| B01.003.004.008 | 37.1.3.3 | Spinoepidural anesthesia from 3 hours to 4 hours | 27 000 |
| B01.003.004.008 | 37.1.3.4 | Spinoepidural anesthesia from 4 hours to 5 hours | 30 000 |
| B01.003.004.009 | 37.1.5.1 | Total intravenous anesthesia from 1 hour to 2 hours | 20 000 |
| B01.003.004.009 | 37.1.5.2 | Total intravenous anesthesia from 2 hours to 3 hours | 24 000 |
| B01.003.004.010 | 37.1.9.1 | Endotracheal anesthesia from 6 to 7 hours | 65 000 |
| B01.003.004.010 | 37.1.9.2 | Endotracheal anesthesia from 7 to 8 hours | 70 000 |
| B01.003.004.002 | 37.1.15.1 | Conduction anesthesia of the 2nd category of complexity | 5 000 |
| B01.003.004.002 | 37.1.15.2 | Conduction anesthesia of the 3rd category of complexity | 6 000 |
Intimate surgery
| Service code | Internal code | Name | Price, rub |
| A16.21.019 | 37.26.1 | Penis lengthening (1 cat) | 80 000 |
| A16.21.019 | 37.26.2 | Penis lengthening (2 cat.) | 120 000 |
| A16.21.019 | 37.26.3 | Penis lengthening (category 3) | 160 000 |
| A16.21.019 | 37.26.4 | Thickening of the penis (1 category) | 100 000 |
| A16.21.019 | 37.26.5 | Thickening of the penis (category 2) | 150 000 |
| A16.21.019 | 37.26.6 | Thickening of the penis (category 3) | 250 000 |
| A16.21.019.003 | 37.26.7 | Thickening/lengthening of the penis with microsurgical flap transplantation (4 categories) | 350 000 |
| A16.21.019 | 37.26.8 | Augmentation penile endoprosthetics (1 category) | 120 000 |
| A16.21.019 | 37.26.9 | Augmentation penile endoprosthetics (2 categories) | 190 000 |
| A16.21.019 | 37.26.10 | Augmentation penile endoprosthesis (category 3) | 290 000 |
| A16.21.019.001 | 37.26.11 | Penile endoprosthetics (1 category) | 100 000 |
| A16.21.019.001 | 37.26.12 | Penile endoprosthetics (2nd category) | 150 000 |
| A16.21.019.001 | 37.26.13 | Penile endoprosthetics (category 3) | 200 000 |
| A16.21.019.001 | 37.26.14 | Penile endoprosthetics (4th category) | 250 000 |
| A16.21.036 | 37.26.15 | Testicular replacement | 35 000 |
| A16.21.036 | 37.26.16 | Bilateral testicular replacement | 60 000 |
| A16.20.098 | 37.26.17 | Plastic surgery of the labia minora (1 category) | 25 000 |
| A16.20.098 | 37.26.18 | Plastic surgery of the labia minora (2 categories) | 35 000 |
| A16.20.098 | 37.26.19 | Plastic surgery of the labia minora (3 categories) | 40 000 |
| A16.20.028.004 | 37.26.20 | Reduction of vaginal volume (1 category) | 45 000 |
| A16.20.028.004 | 37.26.21 | Reduction of vaginal volume (2nd category) | 60 000 |
| A16.20.028.004 | 37.26.22 | Reduction of vaginal volume (category 3) | 80 000 |
| A16.20.029 | 37.26.23 | Aesthetic clitoroplasty (1 category) | 35 000 |
| A16.20.029 | 37.26.24 | Aesthetic clitoroplasty (2 categories) | 50 000 |
| A16.21.036 | 37.26.25 | Microsurgical ligation of the veins of the spermatic cord (1 category) | 50 000 |
| A16.21.036 | 37.26.26 | Microsurgical ligation of the veins of the spermatic cord (2 classes) | 75 000 |
| A16.21.036 | 37.26.27 | Microsurgical reconstruction of the vas deferens (1 category) | 120 000 |
| A16.21.036 | 37.26.28 | Microsurgical reconstruction of the vas deferens (category 2) | 150 000 |
| A16.21.036 | 37.26.29 | Microsurgical reconstruction of the vas deferens (category 3) | 200 000 |
| A16.21.019 | 37.26.30 | Reconstruction of the penis using microsurgical techniques (phalloplasty, stage 1) | 150 000 |
| A16.21.019 | 37.26.31 | Reconstruction of the penis using microsurgical techniques (phalloplasty, stage 2) | 250 000 |
| A16.21.019 | 37.26.32 | Reconstruction of the penis using microsurgical techniques (phalloplasty, category 3) | 350 000 |
| A16.28.032.002 | 37.26.33 | Stem urethroplasty using microsurgical technique (1 category) | 170 000 |
| A16.28.032.002 | 37.26.34 | Stem urethroplasty using microsurgical technology (2 categories) | 270 000 |
| A16.28.032.002 | 37.26.35 | Stem urethroplasty using microsurgical technology (category 3) | 370 000 |
| A16.28.032.002 | 37.26.36 | Urethroplasty using local tissues (1 cat) | 50 000 |
| A16.28.032.002 | 37.26.37 | Urethroplasty using local tissues (2 cat) | 80 000 |
| A16.28.032.002 | 37.26.38 | Urethroplasty using local tissues (category 3) | 120 000 |
| A16.28.032.002 | 37.26.39 | Anastomotic urethroplasty (1 category) | 120 000 |
| A16.28.032.002 | 37.26.40 | Anastomotic urethroplasty (2 categories) | 150 000 |
| A11.02.002 | 37.26.41 | Botulinum therapy in urology (anesthesia, drug administration) | 28 000 |
| 37.26.42 | Botox (medical use in addition to a service that includes at least 100 units of the drug) 1 unit | 213 | |
| A16.20.068.01 | 37.26.43 | Reduction of the labia majora, category 1 | 40 000 |
| A16.20.068.02 | 37.26.44 | Reduction of the labia majora, category 2 | 55 000 |
| A16.20.068.03 | 37.26.45 | Reduction of the labia majora, category 3 | 70 000 |
| A16.20.068.04 | 37.26.19.1 | Plastic surgery of the labia minora (4 categories) | 55 000 |
| A16.20.068.05 | 37.26.19.2 | Plastic surgery of the labia minora (category 5) | 70 000 |
| Intimate surgery* | |||
| A16.30.066 | 37.30.19 | Removal of endoprosthesis of the penis and scrotum 1st stage | 30 000 |
| A16.30.066 | 37.30.20 | Removal of endoprosthesis of the penis and scrotum 2nd stage | 40 000 |
| A16.30.066 | 37.30.21 | Removal of endoprosthesis of the penis and scrotum 3rd class | 60 000 |
| A16.20.059 | 37.30.22 | Removal of a foreign body from the genital organs, stage 1 | 20 000 |
| A16.20.059 | 37.30.23 | Removal of a foreign body from the genital organs, category 2 | 40 000 |
| A16.20.059 | 37.30.24 | Removal of a foreign body from the genital organs, category 3 | 80 000 |
| Intimate surgery, Reconstructive urology* | |||
| A16.30.030.1 | 37.30.26 | Prefabrication of autograft – I category of complexity | 35 000 |
| A16.30.030.1 | 37.30.27 | Prefabrication of autograft – II category of complexity | 45 000 |
| A16.30.030.1 | 37.30.28 | Prefabrication of autograft – III category of complexity | 60 000 |
General hospital services
| Service code | Internal code | Name | Price, rub |
| S01.001.001 | 37.0.1 | Stay in a hospital ward (daily) | 6 000 |
| S01.001.002 | 37.0.2 | Stay in a hospital ward (daytime until 21:00) | 3 000 |
| S01.001.003 | 37.0.3 | Stay in the ward for accompanying persons (daily) | 6 000 |
| S01.001.004 | 37.0.4 | Stay in hospital room VIP 1 (daily) | 10 000 |
| S01.001.005 | 37.0.5 | Stay in hospital room VIP 2 (daily) | 16 000 |
| S01.001.006 | 37.0.6 | Stay in a hospital ward (daily, without meals) | 3 400 |
| S01.001.007 | 37.0.7 | Stay in the intensive care unit from 6-24 hours | 8 000 |
| B01.047.009 | 37.0.9 | Supervision by a therapeutic physician (1 visit) | 2 500 |
| A11.12.003 | 37.0.10 | Infusion therapy of expensive drugs | 4 000 |
| A23.01.001 | 37.0.11 | Extraction of surgical material using delivery means (calculated price) | 1 000 |
| A18.05.013 | 37.0.22 | Treatment using blood products (calculation, price) | 1 000 |
| A11.12.003 | 37.0.23 | Treatment using additional drug therapy (calculation, price) | 1 000 |
| A23.01.001 | 37.0.24 | Selection of implants (calculation, price) | 1 000 |
| S01.002.001 | 37.0.25 | Selection of compression garments (calculation, price) | 1 000 |
| B01.057.001 | 37.0.28 | Appointment with an operating specialist | 0 |
| A11.01.014 | 37.0.29 | Hemostasis using local hemostatic agent Zhelplastan 2.5 g | 6 600 |
| A11.01.014 | 37.0.30 | Hemostasis using local hemostatic agent Zhelplastan 5.0 g | 12 700 |
| A11.12.003.002 | 37.0.31 | IV drip infusion of Ferinject 500 mg (Ferinject, 50 mg/ml, 2 ml No. 5 in ampoules or 50 mg/ml, 10 ml in a bottle), duration up to 30 minutes | 8 000 |
| А11.12.003.003 | 37.0.32 | IV drip infusion of Ferinject 1000 mg (Ferinject, 50 mg/ml, 10 ml in bottle No. 2), duration up to 30 minutes | 15 000 |
| S01.001.008 | 37.0.1.1 | Stay in a hospital room (overnight) | 3 000 |
| S01.001.009 | 37.0.4.1 | Stay in hospital room VIP 1 (no more than 12 hours) | 5 000 |
| S01.001.010 | 37.0.5.1 | Stay in hospital room VIP 2 (no more than 12 hours) | 8 000 |
Contraindications, possible complications and side effects during surgical defloration.
The likelihood of side effects and complications after surgical defloration is extremely low. Undesirable consequences of the operation may include:
- pain in the genital area in the first days after surgery;
- general internal discomfort;
- introduction of infection;
- bleeding;
- elevated temperature.
If such symptoms appear, you should immediately consult a doctor to find out and eliminate the cause of the problems.
As for contraindications, these, in addition to general surgical ones, include the presence of cancer or acute inflammatory diseases of the genital organs and blood clotting disorders.
Indications for surgical deflowering
Surgical defloration is a fairly rare operation, but there are many reasons when it cannot be avoided. So, correction can be carried out for medical reasons:
- the hymen is too dense, preventing normal sexual intercourse;
- high elasticity of the film (it stretches but does not tear);
- late age for natural defloration (after 30 years the hymen becomes very dense).
The film that covers the entrance to the vagina begins to lose elasticity from the age of 18-20, and every year its density increases. In addition, the structure of the hymen is different for each woman.
Sometimes girls come to us with a rare pathology - hymenal atresia (complete fusion). A normal film has a perforation through which blood comes out during menstruation; if it is absent, the blood stagnates, provoking the development of serious inflammatory processes and other complications.
The second category of indications for surgical deflowering is a psychological factor: fear of the first sexual contact, desire to make this process easier for oneself and one’s partner. This is a normal desire, which often helps to completely and permanently get rid of the fear of sex.
Recently, many girls prefer to tear the hymen using a scalpel or laser. The reason is that with a natural rupture of the hymen, a flap is often left that is wrapped inside the vagina. As a result, during sexual contact, a woman experiences pain and discomfort, receiving complete suffering from sex instead of pleasure. To avoid such negative consequences, it is sometimes easier to undergo a simple correction, during which the septum is excised quickly and easily.
So there is no need to be shy about this procedure, it is performed all over the world, including in our clinic, so if you decide to use this service, we are always ready to help you.
How is the procedure done?
The dissection procedure takes very little time. With sufficient skill of the operating doctor, there is practically no pain after the procedure. If necessary, you can take a painkiller tablet.
- Preliminary preparation - consultation with a specialist in intimate surgery, testing (smears for flora, blood for syphilis, HIV, hepatitis B and C; test for anesthetics - according to indications).
- The technique is a radiosurgical method, i.e. artificial defloration is carried out using a radio wave or a scalpel; other piercing and cutting instruments are not used.
- Anesthesia - local anesthesia, modern imported anesthetics, pain is excluded. Let us separately focus on two points - technique and anesthesia.
- Which anesthesia to choose - general or local? General anesthesia carries risks and side effects, significantly increases the cost of the process and is completely unjustified for this manipulation. Modern imported local anesthesia, used in our clinic when performing hymenotomy, completely eliminates any pain.
- Surgical defloration with laser - is it better or not? The use of a laser beam when cutting any tissue is technically more convenient for the doctor, but it leads to the formation of burn surfaces, which, by definition, will make it more difficult and longer for the patient to heal. Incision of the hymen with a radio wave or scalpel is preferable, because these adverse reactions and similar complications are absent.
- Duration - 15-30 minutes, depending on complexity; observation after surgery - 1-2 hours (if necessary).
- Possibility of performing a hymenotomy on the day of treatment
- Confidentiality and anonymity of treatment, out-of-town patients
- The total time spent (from entering the clinic and leaving after defloration is done) is about 2 hours.
What is surgical defloration?
Surgical defloration is an operation to remove the hymen, performed in a clinic, for medical reasons or at the request of the patient. As a rule, girls consult a doctor in cases where, when trying to lose their virginity in the usual way, they experience severe pain that they cannot bear.
Thus, surgical defloration will be the best option in the following cases:
- the hymen is too elastic and stretches well, but does not tear;
- the hymen is too dense;
- complete overgrowth of the hymen, as a result of which menstrual blood accumulates in it;
- increased sensitivity to pain;
- psychological fear of the first sexual intercourse.
The operation itself is considered simple and does not require special preparation. After a preliminary consultation with a gynecologist, you will need to undergo tests:
- urine test (general);
- blood test to determine its coagulability (biochemical and general);
- blood test to determine blood group and Rh factor;
- blood test for HIV, syphilis, hepatitis;
- smear on flora.
Based on the results of a visual examination and examination of tests, a final decision is made on the possibility of performing the operation.