What is molluscum contagiosum
This is a viral skin pathology that mainly occurs in children under 10 years of age.
The disease also occurs in young people aged 20-30 years, during the period of their most active sexual life. This disease is characterized by the appearance of hemispherical nodules with a diameter of 2-5 millimeters on the skin or mucous membranes. Regarding the prevalence of this infection, rates in different countries vary from 1 to 22%. It is difficult to determine the exact incidence rate because the virus is easy to spread. To do this, you just need to come into contact with a patient or a virus carrier. The virus remains active for some time on the surface of objects, so infection is also possible when using things and objects shared with the patient.
Molluscum contagiosum is not considered a dangerous disease. It does not threaten the life and health of a child or adult. The presence of the disease, as a rule, indicates a reduced immune status. This is why the infection most often affects children whose immunity is just developing. The risk group also includes people with congenital or acquired immunodeficiency.
Important! You can become infected with molluscum contagiosum again. After illness, patients do not develop stable immunity, which makes reinfection possible. Minimizing the risk of infection is mainly associated with strengthening the immune system and compliance with preventive measures.
Similarities with other diseases
Molluscum contagiosum consists of a huge number of elements. This is why it is very easy to confuse it with other skin diseases.
These include:
- Genital warts;
- Flat warts;
- Vulvar micropapillomatosis;
- Hyperplasia of the sebaceous glands;
- Pearly penile papules;
- Syringiomas.
If a single large element is detected, differential diagnosis is made with keratoacanthoma, basal cell and squamous cell skin cancer.
Causes of molluscum contagiosum
The causative agent of the disease is viruses of the orthopoxvirus family, which belong to the smallpox virus family. Molluscum contagiosum virus is abbreviated as MCV (Molluscum contagiosum virus). Today, 4 varieties of such viruses have been identified, but the most common viruses in the human population are MCV-1 and MCV-2. Moreover, if the first occurs in adults and children, the second occurs mainly in adults, since it is transmitted through sexual contact. Characteristic skin manifestations of infection appear in those areas where the virus has penetrated. Most often these are the limbs, face or genitals.
Molluscum contagiosum virus. Photo: PHIL CDC
All smallpox viruses, including orthopoxviruses, are large DNA viruses. This means that the mutation rate of such viruses is much lower than that of RNA viruses (for example, influenza viruses). This is due to the fact that when copying genetic material, DNA viruses use DNA polymerase, which also performs editing functions, clearing the genome of mutations.
The incubation period for this pathology ranges from one week to several months. Most often it is 2-8 months. In most adults and children, characteristic symptoms develop within a specified period of time after infection.
Important! A patient with molluscum contagiosum remains contagious until all skin manifestations disappear.
TOP 5 methods for removing formations
There is more than one technique that allows you to get rid of this problem in a short period. Let's look at them in more detail.
Laser exposure
Under the influence of a laser beam, the skin with molluscum rashes overheats, which helps to destroy the causative viruses. Damaged cells also evaporate.
The laser penetration depth into the skin layers is no more than 5 mm, which cannot cause harm to the tissues in the vicinity.
The procedure is absolutely safe for both children and adults. Does not cause any discomfort or pain. It is carried out in sterility and prevents further spread of the virus.
After you have managed to get rid of molluscs on your face, you should protect the treated areas for the first 3 days. You cannot go to the pool or sauna, or sunbathe for a long time in the sun or in a solarium.
Using liquid nitrogen
You can get rid of such a scourge as mollusks on the face with the help of chilled liquid nitrogen.
By freezing the contents of the papules, the process is inhibited. Against this background, damaged tissues disintegrate.
This procedure is safe and painless, keeps nearby healthy cells intact and does not leave scars.
Thus, it is recommended to remove shellfish from the child’s face. The treatment is effective, and most importantly, one-time. In the future, there is no need to take any medications.
Electrocoagulation method
Molluscum contagiosum is destroyed by exposure to a special coagulator spray with the simultaneous influence of variable frequency currents. This destroys pathological bodies and affected dermal cells.
Local anesthesia is used to relieve the pain threshold. Upon completion of the procedure, crusts remain on the treated areas, which quickly heal without a trace.
Surgical scraping of papules
If there are few bubbles, then surgical curettage is prescribed. Approximately an hour before surgery, the area with papules is lubricated with an anesthetic cream.
Then a sterile bandage is applied on top, which is removed immediately before the operation. The skin is wiped and the procedure begins.
To scrape the papules, a special tool is used - a curette or a wooden spatula pointed at the end. Sometimes tweezers are used.
When all contents have been removed, the skin is treated with iodine. During the process, bleeding is possible, which subsequently leads to scarring.
Getting rid of papules with chemicals
The method is simple to implement, but quite productive. It involves daily application of ointments and solutions with an antiviral spectrum of action to the nodular rash:
- Fluorouracil or Oxolinic ointment;
- Gels containing benzoyl peroxide;
- Tretinoin;
- Imiquimod;
- Infagel;
- Vartek;
- Kondilin;
- trichloroacetic acid solution;
- salicylic acid.
It is enough to do this twice a day. Complete cure occurs in 4-10 weeks.
The products are applied point-by-point - exclusively to the neoplasms themselves. At the same time, they try not to affect living tissue.
Methods of infection and provoking factors
Infection with the virus occurs through contact with a patient or carrier of the virus. Using things and objects shared with the patient also poses a danger, since orthopoxviruses remain active for some time on various surfaces. For this reason, children often become infected when visiting sports sections, where the likelihood of infection spreading is especially high due to the large crowd of people who use the same sports equipment. Contact sports (such as combat sports) also pose a risk because close contact increases the likelihood of transmitting the virus.
Children's judo section. Photo: nomadsoul1 / freepik.com
In young people who are sexually active, infection most often occurs through sexual contact. As in young children, in older people the provoking factor for infection is weakened immunity. HIV-infected people, as well as people suffering from atopic dermatitis, are at risk. One of the factors in the development of the disease is long-term use of glucocorticoid drugs and cytostatic agents that reduce the activity of the human immune system.
Important! If molluscum contagiosum is sexually transmitted, many people mistakenly believe that they can protect themselves from the virus by using a condom. This is a big misconception, since a condom is only effective in protecting against infections concentrated directly in the urethra, penis, semen or vagina. It is impossible to completely protect yourself from sexually transmitted infections such as molluscum contagiosum, syphilis or genital herpes using a condom.
Folk remedies for fighting shellfish (4 recipes)
Treatment of molluscum on the face with folk remedies is possible in different ways, for which there are many effective recipes. They include both individually and in combination herbal and medicinal products.
The most promising options are presented in the table:
| An approach | Photo | Instructions |
| Garlic | Grind the garlic to a paste and mix with softened butter. The proportions are maintained at 1:1. Distribute the mass over gauze and apply it to the papules, fixing it with an adhesive plaster. Change the lotions to fresh ones three times a day. You can wipe the affected areas with garlic alone (cut into a clove). The course of treatment is a week. | |
| Potassium permangantsovka | Cauterization is carried out with a manganese solution. | |
| Iodine, hydrogen peroxide, calendula tincture | Apply any product directly to the tumors with a cotton swab, being careful not to infect healthy skin. Medical alcohol is applied around the papules. Then the nodules are carefully squeezed out and treated with alcohol. Cauterize with iodine, hydrogen peroxide or calendula. It is advisable to wash clothes and bedding to prevent re-infection. After the procedure, you should not wet the wounds and carry out disinfection with iodine every day. As soon as crusts appear, use oxolinic ointment. | |
| Celandine juice | Lubricate the rash with freshly squeezed juice of celandine or dandelions. Eucalyptus also helps a lot. |
Symptoms
The main symptom of a skin infection is painless nodules 2-5 mm in diameter with a small dimple in the center. Let's take a closer look at the main characteristics of rashes and other symptoms.
- The rashes have the appearance of dome-shaped papules. The surface of the papules may be smooth or waxy. The consistency of the papules is dense, and as the tumor grows it softens. In patients with HIV infection, as well as in people with weakened immune systems, the diameter of the rash reaches 10-15 mm.
- Papules are flesh-colored, pink, or darker in color. When pressed, curdled contents come out of the papule. Sometimes pearlescent stains, like a pearl, are clearly visible on the papules.
- Papules form at the sites of viral infection penetration - in various parts of the body. They are often grouped into one or two areas, but diffuse distribution of papules over a specific area of the skin is also possible. Often in people with weakened immune systems, the rash affects large areas of the skin.
- The rash is painless, but the area of the rash may become inflamed, which is accompanied by itching.
- In approximately 10% of cases, patients develop eczema in the affected area - an inflammatory skin lesion (dermatitis).
- Papules never appear on the palms or soles. Very rarely, rashes form on the mucous tissues of the oral cavity.
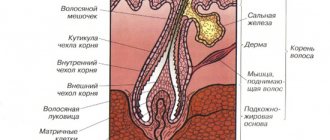
- Skin tumors with molluscum contagiosum grow slowly. The papule increases in size and is filled with a light, cheesy mass consisting of skin cells, sebaceous gland secretions, as well as dead leukocytes and the viral particles themselves.
- Around the 12th week, papules reach their peak size, after which their growth stops. Then the tumors gradually die off.
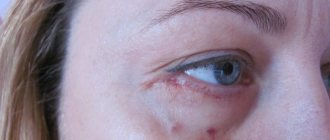
Figure 1. Molluscum contagiosum rash on the face. Source: Ben Naafs/Community Eye Health/Flickr
Symptoms in women
In adults, rashes most often affect the genital area. This is due to the predominance of transmission of infection through sexual contact. For infection, genital contact itself is not at all necessary; just contact with the infected area of the partner’s skin is sufficient.
Most often in women, papules form in the lower abdomen, on the thighs, pubic area or external genitalia.
It is noteworthy that pregnant women are especially susceptible to infection due to a natural decrease in immunity. The manifestations are indistinguishable from the classic clinical picture of the disease. The virus does not pose a threat to the life and health of the fetus. However, if the baby comes into contact with the mother's infected skin, the child runs the risk of becoming infected.
Symptoms in men
In men, as in women, the rashes are predominantly located in the genital area. This is the groin area, penis, inner thighs. Men are more likely than women to rub papules on clothes, which leads to the release of viral particles and re-infection. Therefore, the rash affects not only the area of contact with the infected partner, but also nearby areas.
How does the infection manifest in children?
Skin manifestations in children mainly affect the face, limbs and chest area. The rashes do not cause any inconvenience to children other than aesthetic ones, especially if they are located on the face. Papules in children do not hurt and very rarely cause itching. It is important to ensure that the child does not scratch or rub the affected areas. Otherwise, secondary infection with the virus will occur.
Important! In children, rashes are extremely rarely observed in the genital area. If a child has papules on the genitals, pubis, buttocks or inner thighs, the circumstances of possible infection should be especially carefully examined, since sexual abuse cannot be ruled out.
Transmission routes
To protect yourself as much as possible, you need to know which routes of transmission of molluscum contagiosum are common. In this case it is:
- Household contact with a sick person or with contaminated things. Usually these are the patient’s personal belongings - for example, a towel.
- Sexual contact with an infected person. Often the rashes are localized on the genitals, lower abdomen and inner thighs.
- Transmission from mother to child. This is not a common option, but it is still possible.
- Infection during the tattooing process occurs in situations where the instruments are unsterile and the artist does not follow safety rules.
If there is a person with such an infection in your immediate environment, you need to be very careful, since the routes of transmission of molluscum contagiosum are quite simple.
Types of molluscum contagiosum
There is no generally accepted classification for molluscum contagiosum. At the same time, in addition to the “classical” papules, atypical forms of rashes are distinguished. These include:
- giant clams, the size of which is 3 cm or more;
- cystic molluscs - the appearance of cysts (cavities, with a wall and contents) instead of papules of the same size;
- ulcerated mollusks - instead of nodules, small areas of erosion appear, which subsequently turn into bleeding ulcers;
- molluscs in the form of eels or warts;
- pendicular mollusks - neoplasms are located on a thin stalk above the skin.
Depending on the prevalence of lesions, two forms of the disease are distinguished:
- Localized - affects only a specific area of the body, such as the face, genital area, upper or lower extremities.
- Generalized - rashes are observed over a large surface of the body. In some cases, neoplasms are noted throughout the body.
Forms
The main form of molluscum contagiosum in children or adults is typical. It has the symptoms described above.
There are also atypical (very rare) forms, for example:
- Keratinizing molluscs. In this case, the skin on the rash is very flaky and comes off the surface in scales.
- Cystic molluscs. Where a nodule immediately forms, cysts subsequently grow.
- Giant clams. Such rashes can grow up to three centimeters in diameter or even more.
These are not all forms of atypical molluscum contagiosum, but the risks of encountering them are minimal.
Treatment of molluscum contagiosum
Source: Fantasy Children's Clinic
Before starting treatment, a diagnosis is carried out, which is not difficult for molluscum contagiosum. The diagnosis is made based on the external manifestations of the disease. For atypical forms, specific laboratory tests are used to identify viral particles. This is staining of the contents of nodules according to Romanovsky-Giemsa, Papanicolaou or Wright. Instrumental diagnostics for molluscum contagiosum are not used.
There is no specific treatment for molluscum contagiosum. Treatment is aimed at eliminating skin lesions as quickly as possible. The disease is treated on an outpatient basis by a dermatologist.
Treatment for molluscum contagiosum is not always carried out, since within 6-18 months the papules “go away” on their own. Treatment measures are resorted to based on aesthetic considerations, as well as in severe cases of the disease (when a significant part of the body is affected by rashes) and when patients at risk are infected (people with HIV and a weakened immune system).
Drug treatment
Drug therapy is ineffective. However, to eliminate papules, salicylic acid is used as an external agent. The healing of rashes in this disease is also facilitated by topical preparations with retinoids (in particular, tretinoin).
To eliminate rashes, cantharidin is used, a poison contained in the hemolymph of some types of beetles. Currently, cantharidin is used as a blister agent. In particular, one drop of cantharidin is applied to the papule of molluscum contagiosum. In this case, blisters may appear at the application site. Cantharidin has not yet been registered in the Russian Federation and cannot be used.
Cytostatic drugs (podophyllotoxin) and potassium hydroxide are also used for medicinal purposes. However, the effectiveness of these drugs, as well as the above, for molluscum contagiosum is extremely low.
Antiviral drugs
Since molluscum contagiosum is a viral disease, it is logical to assume that antiviral drugs can help in treatment. Unfortunately, here too the existing arsenal of antiviral drugs turned out to be powerless against the molluscum contagiosum virus. Some doctors prescribe acyclovir and oxolinic ointment to such patients, but these drugs are ineffective against the molluscum contagiosum virus. Currently, antiviral drugs acting directly against the molluscum contagiosum virus have not yet been developed.
Immunomodulators
Some doctors may prescribe immunomodulatory and immunostimulating drugs to patients. For example, this is imiquimod, a drug that enhances local immunity; Local drugs with inducers of interferons, proteins that have antiviral activity, are also prescribed. However, there are no studies confirming the effectiveness of such drugs for molluscum contagiosum.
Thus, in the treatment of molluscum contagiosum, medications and folk remedies are either ineffective or useless. An effective way to eliminate rashes are methods of direct papule removal.
Surgery
The following surgical techniques are used to remove molluscum contagiosum papules:
- Cryosurgery is treatment using liquid nitrogen. The papule is exposed to liquid nitrogen for a few seconds, which leads to its deep freezing and destruction. Since new papules may form over time, the patient will have to undergo several cryotherapy sessions. Among the disadvantages of this treatment is the painfulness of the procedure. Therefore, it is not used to treat young children. In addition, after exposure to liquid nitrogen, blisters may form, and then barely noticeable scars.
- Evisceration is the removal of a papule using thin tweezers. The advantage of the method is that the removed papule is not destroyed, which means it can be sent for laboratory testing.
- Curettage is the removal of lesions using a curette. This is a tool that resembles a long metal fork with a loop instead of teeth. This technique is painful, and after removal scars may form. As a rule, curettage is used for a small number of papules. If there are a lot of rashes, then curettage is ineffective, since after the procedure there is a high risk of new rashes appearing.
- Laser therapy - laser exposure to molluscum contagiosum papules. As a rule, one session is enough for laser removal of papules, but in some patients the rash may persist, which requires re-treatment after 2-3 weeks.
- Electrocoagulation is the removal of skin lesions using electrical cauterization. For this purpose, an electrocoagulator is used - a device that supplies high-frequency current. Under the influence of current, the proteins of the papules are destroyed, which leads to its destruction.
Molluscum contagiosum is a viral skin infection that is usually seen in healthy and immunocompromised children. The infection is caused by the molluscum contagiosum virus of the family Poxviridae. Molluscum contagiosum appears as single or multiple small white or flesh-colored papules, which usually have a depression in the center. The indentation may not always be present in younger children and, instead, the papules may have a pimple-like appearance. The lesions vary in size (from 1 mm to 1 cm in diameter) and are painless, although some patients may experience itching in the area of the rash. On average, up to 11-20 papules appear on the body and often the disease tends to resolve spontaneously. However, in immunocompromised patients, molluscum contagiosum can be a severe infection with hundreds of papules on the body. Extensive rashes indicate a late stage of immunodeficiency.
Molluscum contagiosum rashes usually begin in a localized area of skin, although the infection can spread to other parts of the body—such as the genitals, perineum, pubis, and surrounding skin—by autoinoculation. Molluscum contagiosum can be transmitted sexually, and therefore child abuse in genital or perineal locations should be considered. But, as a rule, the most common route of transmission of infection to the genitals is autoinoculation. In most cases, sexually transmitted molluscum manifests itself in the form of papules localized exclusively on the genitals. A Spanish study found that sexual transmission of molluscum contagiosum has increased since 1987. to 2007 three times.
Rarely, molluscum contagiosum can also spread from the genitals to the oral cavity, conjunctiva and cornea, most often occurring during oral-genital sex. The latter scenario may result in chronic conjunctivitis or superficial punctate keratitis, making orbital lesions more difficult to treat. Some patients may develop eczema around the papules, which is observed in more than 30% of patients and, most importantly, increases the risk of autoinoculation when scratching the eczematized parts with the spread of viral particles to other parts of the body. Chronic conjunctivitis and eczema caused by molluscum contagiosum tend to resolve spontaneously. Pre-existing eczema may also predispose children to infection with the virus. 62% of children with molluscum contagiosum in Australia suffered from eczema.
CM is transmitted through close physical contact with an infected person or through objects used by him. In the United States alone, there were 280,000 patient visits per year for molluscum contagiosum in the 1990s. While data are limited, several studies have suggested a worldwide prevalence of 5%-7.5% in the pediatric population. but the number of CM increases to 5%-18% among the HIV-positive population and even reaches 30% among acquired immunodeficiency syndrome (AIDS) patients with CD4+ below 100/ml. Infection is also observed at higher rates in certain geographic areas with tropical climates, such as Congo, Fiji, and Papua New Guinea, where incidence may approach 20% of the child population. It is not known whether this increase in prevalence is due to the genetic susceptibility of these populations to BM infection or whether BM becomes more virulent in tropical environments.
The infection in immunocompetent patients is usually self-limiting and resolves spontaneously within 6 to 9 months. One study reported spontaneous resolution in 94.5% of patients within 6.5 months after initial infection. Additionally, the same study found that 23% of study participants were cured within one month of their first consultation with a dermatologist. It should be emphasized that spontaneous resolution occurs primarily in immunocompetent patients. In contrast, people with suppressed immune systems often suffer from persistent forms of CM, which directly correlates with the level of immunodeficiency.
Biology and pathogenesis of molluscum contagiosum
CM is one of the largest human viruses. It belongs to the genus Molluscipoxvirus and contains double-stranded DNA 200-300 nm in length. The genome is covalently linked at both ends and encodes redundant, repetitive sequences at both ends. Restriction endonuclease is used to distinguish between four species of molluscum contagiosum—KM-1, KM-1a, KM-2, and KM-3—which all appear to cause very similar disease manifestations. Of these, MCV-1 is the most common, while MCV-2 usually appears in adults and is often sexually transmitted. The KM-1 genome has been completely sequenced and several novel gene products involved in pathogenesis and immune evasion have been identified: MC54L, MC148, MC013L, MC159 and glutathione peroxidase.
The MC54L protein prevents inflammation by binding to the proinflammatory cytokine human interleukin-18. 20 MC148 promotes viral replication by preventing the differentiation of infected keratinocytes. MC159 interacts with Fas (CD95 member of the tumor necrosis factor receptor family), tumor necrosis factor (TNF), and TNF binds to apoptosis-inducing ligand (TRAIL) to inhibit apoptosis. MC80R, a major histocompatibility complex (MHC) class I homologue, collides with the host, the presentation of peptides specific to CM and inhibits the cellular cytotoxicity of infected cells. Finally, infected cells express glutathione peroxidase to prevent leukocyte-mediated oxidative damage. Collectively, these viral gene products may not support an active infection while the host immune system gradually takes over.
CM enters the skin through small abrasions; this explains why CM is common in individuals with eczema and atopy, who tend to scratch inflamed areas of the skin. Next, CM penetrates into the lower layers of the epidermis and begins replication, spreading in the epidermis .
According to various estimates, the incubation period ranges from 14 days to 6 months. When active infection begins, the epidermis hypertrophies, extending into the underlying dermis. As the infection progresses, the number of viruses increases, causing the cells of the papillary layer to migrate upward, while hyperplasia of the cells of the basal layer simultaneously contributes to their replacement of the migrating cells of the papillary layer. Viral structures are rarely observed in the basal layer and the structure of the basal lamina remains unchanged. Hypertrophied epidermal cells protrude above the skin and form a characteristic tumor observed in molluscum contagiosum in the form of a papule.
Diagnostics
The morphological manifestations of CM in most cases are typical enough to establish a clinical diagnosis. However, in some cases the diagnosis can be more difficult. Using a magnifying glass or a dermatoscope, a characteristic central depression is visualized, which often helps in diagnosis. If magnification of the CM element does not allow a final diagnosis, the doctor can perform a biopsy of the affected area and conduct either histological studies or polymerase chain reaction (PCR) methods. Histopathology typically demonstrates epidermal hyperplasia with the formation of a crater filled with CM viruses. CM viruses are defined as huge (up to 35 µm) discrete ovoid intracytoplasmic inclusion bodies, large acidophilic granular masses, pushing the nucleus and numerous keratohyalin granules to the side. Although the identification of CM virus is conclusive for diagnosis, detection of the virus may be difficult in some compacted inflamed lesions . Intact BM elements display little inflammation, while disrupted elements show a mixed inflammatory response characterized by mononuclear cells, neutrophils, and multinucleated giant cells. Using electron microscopy, brick-shaped virions can be seen. Molluscum contagiosum may resemble the clinical presentation of other disorders. Rarely, they may be confused with warts and, if located on the genitals, may be mistaken for condylomas caused by human papillomavirus infection. Giant CM nodules may resemble basal cell epithelioma, keratoacanthoma, common warts, condylomas, or verrucous dyskeratoma.
Clinical management
In almost all immunocompetent individuals, molluscum contagiosum is a self-limiting disease that resolves spontaneously, usually without scarring. Resolving this infection without therapeutic intervention is one treatment strategy that also minimizes health care costs. Regardless of whether treatment is required, it is very important that the physician inform the patient to avoid swimming pools where healthy people swim and not to give personal hygiene products. healthy persons (towel, clothes, etc., children’s personal toys), avoid physical contact with other people.
Therapeutic intervention in the treatment of molluscum contagiosum is intended only to accelerate the process of elimination. A systematic review in 2009 found that there was insufficient evidence to support the use of any treatment as definitively effective. However, for rapid resolution of localized lesions, clinical experience advocates the use of curettage, cryotherapy, and some topical agents. Thus, the patient may wish to seek treatment for a variety of reasons, including: reducing pruritus, minimizing autoinoculation, and also transmission of infection to others, management of cosmetic problems, prevention of scarring, secondary infection or bleeding from lesions. Patients with sexually transmitted CM should receive early treatment to prevent spread of infection to future sexual partners. Rapid treatment is also indicated for immunocompromised patients in whom the infection may become serious.
Before starting treatment, the doctor should examine the skin of the entire body to identify any damage. Failure to treat all lesions may result in further spread of infection and autoinoculation. Curettage, cryotherapy, and cantharidin are considered first-line treatments due to their popularity and established effectiveness in resolving localized lesions. Curettage involves physically removing the lesions using a curette and is the preferred treatment choice in the Netherlands. Treatment failure is common with extensive lesions and concomitant atopic dermatitis. Local anesthetics are used to reduce pain and discomfort associated with the curettage procedure, which can be stressful for some children. .
Cryotherapy involves the use of a cotton swab soaked in liquid nitrogen with an exposure time of 6 to 10 seconds for each element. Studies have shown the advantage of cryotherapy over imiquimod cream. However, cryotherapy also has its fair share of side effects such as pain, blistering, depigmentation and soft scarring.
Cantharidin, the most popular treatment among American dermatologists, is applied directly to the lesions, usually with a cotton swab. To prevent further autoinoculation or transmission, the site of cantharidin application should then be covered with a bandage, followed by washing off the cantharidin with soap and water 2 to 6 hours after application. Treatment can be repeated every 2 to 4 weeks and is contraindicated in the presence of lesions located on the face, genitals organs or perianal area. A retrospective study showed that 90% of children treated with cantharidin for CM achieved complete cure. The average number of patient visits to achieve complete cure was 2.1. About 95% of parents of children participating in the study said they were satisfied with the treatment and would be willing to have their child treated with cantharidin again. Side effects included transient burning, erythema, pain and itching.
Several second-line therapies have been described in the literature, including (but not limited to): imiquimod, sinecatechins ointment, podophyllin, potassium hydroxide, salicylic acid, topical retinoids, oral cimetidine, pulsed dye lasers, and silver nitrate. However, the effectiveness of these treatments is controversial. In their reviews, Van der Wouden et al (2009) and Brown et al. (2006) reviewed comparative studies involving the above-mentioned second-line treatments. Patients with immunodeficiency may develop serious, persistent infections not only with BM, but also with opportunistic pathogens.
Procedures that create wounds, such as curettage, should be avoided in these patients because the wounds increase the risk of additional infection. Instead, it is recommended to use imiquimod 3 times a week. Studies have been conducted that have successfully reduced genital lesions using 0.05% ingenol mebutate gel as a spot treatment in patients undergoing kidney transplantation. In HIV-positive patients, resistant lesions sometimes resolve only after initiation of highly active antiretroviral therapy (HAART).
Regression of resistant lesions in HIV-positive patients has been achieved through the use of intravenous cidofovir, a nucleotide analogue of deoxycytidine monophosphate. However, systemic cidofovir may be toxic to the kidneys. Therefore, topical cidofovir is currently being studied as a potential therapeutic agent. The authors of one trial reported complete resolution of a severe case of CM on the face of an HIV patient 2 months after treatment with topical cidofovir 2% ointment.
Patients with atopic dermatitis are at greater risk of scarring as the number of lesions increases and curettage is not recommended for them. Before starting CM therapy, the doctor must treat atopic dermatitis with topical corticosteroids and antihistamines. Javed and Thiring, in a published report, achieved complete remission of CM in a child with atopic dermatitis using 0.015% ingenol mebutate gel. At the same time, regression of distant unprocessed CM elements was also observed. Ingenol mebutate has been approved by the US FDA for the treatment of keratosis keratoses. The mechanism of the drug is necrotization of the lesion due to neutrophil-mediated cellular cytotoxicity. Patients with periocular lesions should be referred to an ophthalmologist for further treatment.
Conclusion
There is currently no FDA-approved therapy for CM and no widely accepted standard of care. Many pediatricians prefer spontaneous resolution over aggressive therapy. However, research must continue to be conducted in hopes of finding an answer to the treatment approach for this childhood infectious disease. In addition, sexually transmitted CM should be considered not only in the interests of the patient, but also to prevent infection of the sexual partner. Most importantly, standardized therapy must be developed for immunocompromised patients, who may be severely affected by generalized CM both physically and psychologically, especially on the face and genitals.
Prevention of molluscum contagiosum
Source: Jesselton Medical Center
There is no specific prevention against molluscum contagiosum (a vaccine against the pathogen has not yet been developed). Basic preventive measures involve isolating patients to avoid infecting other people. To minimize the spread of infection, doctors recommend:
- isolate the sick person until complete recovery;
- observe the rules of hygiene;
- conduct preventive examinations for children of preschool and school age;
- be more attentive to your sexual partners - a quick examination of the person can help you avoid infection, and motivate your partner to undergo examination.
How does infection appear? Main symptoms
Infection with the virus occurs in various ways.
Both the result of sexual intercourse and domestic infection are possible.
The incubation period of molluscum contagiosum lasts from two weeks to several months.
After this stage ends, the main symptoms begin to appear.
The clinical picture of the disease is quite pronounced. Localization of molluscum contagiosum:
- external genitalia,
- hip area,
- buttocks or lower abdomen.
Raised nodules appear on healthy skin. They have a hemispherical shape. The color matches the natural color of the skin or is slightly pinker, single or multiple.
In the middle of the hemisphere there is a depression, slightly reminiscent of a human navel.
The nodules are smooth to the touch and only slightly differ from the natural color of the skin. The skin around these formations usually does not change. But sometimes the rim around them becomes inflamed. The person does not experience any particular discomfort.
A significant increase in manifestations is observed after approximately 3 weeks. And with slight pressure a cheesy plug is released.
It is worth considering that in most cases, symptoms can go away on their own after six months. Clinical manifestations are dense nodules, sometimes with a light pearlescent hue.
Painful sensations may not be observed at all. Often these are small skin rashes that are localized in certain small areas.
Such nodules can have different sizes. This significantly complicates diagnosis. But a specialist will immediately understand what the problem is. Because the symptoms are quite specific. If you press on the manifestation, a slightly whitish liquid will appear.
In some situations, patients complain of itchy skin. However, the risk of bacterial infection should not be excluded. Few people know, but symptoms can appear for several years. The appearance of these bubbles is possible anywhere. But such formations are rare on the palms and soles. Most often, the “abode zone” of the mollusk is the face and neck.
The first sign that should alert you is a small lump on the skin. Then other nodules appear.
In the case of small sizes, they merge into a single seal. It can be 1 cm in size.
Therefore, it is quite difficult not to notice it. Already at this stage, it is important to immediately consult a doctor.
As for general malaise and fever, this is rare.
Interesting fact: apart from its appearance and slight itching, mollusk on the skin does not cause discomfort. Therefore, the child may not be aware of his illness. After the course of therapy there are no scars left on the skin. Only slight depigmentation occurs. In some situations, inflammation of the skin around the nodules occurs. In this regard, the use of antibiotics is relevant.
Diagnostics
The symptoms are quite specific, so once symptoms appear, diagnosis is not difficult. For example, a rash with an umbilical depression and crust-like contents is typical of molluscum contagiosum.
After examining the nodules, a dermatologist can immediately make the correct diagnosis.
Additional examinations are extremely rarely required. To do this, a small amount of skin is taken from the neoplasm. Next, it is studied under a microscope.
Such a biopsy of the biopsy thoroughly shows all the features of the disease. Molluscum contagiosum nodules are often confused with similar formations, which happens with certain diseases.
Among them are the following formations:
- Flat warts. They usually appear on the face or the back of the hands. They are small in diameter and smooth.
- Keratoacanthomas are convex-shaped formations. They are usually hemispherical in shape and slightly reddish in color.
- Milia are small white dots located in the sebaceous glands of the skin. They occur when excessive amounts of dense sebum are produced. It is not completely released from the layers of the skin and the pores begin to clog.
- With scabies, small pink papules appear on the skin.
- Basal cell carcinoma actually resembles a clam on the skin. They are also lightly pearlescent in color and protrude above the surface of the skin. The main difference is the single location. But the “contagious mollusk” appears in plural quantities. Moreover, these rashes are nearby.
But the risk of confusing this disease with warts or lichen ruber is minimal.
Main transmission options
The virus that causes the disease is transmitted from one person to another. Representatives of the animal world are not carriers of orthopoxvirus. There are 3 main infection options:
- Due to sexual intercourse with an already infected person;
- through water;
- contact-household method.
The last case occurs most often. You can become infected through tactile touch (hugs, travel on public transport, massage of a sick subject). This explains why children are often treated for this disease.
The indirect contact route is dangerous because a person cannot be sure that infection will not occur even in the absence of obvious signs (an incubation stage is possible).
You can simply walk into an unfamiliar room, sit on the sofa and become a carrier of the virus. After all, it is wonderfully preserved in various materials. Therefore, it is necessary to carry out thorough disinfection in residential premises and public places.
Another situation is frequent change of sexual partners. In this case, the person takes responsibility for his health. You need to understand that contraception cannot protect against all diseases.
In this case, even a hug will be enough to cause health problems. Although the virus foci are predominantly located in the genitals, so a condom can still protect against infection.
The waterway is often not classified as a separate group. In fact, infection occurs through water, but viral particles enter it from an infected subject. Therefore, many experts are inclined to believe that this is also a household contact route.
A similar outcome of events is possible when visiting swimming pools, saunas and public beaches.
In addition, a person who has previously suffered from molluscum contagiosum may become self-infected again. This happens when the skin rubs. But regardless of the method of infection, the clinical symptoms are very similar.
Some people are immune to this infection.
Recommendations for caring for a child during illness
To avoid spreading the infection to other parts of the body, the following recommendations should be followed:
- Cover the lesions with tiny bandages.
- Wash your hands often.
- Wash clothes in hot water and iron with a hot iron.
- Clean your child's skin with a hydrogen peroxide solution.
Rice. 15. If you have molluscum contagiosum, you should constantly clean and lubricate the skin with antiseptics.