Erysipelas, or simply erysipelas, is an infectious-allergic disease that affects the skin and subcutaneous tissue. The disease is quite common and prone to relapse. It ranks fourth among all infectious diseases and is also becoming more common over time. Thus, over the past twenty years, the number of relapses of this disease has increased by 25%. Moreover, a severe form of the disease is becoming more common - now it is about 80% of cases, although 50-60 years ago only 30 percent of patients were diagnosed with a severe form.
At-risk groups
Most often, women over 50 years of age are affected by this disease, but it can also occur in infants. In their case, infection occurs after streptococcus enters the wound of the umbilical region. There is no explanation for this fact, but people with blood group III suffer from erysipelas more often. There is also a connection with the place of residence. In South Asia, as well as in Africa, this disease is very rare.
People with a low level of immunity, weakened by illness, stress, treatment and other factors are at risk.
Relapses of the disease
Erysipelas that occurs repeatedly in the same place is recurrent in nature. Relapses are divided into early and late. Early relapses are considered repeated episodes of the disease that occur before 6 months, late relapses - more than 6 months.
The source of infection is foci of chronic infection, from which streptococci spread through the blood throughout the body, as well as latent (hidden) foci of infection in the dermis, where streptococci turn into the parasitic L-form during a lull period.
Chronic venous insufficiency, lymphostasis, diabetes mellitus and improper treatment of the disease contribute to recurrence. Relapses are often observed in patients working in unfavorable conditions and in the elderly.
When multiplying in the lymphatic capillaries of the skin, streptococci form an inflammatory focus in the dermis. Frequent relapses occur with low body temperature and moderate symptoms of intoxication. Oily erythema and swelling appear on the skin. The demarcation from healthy areas is weakly expressed.
Frequent relapses lead to the development of fibrous changes in the dermis and subcutaneous tissue with the subsequent development of elephantiasis.
Rice. 22. In the photo there is erysipelas (erysipelas) of rare localization.
Symptoms
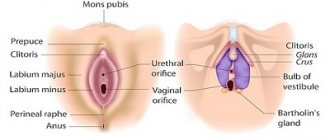
You can notice the first symptoms of erysipelas on different parts of the body: legs, arms, face, torso, perineum. Moreover, much will depend on how exactly the disease develops. For example, inflammation on the face can be localized around the eye socket, near the ear, on the scalp and neck. If the disease starts from the nose, a butterfly-type lesion may develop - extending to the cheeks. At the same time, swelling occurs, which distorts the size of the tissue. The same applies to all other organs - the localization of the disease is different and depends on the situation.
Symptoms of erysipelas are divided into general and local. General points include:
- Chills, fever. Patients often shake violently.
- High temperature, up to 40 degrees. It can last up to ten days.
- Convulsions, clouding of consciousness, delirium.
- Very strong weakness, dizziness.
- Nausea, often vomiting.
- Pain in muscles and joints.
In other words, symptoms of general poisoning of the body are observed.
Local symptoms of erysipelas look like this:
- Redness of the skin at the site of the lesion. Usually changes are noticeable ten to twenty hours after the pathological processes begin.
- Puffiness, swelling, pain in the place where the skin rises. Also, the area of skin becomes warmer to the touch, even hot. The patient may feel a burning sensation and a sensation as if something is bursting the skin from the inside.
- Rapid growth of inflammation, since streptococci multiply quite actively. The edges of the lesions are uneven, they constantly change as they grow.
- Enlargement of nearby lymph nodes as the pathogen spreads through the lymphatic system.
- Bubbles with clear liquid. They are small at first, but then they grow and unite with each other. This sign is not always present.
- Hemorrhages. If you do not help the patient at first, complications will occur, including damage to the blood vessels, the blood of which enters the intercellular space.
- Bubbles with blood and pus surrounded by areas of hemorrhage. The classification of erysipelas suggests different degrees of development of the disease - and these manifestations are already characteristic of complicated forms.
The more advanced the situation, the higher the risks that even after successful treatment a relapse will occur. Often the disease occurs in the same place as the first time.
How does erysipelas occur (pathogenesis of erysipelas)
Inflammation in erysipelas is most often localized on the face and legs, less often on the arms, torso, scrotum, perineal area and mucous membranes. The inflammatory process during the disease affects the main layer of the skin, its framework - the dermis. It performs supporting and trophic functions. The dermis contains many capillaries and fibers.
Inflammation in erysipelas is infectious and allergic in nature.
- Waste products and substances released when bacteria die cause the development of toxicosis and fever.
- The cause of the development of the inflammatory process is the effect on tissue of toxins, enzymes and antigens of hemolytic streptococci, as well as biologically active substances. Small arteries, veins and lymphatic vessels are damaged. The inflammation is serous or serous-hemorrhagic in nature.
- Human skin antigens are similar in structure to streptococcal polysaccharides, which leads to the development of autoimmune processes when the patient’s antibodies begin to attack their tissues. Immune and autoimmune complexes cause damage to the skin and blood vessels. Intravascular blood coagulation develops, the integrity of the capillary walls is disrupted, and local hemorrhagic syndrome is formed. As a result of vasodilation, a focus of hyperemia and vesicles appear on the skin, the contents of which are serous or hemorrhagic in nature.
- Biologically active substances enter the bloodstream in large quantities, including histamine, which is involved in the development of hemorrhagic forms of erysipelas.
- Insufficiency of lymph circulation is manifested by edema of the lower extremities. Over time, damaged lymphatic vessels are replaced by fibrous tissue, which leads to the development of elephantiasis.
- The focus of infectious-allergic inflammation consumes large amounts of glucocorticoids. This leads to the development of extra-adrenal insufficiency. Protein and water-salt metabolism are disrupted.
Rice. 6. The inflammatory process during the disease affects the main layer of the skin, its frame - the dermis.
Causes
Erysipelas is caused by streptococci - or rather, one of the varieties of bacteria of this group. In an organism with a weakened immune system, streptococcus can cause other diseases - for example, scarlet fever, myocarditis, and sore throat.
About 15% of the world's people are carriers of streptococcus. That is, their immunity is quite strong so as not to get sick, but at the same time they spread the infection. It is transmitted through personal contacts, household objects, airborne droplets, etc.
Predisposing factors for infection:
- Various skin injuries, including insect bites, animal bites, bedsores and ulcers. Even venous catheters can be dangerous in this sense.
- Harmful working conditions - when the skin is constantly exposed to chemicals, it often becomes dirty. People who constantly wear rubber clothing and shoes are also at risk.
- Viral skin lesions - chickenpox, shingles, herpes. They not only violate the integrity of the integument, but also greatly reduce immunity.
- Chronic skin lesions such as eczema, atopic dermatitis, psoriasis, etc.
- Purulent lesions of the skin: boil, carbuncle and similar formations.
- Disturbances in the circulatory system - varicose veins, thrombophlebitis. If the skin is deprived of oxygen, it becomes damaged and becomes more susceptible to infection.
- Various scars, the cells of which the body itself can attack, which is why erysipelas develops.
- Fungal diseases of the scalp and feet.
- Serious complications with rhinitis, otitis media, conjunctivitis.
- Injuries to the skin caused by wearing tight clothing that rubs and disrupts blood circulation in the tissues.
- Any reasons that suppress the immune system: taking certain medications, serious illnesses, exhaustion as a result of malnutrition, hypothermia, bad habits, chronic or severe stress and much more.
To summarize, the disease develops against a background of weakened immunity and streptococcal infection, which can occur in different ways.
Erysipelas
There are 20 types (serogroups) of streptococci. The most significant of them are streptococci of serogroups A, B, C, D and G. Beta-hemolytic streptococci of group A (Streptococcus pyogenes) are the cause of many dangerous diseases in humans - pustular diseases of the skin and soft tissues (abscesses, cellulitis, boils and osteomyelitis) , tonsillitis and pharyngitis, bronchitis, rheumatism, scarlet fever and toxic shock. Erysipelas can be caused by any type of group A streptococcus.
Bacteria have a round shape. They are often arranged in chains, less often in pairs. They reproduce by dividing in two.
- In the external environment, including sputum and pus, the bacteria persist for months and survive at low temperatures and freezing.
- High temperature, sunlight and disinfectant solutions have a detrimental effect on microbes.
- Streptococci show high sensitivity to antibiotics, resistance to which they develop slowly.
Streptococci secrete a number of endo- and exotoxins and enzymes that cause their damaging effects.
Rice. 2. Streptococci have a round shape. They are often arranged in chains, less often in pairs.
Rice. 3. Beta-hemolytic streptococci of group A, when growing on blood agar, form zones of hemolysis (light halos) that are 2 to 4 times larger than the diameter of the colonies themselves.
Rice. 4. When growing on nutrient media, colonies of streptococci are shiny, drop-shaped, or gray, matte and granular with uneven edges, or convex and transparent.
Diagnostics
If the first signs of erysipelas occur, you should consult a dermatologist or therapist. Depending on the extent of the problem, assistance from specialists such as an immunologist, surgeon, or infectious disease specialist may be required.
Diagnosis of the disease includes interviewing the patient, as well as a thorough examination. Then tests are prescribed for the level of T-lymphocytes, ESR, and the number of neutrophils (all this is determined through a blood test).
An optional bacteriological examination is prescribed to determine the causative agent - doctors do not agree on the advisability of such an examination.
Erysipelas in children
Erysipelas are rare in children. In older children, the disease is mild. The focus of erysipelas can occur in different places. The erythematous form develops more often. The prognosis is favorable.
In children under one year of age, erysipelas is more severe. Foci of inflammation often appear in areas of diaper rash and on the face, sometimes spreading to other parts of the body. With the phlegmonous form of the disease, sepsis can develop, with erysipelas of the face - meningitis.
Erysipelas develops severely when streptococci penetrate into the umbilical wound in newborns. The process quickly spreads to the child’s back, buttocks and limbs. Intoxication increases, body temperature rises significantly, and convulsions appear. Some patients develop sepsis. Mortality from erysipelas in newborns is extremely high.
Rice. 24. The photo shows erysipelas in children.
Treatment
If erysipelas develops on a leg, arm or other part of the body, the approach will always be comprehensive - local treatment alone is simply not enough. Moreover, the emphasis is largely on increasing immunity, otherwise the risks that the disease will recur are very high. Special medications are used to work with the immune system, but it is important for the patient to change their lifestyle: rest well, carefully monitor their health, eat right, and eliminate negative factors.
In the treatment of erysipelas, antibiotics are used, as well as antibacterial drugs from other groups. Drug therapy is selected individually - you should not prescribe medications yourself under any circumstances.
Along with taking medications, it is necessary to treat the affected skin: with special solutions, powders, aerosols. And the ointments that people love to prescribe for themselves - synthomycin, ichthyol, Vishnevsky - are strictly prohibited in this case, since they can provoke complications and cause the development of an abscess. The use of traditional medicine in any form is not allowed - in the treatment of erysipelas it is extremely dangerous!
Patients must have a preventive conversation regarding the nuances of hygiene during treatment. So, you need to change bed linen every day, take care of air access to the affected area, and regularly take a shower in warm, very comfortable water. Do not wipe the skin - only soak it with paper towels.
Physiotherapeutic methods are also used for erysipelas: ultraviolet irradiation, magnetic therapy, UHF, electrophoresis, certain types of laser therapy, applications with warm paraffin. At each stage of treatment, specific procedures are prescribed, and they are selected individually - for each patient and his condition. Any amateur activity is also inappropriate here, otherwise you can harm your health.
Very serious complications require surgical treatment.
If you encounter such a problem, we recommend immediately contacting the JSC Medicine clinic. We are located in Moscow and have a large staff of professional dermatologists, therapists and other specialists who can help you. And modern conditions for diagnosis and treatment will help achieve results much faster.
If doctors begin treatment in a timely manner and the patient follows all recommendations, the disease can be cured within 10-14 days.
Factors influencing the development of erysipelas
The development of erysipelas is influenced by the following factors:
- Individual predisposition to the disease, which is caused by genetic predisposition or increased sensitivity to allergens of streptococci and staphylococci.
- Reduced activity of the body's defense reactions - nonspecific factors, humoral, cellular and local immunity.
- Disorders of the neuroendocrine system and imbalance of biologically active substances.
Prevention
Since the disease can affect anyone, prevention of erysipelas is important both for those who have already had the disease once, and for those who have only heard about such a disease.
Prevention consists of following the following tips:
- Treat any inflammation on the skin or mucous membranes in a timely manner.
- Maintain personal hygiene. In the event that work or lifestyle is associated with additional pollution, hygiene should be even more thorough, but not excessive, so that the skin does not suffer - otherwise the effect will be the opposite.
- Use special products (gels and oils) for washing that do not dry out the skin. Regular soap is not suitable for regular use.
- Carefully monitor the condition of your skin in hot weather or if you have folds that constantly sweat. In this case, it is necessary to use special powders.
- Pay close attention to your health if you have problems with blood vessels or lymph stagnation. Such people are recommended for massages and various procedures that disperse fluids in the body.
- Treat your skin immediately if you have frostbite, chapping, or sunburn.
- Wear comfortable, breathable, natural clothing if possible that fits loosely on the body.
- Carefully monitor your immunity and eliminate all factors that can weaken it.
Remember that you cannot insure against this disease, but you can do everything to reduce the risks of its occurrence.
Classification of erysipelas
- There are erythematous, erythematous-bullous, erythematous-hemorrhagic and bullous-hemorrhagic (uncomplicated) and abscessing, phlegmonous and necrotic (complicated) forms of erysipelas. This classification of erysipelas is based on the nature of local lesions.
- According to the severity of the course, erysipelas is divided into mild, moderate and severe.
- According to the frequency of manifestation, erysipelas is divided into primary, repeated and recurrent.
- There are localized, widespread, migratory and metastatic forms of erysipelas.
By prevalence
- When a limited area of lesion appears on the skin, they speak of a localized form of erysipelas.
- Extension of the lesion beyond the anatomical region is regarded as a common form.
- When one or more new areas appearing near the primary lesion, connected by “bridges,” they speak of a migrating form of erysipelas.
- When new foci of inflammation appear far from the primary focus, they speak of a metastatic form of the disease. Streptococci spread by hematogenous route. The disease is severe and long-lasting, often complicated by the development of sepsis.
By frequency of occurrence
- Erysipelas that occurs for the first time is called primary.
- If a repeated case of the disease occurs in the same place, but not earlier than 2 years after the first case, or if a repeated disease occurs that arose in another place earlier than this period, they speak of recurrent erysipelas.
- Erysipelas that occurs repeatedly in the same place is recurrent in nature.
By severity
- Mild severity of the disease is characterized by short-term fever and mild symptoms of intoxication, which is characteristic of the erythematous form of erysipelas.
- Moderate severity is characterized by longer-lasting (up to 5 days) fever and more pronounced symptoms of intoxication, which is typical for the erythematous and erythematous-bullous forms of the disease.
- The severe course of erysipelas is characteristic of hemorrhagic and complicated forms of the disease, which occur with high (up to 400C) body temperature, severe intoxication, and the development in some cases of infectious-toxic shock and sepsis. Severe course is observed in migratory and metastatic forms of the disease.
Erased or abortive forms of the disease are observed with adequate, timely treatment. They are rare.
Rice. 7. The photo shows erysipelas of the skin.
Irritative dermatitis
In irritative dermatitis, the rash may be caused by physical or chemical irritation and damage to the skin, in which case it is not usually associated with an allergy. This type of damage can be caused by soap, detergents, food products, and building materials.
The necessary examination and adequate modern treatment for each form of dermatitis can be determined by highly qualified specialists of our center - the Three I Immunology Clinic - allergists and dermatologist. Come visit us at Novosibirsk, st. Galushchaka, 2, we will help solve your problems!
Discoid dermatitis
Discoid dermatitis is characterized by the appearance of round or oval spots in symmetrical areas, often on the extensor surfaces, usually in adult patients. Exogenous causes must be excluded.
Dyshidrosis is a variant of eczema in which recurrent vesicles or bullae affect the palms, fingers, toes, or both. The disease is characterized by remissions and exacerbations, which are sometimes provoked by fever, emotional stress, and active fungal infection.
Complications of erysipelas
Complications of erysipelas occur in 4 - 8% of cases. A decrease in the activity of the body’s defense reactions and inadequate treatment lead to the development of:
- lymphorrhea - leakage of lymph from damaged lymphatic vessels,
- ulcers - deep skin defects,
- abscess - an abscess surrounded by a dense capsule,
- phlegmon, when inflammation spreads to subcutaneous fatty tissue and connective tissue,
- gangrene - complete destruction of tissues affected by inflammation,
- thrombophlebitis - inflammation of the venous walls with the formation of blood clots,
- pneumonia in elderly people,
- lymphostasis (lymphedema), which developed as a result of impaired lymph outflow and elephantiasis (fibredema),
- infectious psychosis,
- At the site of inflammation, hyperkeratosis, eczema, and pigmentation often develop over a long or recurrent course.
Immunity does not develop after suffering from erysipelas.
Rice. 25. Lymphostasis and elephantiasis during erysipelas often lead the patient to disability.
Rice. 26. A terrible complication of erysipelas is phlegmon.
Rice. 27. In the photo, gangrene of the lower limb is a complication of the bullous-hemorrhagic form of erysipelas.