It is worth talking about some indications for tissue coagulation in more detail, since the incidence rate is growing, and this method sometimes becomes a priority in the treatment of pathology. Cervical erosion is a structural change in the uterine mucosa. It can be present in a woman’s body under normal conditions, or it can reach enormous sizes after childbirth or surgery, which requires minimally invasive surgical intervention. If the patient refuses coagulation, then consequences such as cervicitis and cervical cancer appear. Papillomatosis is multiple formation of papillomas on the surface of the epithelium or mucous membrane of organs. In the initial stages it has a benign course. Without surgery, it tends to malignize, that is, it turns into a malignant tumor. Hemorrhoids are dilation of veins, the formation of hemorrhoids within the tissues of the rectum. Significantly reduces the quality of life, accompanied by itching, pain, bleeding and other symptoms. At the third or fourth stage, surgery in the form of laser coagulation is required, as the risk of thrombosis and necrosis increases.
Causes of coagulation
If we consider coagulation as the natural ability of blood to close wounds and prevent infection, then the mechanism of development here is as follows:
- disruption of tissue structure, the appearance of a wound becomes a trigger for subsequent chemical reactions;
- platelets, together with blood clotting factors, attach to the affected area, fibrin is produced;
- this fibrin is a thread intertwined with each other, which will ultimately become a framework for the resulting blood clot;
- an increasing number of platelets are attracted, the hemocoagulation process is suspended when the thrombotic mass completely prevents further bleeding.
Physical and chemical coagulation follows a completely different path. With the help of a laser and biochemically active substances, protein synthesis is disrupted at the cellular level, cells die in unusual conditions and cover the area of influence with a kind of crust consisting of dead tissue. If we are talking about capillaries, small vessels that undergo coagulation, then they simply curl up and stop functioning. Next, the human immune system is primarily involved, producing large numbers of macrophages, leukocytes, that is, cells with phagocytosis - the ability to break down and absorb foreign solid particles. All dead cells are broken down, and new healthy tissue is formed that is capable of performing its own functions.
Use in surgery
Coagulation began to be used in surgery relatively recently. It is used to “seal” bleeding vessels, remove malignant or benign tumors, and perform operations that require special precision and care.
- electrosurgical (contact and non-contact);
- thermal stapler;
- argon plasma;
- laser.
The electrosurgical method is performed using a charged scalpel in the shape of a ball, a loop needle. The instrument can be used to perform local dissection of the membranes in a small area. Moreover, all manipulations can be performed with minimal access to the organ, which avoids complications in the form of secondary infectious inflammation. Most often used for bleeding from erosions or ulcers located in the organs of the gastrointestinal tract. Using a thermal stapler, vessels are also sealed during surgery, and tissue incision is less traumatic. The advantage of this method is a clean surgical field, that is, the entire view is not obscured by leaked blood, a short tissue healing time, and a lower risk of complications. Used for laparoscopy, prostatectomy, hysterectomy.
Complications
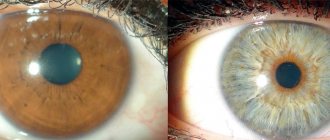
- Visual field defects - an incorrectly configured laser device can damage not only the target arteries, but also nerve fibers. A person begins to look as if through binoculars or a pipe.
- Allergic reaction. If there is a tendency to hypersensitivity, if there is an individual intolerance to electrical procedures, a person becomes covered with a rash, red spots, and dermatitis may develop.
- Suppuration of the affected area. If the skin or mucous membranes are not properly cared for after laser coagulation, active inflammation forms, first serous and then purulent exudate appears.
- Bleeding. If the rules of coagulation are violated, primary or recurrent bleeding may occur from a vessel at the bottom of the ulcer or the area where there was a neoplasm.
- Sanitation of the vagina using antifungal agents.
- Prevention of bleeding using special medications.
During the preparation process, it is important to take precautions that will increase the success of the procedure and reduce the risk of complications during the recovery period. Precautions include:
- Checking blood clotting function to prevent serious complications.
- X-ray examination of the lungs.
- Diagnosis of HIV infection, which leads to a significant decrease in immunity and will aggravate the postoperative process.
- Diagnosis of sexually transmitted infections and their mandatory treatment.
- Identification of oncogenic tissues that require a separate treatment method (taking a smear for oncocytology).
Preparing for surgery
No special preparation is required for this procedure.
All you need is standard research data:
- general blood analysis;
- markers of hepatitis C and B;
- fluorography;
- blood test for RW;
- blood test for HIV.
In some cases, tests for blood clotting and bleeding time (Duke's test) may be necessary. This will make it possible to more accurately determine the presence/absence of dysfunctions of vascular-platelet and coagulation hemostasis.
Persons 40 years of age or older must also provide ECG readings and a statement from a physician. Before the intervention, it is also necessary to shave the operated area.
The surgeon then marks the veins according to the data obtained during the examination of the problem area.
Methodology for performing various types of procedures
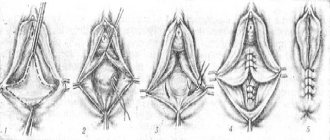
Today, there are several types of cervical coagulation. They differ in the method of influencing the pathological focus. We will consider the most popular treatment methods below.
Diathermocoagulation with electric current
This type of influence is carried out using alternating current and a special loop (conductor). In this case, the pathological focus is cauterized and destroyed with the formation of a dense scab, which subsequently disappears. Electrocoagulation is carried out using two electrodes. Depending on the lesion, various loops are used that conduct electric current to the tissues.
Radio wave coagulation
The procedure involves exposing the altered area of the cervix to high-frequency radio waves. Unlike the previous option, the beam directed at the defect displaces it, acting in a targeted manner. This type of coagulation is based on exposure to high temperatures, which lead to the evaporation of the pathological focus without affecting healthy tissue.
Radio wave treatment of the cervix is carried out using a special device
Argon plasma method
Argon plasma coagulation is one of the modern and advanced methods of treating gynecological diseases. During the procedure, the affected tissue is exposed to a radio wave, which is amplified by ionized gas - argon. When exposed to a powerful radio wave, the affected area heats up and coagulates.
Laser beam vaporization and laser destruction
The first method is based on evaporation of the pathologically changed area using the targeted action of a laser beam. In this case, the wound heals quickly and there are no negative consequences. The second method is based on a deeper impact of a laser beam, which dehydrates the affected tissue. As a result, after the intervention, not even a trace remains on the cervix.
Chemical cauterization
Treatment involves influencing the pathological area using a special concentrated composition. It is applied to the cervix, causing a chemical burn to the affected area followed by the formation of a scab. Cauterization is the least effective coagulation method.
Cryocoagulation
Hypothermia of the cervical defect is performed using liquid nitrogen. If almost all previous methods were based on high temperature exposure, then this method, on the contrary, freezes the pathological focus to healthy tissue.
New life for your feet
After the operation has taken place, a period of recovery has passed and all traces of EVLT have disappeared (i.e., after a fairly short period of time), the patient’s legs, and this especially applies to female patients, regain the beauty of their legs. Peace of mind comes and anxiety about the appearance of your beautiful legs disappears. You no longer need to limit yourself in choosing your wardrobe. But with all this, you should not forget and ignore the doctor’s recommendations. It is necessary to undergo examination by a phlebologist, according to his prescription. And you need to get into the habit of strengthening blood vessels, not doing it regularly, but constantly. The body needs your help. Reliable modern technologies, the professionalism and experience of our doctors and your active desire to get rid of the disease will not give varicose veins the slightest chance to develop!
Remember the main advantages of EVLT over other methods:
- The operation is performed on an outpatient basis or discharged on the day of surgery, the duration of the operation is 30-40 minutes
- Cosmetic effect. No skin wounds or stitches
- Less traumatic manipulation
- No anesthesia required. The operation is performed under local anesthesia
- Return to work is possible the next day after surgery
Laser coagulation
This type of coagulation using electromagnetic radiation is used in the treatment of diseases such as:
- Varicose veins;
- cervical erosion;
- the presence of pigment spots;
- external hemorrhoids;
- rosacea;
- retinal dystrophy, tendency to detachment;
- formation of hemangiomas.
It has gained particular popularity due to its minimal point impact, which allows healthy nearby tissues to be preserved. Laser coagulation allows you to prevent complete loss of vision due to retinal detachment, and restore the beauty of the skin of the lower extremities and face, as clearly visible vessels are removed.
- Cataract is a clouding of the lens that cannot transmit laser beams to the deeper parts of the eye;
- Severe hemorrhages in the retinal area - it is not possible to direct the rays precisely to the required area;
- Thrombophilia is an increased tendency to form blood clots. After the procedure, there is a high risk of blockage of blood vessels with thrombotic masses, which will dramatically disrupt the delivery of oxygen and nutrients to the tissues;
- Infectious diseases. Pathogenic microflora after laser correction can either contaminate the affected area or cause an inflammatory reaction in the periphery.
Contraindications
Vascular coagulation is well tolerated by patients, but the procedure has its contraindications. These include:
- changes in the skin of an atherosclerotic nature;
- narrowing of the arterial lumen of the veins;
- inflammatory process on the skin of various etiologies;
- open wounds on the body in the treatment area;
- cardiac ischemia;
- thrombophlebitis;
- tendency to form keloid scars;
- AIDS virus;
- carrying out cosmetic procedures less than 2 weeks before coagulation;
- the patient has epilepsy and other mental disorders;
- serious pathologies of the heart and blood vessels.
Before performing the procedure, the doctor must determine whether there are contraindications
When performing coagulation of blood vessels on the cheeks and wings of the nose, the doctor must take into account such contraindications as a large number of red moles, oncological tumors, a fresh tan, recent peeling or facial cleansing.
Important! If, in the presence of these conditions, some salon still agreed to provide you with treatment, it is better to look for another doctor. This procedure may be unsafe for your health.
Mechanism of coagulation in surgery
At its core, argon plasma coagulation is an electrosurgical, monopolar, non-contact method of influencing biological tissues with high-frequency current using ionized and, as a consequence, electrically conductive argon - argon plasma. Argon gas, which is inert under normal conditions, is ionized under the influence of an electric field generated between the tip of the electrode located at the distal end of the applicator probe and the adjacent tissues. The resulting jet of argon plasma, regardless of the direction of the flow of argon itself, is automatically directed to those areas of the tissue surface that have the lowest electrical resistance and has a coagulating effect on them (Bagt O. et al., 1994). Rapid coagulation of a large surface occurs, creating a thin layer (up to 3 mm) of a reliable scab. When operating an argon plasma coagulator, the temperature on the tissue never exceeds 110° due to the cooling effect of argon. Once a scab has formed, no further penetration of energy into the tissue occurs. The depth of its penetration into the tissue is approximately 2 times less than with traditional coagulation, which significantly reduces the risk of perforation of thin-walled organs and allows the use of argon plasma coagulation in the duodenum and colon, as well as in the esophagus. Since argon does not support combustion, there is less charring of the fabric, and there is virtually no smoke.
Coagulation in medicine and cosmetology
Modern medicine uses coagulation to treat certain vascular diseases. With its help, you can get rid of spider veins on the face and body, as well as solve more serious problems. The darkening of some vessels, noticeable under the skin, is dead capillaries that have long lost their original functions. It is no longer possible to cure them, but it is very possible to get rid of them forever. Using a laser, the doctor exerts a targeted effect on the damaged vessel, causing a coagulation reaction in it. After some time, the vessel sticks together and resolves. The cosmetic defect disappears. In addition to spider veins and unsightly blue webs on the legs, coagulation can help you get rid of warts, moles and papillomas.
Video on spider vein removal sclerotherapy
Treatment results for our patients
Disease: varicose veins
Treatment method: EVLT + MINIFLEBECTOMY
Combined treatment of varicose veins. Endovasal laser obliteration of the vein on the left leg (EVL) + Miniphlebectomy
Disease: varicose veins
Treatment method: EVLT + MINIFLEBECTOMY
Laser treatment (EVLT) followed by miniphlebectomy of the tributaries of the great saphenous vein on the thigh and shin of the right leg. Miniphlebectomy of varicose veins.
Disease: Telangiectasia
Treatment method: Foam sclerotherapy
To remove the stars, the patient underwent a session of microfoam sclerotherapy (Foam-Form) of the reticular veins under the control of laser transillumination.
Disease: varicose veins
Treatment method: EVLT + MINIFLEBECTOMY
Upon examination of the patient, varicose veins were diagnosed on the right leg. Combined treatment with EVLT + miniphlebectomy was performed.
| Fill out an application on the website, we will contact you shortly. Or call us at +7(495) 967-94-42 |