Problem: to the ENT specialist of the Family Dental A.V. A 62-year-old woman came to Arkhandeev with complaints that it was difficult to breathe through her nose, her nose was often stuffy without a runny nose, she snores at night, and she had to constantly use nasal drops to keep her nose breathing. After diagnostics, a diagnosis was made: vasomotor rhinitis.
Solution: vasomotor rhinitis was treated by cauterizing the nasal mucosa using the Celon Elite ESG 200 Olympus device (Japan). Cauterization of the mucous membrane eliminated the cause of nasal congestion, normal nasal breathing was restored, which helped get rid of chronic dependence on vasoconstrictor drops.
What is nosebleed and why is it dangerous?
Nosebleeds are defined as the flow of blood from the nose. It is caused by vascular damage. This pathology occurs in patients of any age and gender. This condition is a clear indicator of trouble in the body. They also appear due to injuries. If they appear, you should immediately contact an ENT doctor.
The causes of nosebleeds are as follows:
- Trauma is a common cause of nasopharyngeal bleeding. They occur during operations on the mucous membrane, diagnostic procedures, and foreign bodies. Pathologies with congestion of the mucous membrane (sinusitis, rhinitis). Dystrophy of the mucous membrane accompanies a deviated nasal septum, as well as atrophic rhinitis. Tumors are benign and malignant.
If this is neglected, repeated episodes occur and the course of the disease, which became the cause of the pathological process, worsens. Nosebleeds have become a major factor in seeking emergency medical care.
The danger of constant nosebleeds is the appearance of iron deficiency anemia. Heavy, repeated bleeding causes a sharp drop in blood pressure. If the lesion involves large vessels, the risk of large blood loss increases. They pose a threat to the patient's life.
Treatment of vasomotor rhinitis
Lack of timely treatment of vasomotor rhinitis can cause serious complications: inflammation of the middle ear, nasal polyps, chronic sinusitis.
Therefore, for the treatment of vasomotor rhinitis, it is very important to contact a good otolaryngologist.
After the initial diagnosis, traditional treatment of vasomotor rhinitis is carried out using a conservative or surgical method. Depending on the degree of development and individual characteristics, the doctor prescribes appropriate treatment.
Methods for coagulation of nasal vessels
Cauterization of blood vessels is considered an effective and low-traumatic method of surgical intervention. It quickly relieves discomfort and restores breathing. Patients easily tolerate this manipulation, quickly recover from surgery and return to normal life.
Instrumental cauterization is carried out using the following methods:
- Laser coagulation. It is considered an effective but expensive technique. The laser beam affects the affected vessels, healthy nearby tissues are not affected. Blood flow in a specific vessel stops. Then it is sealed. Coagulation by radio waves. The vessels are sealed under the influence of current. The electrode is inserted into the nasal passage and the bleeding capillaries are coagulated. The bleeding stops, and a scab forms on the surface of the mucous membrane. Cryodestruction. Here the lesion is treated with liquid nitrogen. It destroys blood vessels, causing blood clots to form in them. Blood circulation stops. Radio knife. This is a thin rod. It doesn't heat up. It cuts tissue and simultaneously cauterizes the edges of the wound. The liquid in the vessels boils and then evaporates. Radio waves. The device produces high frequency radio waves. They quickly evaporate moisture, and then the vessels coagulate.
Mechanical techniques are now rarely used due to their high invasiveness and low effectiveness.
Causes
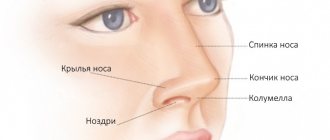
Vasomotor rhinitis primarily affects the inferior turbinates. They humidify and warm the air, but against the background of the disease, this function is disrupted, and the vessels of the mucous membrane do not react correctly to environmental conditions. Constant congestion develops - the main symptom of vasomotor rhinitis. Violation of vascular regulation is associated with an imbalance of the autonomic nervous system, which is responsible for vascular tone.
External and internal factors cause such an imbalance. Environmental conditions include:
- temperature too low or high;
- rapid change in atmospheric pressure;
- air pollution from smoke, substances with a strong odor, the effects of spicy foods, alcohol, nicotine and tar from cigarette smoke, cocaine use;
- respiratory diseases of a viral nature.
Internal factors that can provoke autonomic imbalance:
- stress and strong emotions;
- physical and sexual stress;
- hormonal diseases: ovarian dysfunction (puberty, pregnancy, menstruation), hypothyroidism, excess growth hormone (acromegaly and gigantism);
- pathological reflux (reflux of contents) from the stomach into the esophagus, from the stomach into the pharynx and from the pharynx into the larynx;
- deformation of the nasal septum;
- decreased patency of the upper respiratory tract (adenoids in children).
There may be a hereditary predisposition to the occurrence of the disease.
Rhinitis caused by medications has 2 options. The first of them is associated with long-term use of vasoconstrictor drops, as a result of which vascular receptors lose sensitivity to internal vasoconstrictor factors and chronically dilate.
The second variant of drug-induced vasomotor rhinitis occurs with long-term use of medications that affect the general tone of the autonomic nervous system. These are many drugs for hypertension (ACE inhibitors, alpha and beta blockers, methyldopa, calcium antagonists), antipsychotics, anticonvulsants, oral contraceptives, drugs for regulating potency (sildenafil).
Quite often, rhinitis develops in pregnant women and goes away after childbirth. The reasons for this phenomenon are being studied by doctors. It is believed that hormonal imbalance, stress, and an increase in the volume of blood circulating in the body are important.
Progress of the operation
The intervention is performed under local anesthesia. The patient is operated on in a supine position or seated in a chair.
Cauterization of capillaries is performed as follows:
- Adrenaline is instilled into the nose to constrict blood vessels; a local one is carried out - turundas with a special solution are introduced into the nasal passages and held for a couple of minutes; the surface is disinfected with alcohol; cauterization of vessels is carried out using endoscopic devices; after the intervention, turundas pre-moistened in a hemostatic solution are inserted into the nasal passages.
The procedure lasts up to half an hour and is easily tolerated by patients.
Carrying out laser vaporization.
The doctor sits the patient on a special otolaryngologist chair, puts protective glasses on him and himself, and treats the patient’s skin near the nose with a disinfectant solution. If necessary, the patient’s blood pressure, body temperature, etc. are measured. Next, the doctor numbs the operation site and uses a laser to reduce the size of the inferior turbinates.
Laser vasotomy takes from 20 to 40 minutes, patients tolerate it easily, so after medical supervision they go home on the day of surgery.
Rehabilitation after polypotomy
The postoperative period depends on the extent of surgical intervention performed on the patient. If a polysinusotomy was performed, the patient's nasal cavity is tamponed to avoid postoperative nosebleeds. In the case of endoscopic shaver or laser polypotomy without opening the sinuses, tampons are not needed.
Rehabilitation takes up to one week for any type of intervention.
With minimally invasive interventions, this period is reduced to 2-3 days, until the reactive postoperative swelling of the mucous membrane subsides. After surgery, it is recommended to limit physical activity for 2-3 weeks.
After surgery, topical steroids are prescribed to prevent the regrowth of polypous tissue. Patients with polypous rhinosinusitis should undergo a course of topical steroids several times a year.
Recovery process
The rehabilitation process, as a rule, does not exceed 2 weeks. To accelerate the regeneration of mucosal tissues, it is recommended to use special ointments. You should also carefully remove the crusts that form during the healing process.
To prevent infection of the operated mucosa, the patient should use antiseptic rinsing solutions. Warming the nose, intense physical activity and strong nose blowing are prohibited.
Compliance with medical recommendations will reduce the duration of rehabilitation and minimize the discomfort that accompanies healing.
Symptoms and signs
The main symptom of vasomotor rhinitis is persistent breathing difficulties. Nasal congestion occurs spontaneously. This usually happens in the morning and while lying down. Breathing disorders are accompanied by sneezing, lacrimation, and the release of clear mucus from the mouth. If the disease is accompanied by a bacterial infection, the discharge becomes yellow and green. Body temperature does not increase with vasomotor rhinitis.
The nose may also become stuffy when the patient changes climate or experiences excessive physical activity.
In addition, the clinical picture includes the following main symptoms:
- spasms in the temples,
- redness of the eyeballs,
- heaviness and swelling in the bridge of the nose,
- uncontrolled release of mucus and saliva,
- decreased quality of odor perception,
- redness of the nasal mucosa.
Among the secondary symptoms:
- decreased performance,
- feeling of weakness,
- unstable mental state,
- nervous disorders,
- loss of appetite,
- bitterness in the mouth,
- decreased immunity,
- dyspnea,
- excessive sweating.
Uncontrolled use of drops for vasomotor rhinitis can cause unexpected attacks of itching in the nose. Insufficient ventilation of the lungs entails a disruption of the blood flow process and, as a result, a deterioration in the body’s oxygen supply. This leads to functional disorders of the ANS.
Disease prevention
In order not to wonder in the future about how to cure chronic vasomotor rhinitis, you need to take care of measures to prevent it. To do this you need:
- monitor blood pressure levels;
- do not use harmful chemicals and cosmetics;
- eliminate anomalies in the structure of the nasal cavity;
- eliminate airway obstruction;
- review your diet in favor of healthy foods;
- enrich your menu with minerals, vitamins A and E;
- give up bad habits (alcohol, smoking, drugs);
- stabilize the psycho-emotional state;
- engage in moderate physical therapy;
- avoid infection with viral respiratory diseases;
- normalize the functioning of the immune system.
Regular medical examination helps prevent the development of allergic vasomotor rhinitis. Treatment of symptoms must be agreed with a specialist.
Conservative treatment of nasal polyposis
The first place in conservative treatment is occupied by hormonal drugs: local - topical steroids, and systemic.
Systemic hormonal drugs are used mainly in patients with moderate to severe bronchial asthma. They reduce the intensity and frequency of asthma symptoms, and also counteract the growth of polyposis tissue. Conservative treatment includes mast cell membrane stabilizers and antihistamines. If the polyposis is of an allergic nature or if we are talking about a purulent polyposis process, then antibacterial medications are used. In the case of a fungal process, antifungal agents are prescribed. Conservative treatment methods are indicated for patients with initial and second stages of polyposis or if there are contraindications to surgical treatment. In addition, after surgery, in order to prevent relapse, it is necessary to conduct periodic courses of conservative therapy.
When the disease occurs in children, conservative treatment takes precedence over other methods.
Prices
The specialized private ENT clinic of Dr. Korenchenko (KDK) provides paid medical services both for residents of St. Petersburg and for patients from other cities and regions of the Russian Federation. The clinic employs a team of experienced doctors. Treatment is carried out using the latest medical equipment.
You can make an appointment with KDK specialists in advance by telephone. If you do not have the necessary tests or examination results with you, you can do this at the clinic. The treatment regimen for nasal passage obstruction, including various forms of rhinitis, is selected by the treating ENT doctor.
An effective way to treat vasomotor, drug-induced, and allergic rhinitis is minimally invasive outpatient molecular quantum surgery. The cost of its implementation depends on the volume of surgical intervention, the method of anesthesia (general anesthesia, local anesthesia).
Prices are determined for each specific case individually. The cost of an outpatient operation includes all necessary consumables and medications. The list of medical services and approximate prices are given in the price list in the corresponding section of the website.
Possible complications
With a long course, vasomotor rhinitis can be accompanied by complications:
- constant nasal congestion, causing sleep disturbances and impairing work ability;
- persistent deterioration of sense of smell;
- development of chronic rhinosinusitis, frequent colds;
- formation of polyps or atrophy of the mucous membrane.
Terminology
Selective surgical interventions on the palate include techniques such as surgery, laser plastic surgery, radiofrequency plastic surgery, injection methods and cryoplasty. The above methods are based on the principle of causing trauma to the palate of varying intensity
. During healing, the soft palate usually decreases in volume and thickens. The uvula is partially or completely removed. Thus, snoring can be eliminated or reduced, because the mobility of the structures of the soft palate is reduced.
General anesthesia (anesthesia)
In children under 7 years of age, polypotomy is performed under general anesthesia, so the intervention takes place without pain and, which is especially important for the child, without psychological stress. The clinic uses drugs of a high safety class, they are non-toxic and do not cause complications, so anesthesia is easily tolerated even in childhood and feels similar to normal sleep. Endoscopic polysinusotomy (FESS) and polypotomy, in case of a large volume of intervention, are also performed under anesthesia in children and adults. The type of anesthesia is selected by the operating physician together with the anesthesiologist according to indications.
Responsibilities of doctors
The patient must be warned
that polysomnography or cardiorespiratory monitoring will clarify the diagnosis.
And the patient himself must decide whether he needs additional expenses for a diagnostic study or whether he agrees to surgery on the palate, but without a guarantee that this will help
.
But often no one informs patients about the additional and necessary research, and they take a certain risk without knowing it. Although useless and sometimes dangerous surgical interventions could have been avoided, with proper examination and if an accurate diagnosis of obstructive sleep apnea syndrome (OSA)
. With such a diagnosis, it is impossible to get rid of snoring immediately; this requires time and quite serious treatment methods (you need to lose weight or carry out assisted ventilation during night sleep - CPAP therapy).
Often after ineffective laser uvulopalatoplasty
(LUPP), which did not produce any results, patients are assured that nothing can be done and they are not told about the possibility of CPAP therapy, which is the most effective method for treating severe OSA.
Stages of development of the polyposis process
Stage | Stage I | Stage II | Stage III |
| Size | Covers only the upper part of the nasal septum. | Closes the common nasal passage to the lower border of the middle turbinate. | Covers the entire space. |
| Complaints and signs | The patient is concerned about a decrease in sense of smell or loss of it. Polyps do not interfere with breathing and are discovered by chance. | Polyps are visible during endoscopy or rhinoscopy. The patient is concerned about slight difficulty breathing through the nose and mucous discharge from the nose. | The patient stops breathing normally, vasoconstrictor drops do not help him, and a nasal sound develops. |
Cauterization methods
Cauterization of vessels in the nose occurs using the following basic techniques:
- thermocoagulation;
- radio wave coagulation;
- laser conchotomy;
- chemical cauterization;
- cryodestruction;
- ultrasonic disintegration.
More information about cauterization methods:
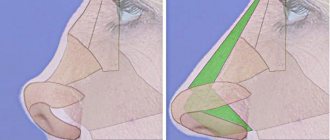
- Thermocoagulation, which can also be called electrocoagulation, is performed using an electric current. A heated electrode is inserted into the mucosal tissue, burning out excess tissue. Subsequently, the treated mucosa heals, and the volume of the shell decreases.
- Radio wave coagulation - the name of the method speaks for itself. Cauterization here is performed using a probe that transmits a radio wave. The wire itself does not heat up, but the current carried through it heats the cells, which leads to their destruction. As a result, the volume of excess tissue and the shell are reduced in volume. This method is characterized by good tolerability, since the effect of the current is not accompanied by a painful effect, and after the procedure, swelling and inflammation are minimal.
- Laser cauterization of vessels in the nose or conchotomy involves exposing the tissue to a beam of light with a certain power. The laser acts in a targeted manner, so the surrounding tissue around the damaged area is not affected. The laser removes hypertrophied mucosal tissue and forms a coagulation film. The latter eliminates infection and further bleeding. Pain and swelling are also reduced.
- Chemical cauterization is usually called, in a simplified formulation, cauterization with silver, since this procedure uses a solution of silver nitrate in a concentration of about 50%. This is a more gentle procedure, which is performed by applying cotton swabs soaked in a special solution to the mucous membrane. The bactericidal effect of silver nitrate is due to a significant change in the properties of the protein (denaturation). The result is the formation of a crust in the nasal cavity, which goes away on its own over the next few days. The use of silver nitrate must be done extremely carefully so that the solution does not come into contact with the patient’s skin.
- Cryodestruction - this cauterization method involves exposure to low temperatures that are transmitted through a cryoprobe. Here, bleeding and thrombosis occur, and the hypertrophied mucosal tissue is destroyed. As a result, the volume of the nasal concha decreases. Sometimes a scheduled repetition of the procedure is required. A few days after cryodestruction, a mucous secretion emanates from the cavity as a spontaneous cleansing.
- Ultrasonic disintegration is done using an ultrasonic waveguide to restore blood supply in the pathologically enlarged tissues of the nasal mucosa. It is characterized as a gentle procedure. The consequence of this effect is reduction of the mucous membrane and normalization of breathing.
Based on the existing symptoms, as well as the age of the patient (the procedure can be performed even on a child), the appropriate technique is selected. During these procedures, safety precautions must be observed. The patient is prohibited from moving his head and talking without the doctor's permission.
Rules for physiotherapy and surgery for various diseases
Laser treatment is carried out in any hospital, hospital or clinic. Laser removal of adenoids and polyps is carried out more often in hospitals or clinics. Treatment is carried out by an otolaryngologist. Laser therapy using low-intensity radiation is carried out in clinics or paid clinics.
Before treatment, the patient must be examined. The doctor (otolaryngologist) collects a complete medical history and conducts an examination. If a child or adult has concomitant diseases, the patient is referred for consultation to other specialists and a pediatrician (general practitioner). Laser treatment does not begin until all necessary examinations have been completed.
Laser treatment cannot be performed at home, since increasing the duration of one physical procedure or the entire course of treatment can negatively affect the course of the disease.
Treatment of runny nose with laser
A runny nose can be acute or chronic (vasomotor, allergic). Treatment for each type of rhinitis is slightly different. Acute rhinitis is manifested by severe inflammation of the mucous membrane. In case of a runny nose, the nasal area and the mucous membranes of the nasal passages are irradiated directly using endonasal attachments. The mucous membrane can be irradiated without inserting a nozzle into the nasal cavity (at the entrance to the nostril). In case of severe inflammation, insertion of the nozzle into the nasal passage is allowed.
Irradiation of the nasal area is carried out during the first 3 days of therapy. The duration of one session lasts 1 minute. You can also work on the collarbone area. The duration of irradiation of this zone is 1.5-2 minutes.
If endonasal irradiation is performed, the nose is rinsed with saline before the procedure to free the nasal passages as much as possible. The duration of one physiotherapy procedure can be up to 4 minutes (this includes all types of irradiation: on the nose, on the collarbone, endonasal exposure). Course therapy is equal to 6-8 physiotherapy procedures. During treatment, swelling of the mucous membrane, redness goes away, and nasal breathing improves.
Vasomotor rhinitis is treated in a similar way. Irradiation is carried out endonasally, on the area of the collarbone and nose. The maximum duration of one physiotherapy procedure should be 4 minutes. Course therapy is equal to 2-4 physiotherapy procedures. Courses of treatment are carried out in spring and autumn.
Seasonal allergic rhinitis is treated in the same way as other types of rhinitis. Therapy begins 3 weeks before the upcoming exacerbation (spring, autumn). The course of therapy consists of 4 physiotherapy procedures. The effectiveness of treatment is quite high. After the first procedure the patient feels significantly better. Laser therapy can prevent the appearance of a mild seasonal runny nose.
Sinusitis and frontal sinusitis, treatment tactics
Nasal discharge can cause sinusitis and sinusitis. Sinusitis is an inflammation of the maxillary sinuses. Frontitis is inflammation of the frontal sinus. Treatment is often carried out using a therapeutic laser.
The patient is irradiated in the forehead or paranasal area (right and left of the nose). The duration of the procedure is 4 minutes. Course therapy consists of 6-9 sessions. Before irradiation, be sure to rinse the sinuses and remove the pus. Treatment can be repeated after 2-3-6 months, depending on the clinical manifestations.
Physiotherapy can reduce pain, reduce inflammation and redness of the sinus mucosa.
After a course of therapy, discharge from the nasal passages decreases or stops in patients. After several courses of treatment, relapses of the disease become much less frequent.
Therapy for grade 2-3 adenoids
Adenoids are more often observed in children under 14 years of age. Many children have this disease during childhood. More often, adenoid vegetations develop due to a weakness of the immune system. The cause of the appearance of adenoids is severe respiratory and other infections: measles, scarlet fever, chickenpox.
After the disease, adenoid vegetations begin to increase in size and block the passage of the nasopharynx. This is manifested by impaired nasal breathing. The child has an adenoid face: the mouth is constantly open, breathing is impaired. The patient's brain constantly experiences hypoxia due to lack of oxygen. This leads to developmental delays, difficulty remembering, and memory impairment.
Laser therapy for adenoids is carried out every day. Irradiation is done endonasally. Laser exposure is carried out in each nasal passage for 1 minute. The area of the front teeth is also irradiated (the mouth is open) for 1 minute. Course therapy is carried out after 2-3 months (2nd course) and 6 months (3rd course).
During therapy, the nasopharyngeal mucosa is restored, hyperemia (redness) goes away.
Irradiation helps fight microorganisms. Adenoid vegetations decrease in size, which improves nasal breathing.
If treatment is ineffective, the patient's adenoids are removed by laser surgery. The laser is inserted into the nasopharynx. After removal of the adenoids, the patient recovers quickly, and nasal congestion is completely relieved.
Features of treatment in children
Polyps are more common in adults than in children. But in childhood, as with any chronic pathology, doctors show a minimum of radicalism in relation to treatment; surgical treatment takes a back seat. And if surgical intervention is still required, it will be minimally invasive. If the child is under 15 years old and polypotomy is indicated for him, it will be gentle - with a laser, radio waves, endoscope or shaver, without opening the paranasal sinuses.
Children are treated conservatively; treatment, in addition to the prescription of local and general medications, includes rinsing the nasal cavity using the displacement method. During the rinsing process, allergens and bacteria from the nasal cavity and paranasal sinuses are washed away, and inflammation is reduced.
Can promises be trusted?
There are medical centers that encourage palate surgery to cure snoring. But at the same time they do not carry out preliminary diagnostics.
, for example, polysomnography or other studies that can diagnose sleep apnea.
Most operations for snoring on the palate are carried out without a preliminary full examination of the patient’s breathing during sleep. Sometimes you can hear that they treat sleep apnea, although this is absolutely contrary to international standards
. Surgery for snoring on the palate without research may at best be simply ineffective, but sometimes it can lead to tragic complications.
In Israel, for example, all ENT centers are required to first fully examine the patient’s nighttime sleep, and only after that decide on the possibility of surgery. Studies are also carried out after laser treatment for snoring. Unfortunately, in our country, standards of this kind have not yet been adopted at the state level, but every otorhinolaryngologist must responsibly
treat your patients. He needs to independently decide whether it is advisable to treat snoring and sleep apnea with laser or radiofrequency. Each specialist must be based on knowledge, clinical experience and remember the main thing - “Do no harm!”
Many centers that provide laser and radiofrequency treatment for snoring do not purchase diagnostic equipment for polysomnography because it is quite expensive. The studies themselves are quite labor-intensive, and therefore many centers take risks and do not conduct the study
, but rely only on the story of the patient, his relatives and on the clinical examination, which is carried out during the day. Therefore, diagnostic errors are often made. Sometimes patients themselves may refuse polysomnography in order to save money.
The attitude of specialists towards selective interventions on the pharynx
Sometimes advertisements present laser treatment as the most effective treatment for snoring. And it seems that curing snoring is quite quick and simple. But in reality, the solution to the problem of snoring is not so obvious. We are often approached by patients who continue to snore, despite the fact that they previously treated snoring with laser and radiofrequency, which turned out to be ineffective.
Foreign experts are critical of selective interventions on the pharynx in patients with snoring and sleep apnea:
- There is low or no effectiveness of laser treatment for OSA [Arch. Otolaryngol. Head Neck Surgery, 1997]
- LUPP may be accompanied by pain. There are no significant differences in postoperative pain between LUPP and uvulopalatopharyngoplasty [J. Otolaryngol., 1997].
- LUPP can lead to various complications. Sometimes LUPP provokes the development of OSA in patients with uncomplicated snoring or aggravates existing OSA. [Am. J. Resp. Crit. Care Med., 1997].
Diagnostics
THE INSTITUTE OF ALLERGOLOGY AND CLINICAL IMMUNOLOGY has a fundamental base that allows it to carry out the full range of diagnostic and therapeutic measures for any form of allergy that meets the level of international standards. Many of the diagnostic and treatment methods were developed by the staff of our Institute.
Diagnostic measures are based on anamnesis, clinical picture and laboratory diagnostics.
- Anterior and posterior rhinoscopy
- Bacteriological study for aerobic and facultative anaerobic microorganisms
- Diagnostic measures aimed at identifying the allergen that causes the disease
- Determination of the sensitivity of microorganisms to antibiotics and other drugs
- Detailed general (clinical) blood test, clinical urine test.
- Cytological examination of the nasal mucosa according to indications
- Biochemical blood test according to indications
Kinds
The classification of vasomotor rhinitis is based on its causes and mechanisms of development. The following types of disease are distinguished:
- medicinal (caused by decongestants or oral medications);
- hormonal (during pregnancy, puberty, diseases of the endocrine system);
- reflex (food, cold and others);
- psychogenic (associated with emotional stress);
- idiopathic (unexplained nature);
- mixed.