Postoperative complications develop in at least 10% of all operations. There are several reasons for this.
Firstly, the situation that made surgical intervention necessary does not disappear at the time of surgery. The patient will have a long time to restore normal functioning of the body.
Secondly, surgical intervention itself is a non-physiological effect that disrupts many cyclic processes in the body. This includes the introduction of a narcotic substance that loads the liver and kidneys, and a change in heart and respiratory rhythm, blood loss, and pain. Emergency and long-term operations are natural factors for the occurrence of complications. Normally, on the 3-4th day the body copes with unexpected circumstances, and the patient’s well-being improves.
Treatment of postoperative complications requires a qualified approach on the part of doctors and medical personnel.
Chapter 6. The main causes of the development of ANFH and symptoms of diseases associated with it
Volkov E.E., Keqin Huang Aseptic necrosis of the femoral head.
Non-surgical treatment / Transl. from Chinese V.F. Shchichko. - M., 2010. - 128 p.: ill. ISBN 978-5-9994-0090-1 UDC 616.7 © Volkov E.E., Keqin Huang, 2010 © HuangDi 黄帝
The most common causes of ANFH are alcohol intoxication, smoking and excessive use of glucocorticoids.
6.1. Necrosis of the femoral head caused by alcohol intoxication
6.2. Necrosis of the femoral head associated with smoking
6.3. Necrosis of the femoral head caused by glucocorticoids
6.4. Osteoporosis
6.5. Congenital varus position of the femoral neck
6.6. lupus erythematosus
6.7. Metabolic bone diseases
6.8. Neurotrophic diseases of bones and joints
6.9. Hyperparathyroidism
Risk of developing avascular necrosis due to trauma
One of the main reasons for the development of ANFH is fractures of the head or neck of the femur. The greatest risk is a transepiphyseal fracture (impaired blood supply to the proximal fragment up to 97.6%), subepiphyseal fracture (impaired blood supply to the proximal parts of the head up to 97.4%), subcapital fracture (impaired blood supply up to 92%).
There are several types of fractures:
Type 1: abduction, subcapital, incomplete fracture without displacement. It occurs due to the action of diverting tension. During a fracture, the neck and diaphysis of the femur are directed towards the head. The bone fragments are firmly wedged, and the fracture surface line is close to horizontal. The disturbance of blood supply is minimal (up to 10.2%). The prognosis for recovery is good.
From left to right: subcapital, transcervical, basicervical fractures.
Type 2: adduction, subcapital, complete fracture without displacement. The fracture is located in a vertical plane, passing through the femoral neck. Trabeculae and lower cortex are torn, without displacement. Microcirculation is impaired by 23.6%. The prognosis is favorable.
Type 3: adduction fracture with incomplete displacement of bone structures. It is characterized by varus deformity of the femoral neck, but the fragments remain connected due to the posteroinferior block. The distal bone fragment is in a position of external rotation and abduction with an angle open anteriorly. There is a comminuted fracture of the posterior surface of the neck. The trabeculae and lower cortex are torn. Vascularization disorders reach 42.8%. Risk of developing avascular necrosis.
Type 4: adduction fracture with complete displacement. The head is deprived of all connections with the synovial membrane of the capsule, as a result of which the fragment becomes free. The disturbance of blood supply is maximum (54.4%). The risk of aseptic necrosis is increased.
To summarize: in the event of a potential injury to the hip joint, you must go to the nearest emergency room and have an x-ray taken. Early diagnosis can save the joint from destruction and maintain a high quality of life!
Minimally invasive endoprosthetics in the Czech Republic: doctors, rehabilitation, terms and prices.
Find out more
6.1. Necrosis of the femoral head caused by alcohol intoxication
In a certain proportion of patients with aseptic necrosis of the femoral head (AFH), this disease arose due to long-term chronic alcohol intoxication.
The effect of alcohol on the development of ANFH is described in detail using the following experiment. Groups of animals with simulated necrosis of the femoral head were compared: a group given strong alcoholic drinks (over 50°C) and a control group.
Radiology, computer and electron microscope image processing, serology and histology were used to monitor changes. The results of the experiments confirmed that in the group of animals with simulated ANFH, which were given strong alcoholic drinks, disorders of fat metabolism, serious damage to cell membranes, fibrous atherosclerosis in arterioles and a large number of fat drops in cell lacunae, twisting of capillaries, their thinning, blockage and ischemia. Due to the toxic effect of lipid peroxides and alcohol, as well as metabolic products, damage to bone cells and their fatty degeneration occurred, as well as necrosis and rupture of trabeculae, and the number of lacunae in the bone cavities increased. Excessive alcohol consumption leads to an increase in the number of fat droplets in the peripheral circulation and their transformation into fat globules, resulting in embolism and necrosis in the subchondral capillaries of the femoral head.
During the experiment, it was established that the amount of fatty substances increased in the bone marrow cavities, and in the subchondral cells of the head of the femur, sedimentation of fat-like substances occurred, the bone structure collapsed, the trabeculae became loose and disordered, and the skeleton was lost. Experimental results indicate that chronic alcohol intoxication can lead to ANFH, as well as to a number of pathological changes in the histology, biomechanics, physics and biochemistry of bone, as a result of which the structure of the femoral head is destroyed and bone cells die, capillary infarction and strangulation obstruction occur. .
In addition, it was found that in 53.2% of people who drink alcohol for a long time, excess fat accumulates in the liver (since alcohol disrupts fat metabolism), causing fat embolism and blockage of blood vessels, which leads to obliteration of the blood microcirculation system in the bones . The effect of alcohol promotes osteoporosis, dulls the transmission of sensations from the nerve-fibrous bundles of the hip joint, weakens the pain threshold, reduces the degree of physiological reaction, which leads to static and dynamic overloads and the occurrence of necrosis of the femoral head.
The fact that chronic alcohol intoxication can cause necrosis of the femoral head has already attracted the attention of practicing physicians. A large number of clinical cases also confirm this conclusion, and if a patient with ANFH continues to drink alcohol during treatment, this negatively affects the results of treatment.
Foreign scientists Cold and Cageni, having examined 790 patients who abused alcohol, found that on radiographs of 1580 femoral heads, 260 of them showed destruction of their structure, collapse and necrosis. Japanese scientists, having examined 1098 alcohol drinkers, found that 60% of patients who drank more than 0.54 liters of alcohol daily had aseptic necrosis of the femoral head. A sample from the authors' clinical statistics showed that out of 1507 patients with ANFH, 927 were addicted to alcohol. The results of functional studies confirmed the fact that chronic alcohol intoxication contributes to the occurrence of ANFH, which made it possible to find new ways to prevention and treatment.
Treatment of dry necrosis
There are two ways to stop the destruction of cells in tissues:
- surgical intervention;
- apply local treatment.
Local treatment, the most gentle, consists of the following measures: treating the area around the affected area with an antiseptic; applying a bandage soaked in ethyl alcohol or other disinfectant (boric acid, chlorhexidine), etc. But it is not always possible to do without the intervention of surgeons, since necrosis is a rather complex disease. Conservative therapy can improve blood circulation in the affected area (intimothrombectomy, bypass surgery). It is not recommended to treat this disease on your own. It is best to contact a specialist who will prescribe treatment. The process of stopping tissue cell death is quite complex. To achieve restoration of the body, it is necessary to take radical measures. In such cases, the work is carried out by several doctors specializing in different fields of medicine. The results of treatment may depend on several factors, including the location of the lesion, the size of the area with necrosis and the general condition of the patient. Tissue destruction can have a toxic effect on the patient’s body due to the emergence of microbes in the affected area. That is why the first actions are aimed at disinfecting this area. Experts recommend visiting doctors as often as possible to check the condition of your body. Such procedures can help identify the disease at the primary stage, which will significantly facilitate further treatment.
6.2. Necrosis of the femoral head associated with smoking
According to statistics, today approximately 4 million people die annually from diseases caused by smoking. More than 30% of patients with ANFH are smokers, and many of them have poor health. By 2022, the number of people killed by smoking will exceed the number of people killed by any other disease, including AIDS. Smoking will become the most important epidemic disease in the 21st century.
When tobacco burns, it releases more than 4,000 toxic substances, of which, as is now known, more than 40 are carcinogenic. Smoking is the main cause of cardiovascular and cerebrovascular diseases. The incidence of lung cancer in smokers is 20 times higher than in non-smokers. One of the research centers in the USA, working on this problem for 35 years, confirmed that there is a clear connection between smoking and cancer: for those who smoke more than 1 cigarette per day, the risk of cancer immediately increases by 2 times , and for those who smoke more than one pack of cigarettes, the risk of getting cancer increases 20 times. Smokers easily get stomach and duodenal ulcers, as well as neurasthenia.
Active and passive smokers - patients with necrosis of the femoral head - poison themselves with nicotine and lead, which accumulate in the body and impair blood circulation, destroy the bone structure and aggravate necrosis of the femoral head. After smoking, nicotine quickly enters the bloodstream and irritates the sympathetic nerve and chromaffin cells, stimulates the production of active factors by the adrenal glands, causing an increase in angiotensin and vasoactive elements in the blood plasma. In different tissues, the quantitative distribution of α- and β-receptors is different, which contributes to the contraction of peripheral blood vessels in tissues and dilation of central vessels, spasm of arterioles, increased vascular resistance, impaired venous outflow, increased blood viscosity, preventing microcirculation in the head of the femur, as a result bone tissue stops receiving nutrition and the destruction of the bone structure of the femoral head accelerates.
Thus, smoking patients aggravate the course of ANFH, slowing down the recovery of health. The harm caused by smokers to society What is even more dangerous is that the smoke exhaled by smokers causes even more harm to others than to the smokers themselves. Research conducted by scientists has confirmed that in Shanghai, 37.8% of school-age children have blood lead levels above the permissible level. For every 100 mg increase in the level of lead in the blood of children, the mental development index decreases by 6-8 points, and the main cause of lead poisoning in children is second-hand smoke created by parents at home. In this regard, to preserve the health of children and other people, it is necessary to create a smoke-free environment in society.
Actively and passively smoking women, in addition to harming themselves, they also destroy their offspring, since smoking has a bad effect on the psychosomatic development of the fetus and causes serious damage to the intellectual abilities of children. If a nursing mother has nicotine in her milk, this has a negative effect on the baby's health. The authors hope that every patient with ANFH will show high social consciousness: will stay away from cigarettes and value the health of their loved ones and other people.
Treatment
For each stage according to ARCO, the duration of each of them is determined. For stage I and stage II - up to 6 months, stage III - 3-6 months and an immediate transition to stage IV.
Early initiation of treatment, while symptoms reveal only minor discomfort in the periarticular area with irradiation to the groin area and knee joint, is extremely important.
Tasks during the treatment period:
- For patients with a history of trauma, intoxication, and those at risk (taking glucocorticoids, cytostatics), use the diagnostic algorithm for ANFH in the early stages. It includes early clinical manifestations, information analysis of cardiac signals using the Screenfax system, MRI/CT, radiography, laboratory tests of markers of bone metabolism, scintigraphy, X-ray/ultrasound densitometry.
- Using a non-surgical treatment method, improve metabolic processes in the lesion, regenerate the elements of the femur and restore the function of the joint itself.
Taking into account the fact that ANFH is a multifactorial pathology, it is necessary to use an integrated approach in diagnosis, treatment and rehabilitation aimed at restoring:
- optimal functioning of all systems and organs;
- microvasculature and hemocoagulation parameters;
- neuroregulatory factors;
- immune reactions;
- myodiscoordinate processes and biomechanics of joints.
Treatment of stages 1-2
Seems most effective for a favorable prognosis. The most important condition for successful treatment is strict adherence to the regimen. You should give up bad habits (alcohol and smoking), avoid overloading and hypothermia of the affected joint.
Therapy is directed in several areas: medication, physiotherapy and exercise therapy.
Drugs . For aseptic necrosis, the following groups of drugs are prescribed:
- Bone resorption inhibitors (bisphosphonates). They slow down the destruction of bone tissue and prevent compression and deformation of the femoral head.
- Calcium and vitamin D preparations. In the form of active forms, they facilitate the formation of bone structures and their mineralization. The dose is selected individually.
- Additional sources of minerals and phosphates (ossein-hydroxyapatite).
- Since blood coagulation factors change in ANFH, antiplatelet drugs (chimes, dipyridamole, xanthinol) are necessarily prescribed.
- Non-steroidal anti-inflammatory drugs (NSAIDs). They have an analgesic and anti-inflammatory effect. The most commonly prescribed drugs are ibuprofen, ketoprofen, diclofenac and their analogues.
- Muscle relaxants to relieve muscle tension around the joint.
- Multivitamin complexes, chondroprotectors.
Physiotherapy. The main task is to stimulate blood flow in tissues and start/accelerate regenerative processes.
- a) hyperbaric oxygenation. The patient is placed in a pressure chamber, where he is exposed to air enriched with oxygen under conditions of high pressure. This procedure improves oxygen supply to the damaged area.
- b) shock wave therapy (SWT). Represents the action of a sound wave. It is carried out pointwise, certainly at the site of damage. It effectively affects pathological tissues that interfere with the healing of diseased joints (calcium crystals or adhesions). UVT improves blood supply to the treated area and thereby enhances the reparative effect.
- c) myostimulation. Allows you to restore muscle tone during developing hypotrophy, which is often found in ANFH. Stimulation relieves spasm of the muscle fibers surrounding the joint and accelerates local blood flow.
Physiotherapy
The initial stage is unloading the affected joint. In this case, the patient is fitted with crutches, which can take up to a year to walk on.
If after therapy the pain has decreased and bone turnover markers have returned to normal, crutches should be discontinued after 2-3 months. But don't rush. Unloading the joint will relieve pain and prevent further destruction of the femoral head. The gentle regime accelerates healing, it is faster and easier.
On the other hand, the patient needs exercise therapy. A special set of exercises will reduce pain and swelling of the joint and increase its mobility. Physical exercise will develop not only the joint, but also the muscles surrounding it, preventing the development of malnutrition.
Obese patients are advised to combine exercise with a specially selected diet. This combination will allow you to achieve better results.
The importance of physical therapy at the rehabilitation stage should be especially emphasized. It will help not only to develop the operated/replaced joint, but also to prevent its instability.
6.3. Necrosis of the femoral head caused by glucocorticoids
Typically, necrosis of the femoral head caused by glucocorticoids appears either 2-3 weeks or 1-2 years after taking these drugs. In 1949, Hench described the treatment of rheumatoid arthritis with glucocorticoids (hereinafter referred to as hormones for short), which are widely used in the treatment of various intractable diseases with satisfactory results. Unfortunately, the future has shown that they also have adverse effects. Fisher et al (1969), conducting pathological studies of ANFH caused by hormones, found that the bone marrow cavities and bone cells are filled with fatty inclusions, fatty liver degeneration, and hyperlipidemia. Fat droplets in the blood can also lead to subchondral embolism, intramedullary blood stasis, increased intraosseous pressure, and bone marrow edema due to hypoxia. Harrington (1971) reported on two groups of patients who underwent kidney transplantation. In group 1 of patients, 3 weeks after surgery, with an average prednisolone level of 2,900 mg, necrosis of the femoral head was detected in 24% of patients. In group 2, in which the prednisolone level was 1180 mg, only 2 patients out of 116 (2%) developed necrosis of the femoral head. That is, in group 1, the incidence of necrosis was 10 times higher than in group 2.
The results of other experiments have confirmed that if healthy white rabbits are given an injection of hydrocortisone acetate at a rate of 8 mg/kg every week, then 3 months after opening under a microscope one can detect fragile and crumbly bone tissue in the head of the femur, an increase in fat in the subchondral cavities of the femoral head bones, a decrease in the content of bone cells in trabeculae, a dense coloration of some pyknotic cell nuclei, the disappearance of some bone cells in bone lacunae, a noticeable decrease in the number of bone cells per unit area. In the skeletal blood vessels, it can be seen that fat emboli are distributed in the subchondral part of the femoral head, the cells are edematous, and there are unusually many fat cells in the medullary tissue of the femoral neck. In addition, compression venules formed by the blood sinusoid are visible, the obturator foramen are unclear, the number of capillaries has decreased and their filling is insufficient, and in the capillaries located closer to the edges of the cartilage, the blood filling is very poor, the density of capillaries per unit area in the femoral head has decreased significantly, the network capillaries noticeably thinned out, blood flow in arterioles and capillaries acquired a sandy appearance, aggregation of erythrocytes appeared, and blood flow speed decreased.
The results of a serological study confirmed that the content of total cholesterol and triglycerides increased in the blood serum of animals. The results of the experiment indicate that glucocorticoids greatly destroy the trabeculae, capillaries and subchondral structure of the femoral head, which loses its mechanical properties, and all this leads to the death of its cells.
This is how hormones cause ANFH. The mechanism of this necrosis is a violation of fat metabolism, which contributes to the appearance of hyperlipidemia and fatty degeneration of the liver, as well as a large accumulation of fat cells in the medullary cavity of the head: fat embolism occurs in its circulatory system, hypoxia of bone cells, edema and destruction of the bone matrix. As a result, bones become brittle and can easily break. An increase in the number of fat cells in the medullary cavity of the femoral head and a decrease in the number of bone cells in the trabeculae, as well as compression to which the capillaries are subjected as a result of structural destruction, accelerate the occurrence of necrosis.
ANFH caused by hormones is classified as drug-induced bone necrosis. Currently, the incidence of this type tends to increase, so doctors need to carefully analyze whether there are any other drugs that, like glucocorticoids, can cause necrosis of the femoral head.
Types of postoperative scars
Keloid.
A lumpy scar made of overgrown connective tissue that is red or bluish in color. It looks like a tumor or a mushroom cap. The size of the keloid scar is larger than the wound itself, it hurts, itches, and sometimes pulsates.
Hypertrophic.
Outwardly similar to a keloid, but its size does not extend beyond the wound. A hypertrophic scar does not cause any discomfort and lightens over time.
Normotrophic.
A well-healing scar is initially convex and reddened, after 3 months it becomes almost invisible, there is no sensitivity.
6.4. Osteoporosis
Osteoporosis (lat. osteoporosis) is a disease of bone tissue due to metabolic disorders, manifested by changes in the structure and thinning of the bone, leading to deformation and fractures. The main changes characteristic of osteoporosis and determined by special studies are expressed in a decrease in the number of load-bearing trabeculae and bone mass per unit area.
The formation of the skeleton, as a rule, by the age of 24-25 provides a peak in bone mass, then, with increasing age, the bones thin out and become less strong and elastic. This can be partly explained by the fact that after about 35 years of age, calcium leaching from bones occurs more rapidly than transport and deposition into bone tissue. This, as a rule, is inherent in everyone, but in some people, with certain changes in metabolic processes, bone tissue proteins are lost, the balance of microelements is disturbed and leaching becomes excessive, which ultimately leads to osteoporosis.
Osteoporosis affects the entire skeleton, but most often the hips, forearms and vertebrae. If we look at the average graphical picture of changes in bone density in accordance with age, we will see a period of low bone density in a growing and developing organism, when metabolic processes are represented mainly by bone formation and its slight resorption. This is typical for childhood and adolescence. At 25 years of age, when maximum bone mineral density is reached and the metabolic processes of bone formation and resorption (resorption) are balanced, bone density is maintained. After 50 years, when, due to certain shifts in metabolic processes and endocrine changes, resorption prevails over bone formation, a mechanism is formed in the body for loss of bone density by an average of 3-5% per year.
Biochemical parameters in patients with osteoporosis indicate not only a decrease in the content of calcium, mainly the ionized form, and phosphorus in the blood, but also an increase in the content of alkaline phosphates and a decrease in the level of calcium in the urine. The total amount of calcium in the body is 1.2-1.5 kg, the presence of other inorganic substances - phosphorus, sodium, potassium, magnesium - is necessary to maintain metabolic processes, absorption of calcium by the intestines and transport by proteins, as well as for the reabsorption of calcium by nephron tubules. Bone tissue contains predominantly 25-30% water and 70-75% inorganic and organic substances.
Inorganic substances contain 60-70% calcium phosphate and calcium carbonate (approximately 700 g), of which 99% is found in bone tissue. Phosphorus in bones is approximately 440 g. Of organic substances, the content of ossein is 20-40%. The organic components of bone form a network structure that gives bone strength and withstands various stresses. Research results confirm that inorganic substances allow bone to withstand compression, and organic collagen fibers allow it to withstand tension.
Bone, being an ideal structural material, plays the role of support and leverage, has high strength and low weight. Some researchers believe that bone is much stronger than granite, and its density is much less than that of steel and granite. Bone has the greatest resistance to compression in the longitudinal direction, and when stretched, it is easily damaged, so the placement of trabeculae depends on the load-bearing capacity of the bone.
The distribution of stress in bone under load depends on the shape and structure of the bone itself. Bone's ability to withstand prolonged stress and fatigue is limited. Bone is very sensitive to physiological stimulation by tension: the greater the force of tension, the greater the trabeculae and bone density.
Radiographs of osteoporosis indicate that trabeculae in cancellous bone thicken and decrease in number, and cortical bone becomes thinner and takes on a layered appearance. Often there is an expansion of the epiphyseal line, and in childhood brush-like formations form on the metaphysis.
Osteoporosis can be accompanied by metabolic diseases of the skeleton: softened bone fluorosis, renal osteodystrophy, hyperparathyroidism, calcium assimilation disorders, nutritional osteodystrophies. Multifactorial changes in the body under certain conditions contribute to the formation of osteoporosis with obligate changes in the structure of the femoral head and the development of ANFH.
Osteoporosis, which causes changes in the structure of the femoral head and leads to compression obstruction of the microvasculature, creates ischemia and conditions for the development of aseptic necrosis. Considering the pathogenetic connection of osteoporosis and aseptic necrosis, it is very important for each doctor and patient to use the principle of individual diagnosis and prevention of osteoporosis with examinations of increasingly younger people, up to children and adolescents, to assess their rate of bone mass gain.
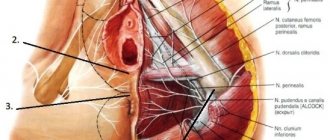
Penile fracture is a traumatic rupture of the tunica albuginea of the corpora cavernosa of the erect penis.
In the structure of emergency andrological conditions, penile fracture ranks first. According to the urgent andrological service in Moscow, penile fractures account for at least 60% of the total number of patients who sought emergency andrological help [1].
When the penis is fractured, the tunica albuginea of the penile body is first torn, sometimes in combination with a tear of the corpus spongiosum and urethra. Trauma to the urethra is accompanied by an average of 10% of penile fractures.
A fracture of the penis is possible only in a state of erection. Rupture of the tunica albuginea of a non-erect penis is possible, but is extremely rare. Due to the significant thickness of the tunica albuginea in the state of detumescence, which is about 2 mm, blunt trauma to the penis usually does not lead to rupture of the latter. Due to the rupture of the saphenous veins, a hematoma is formed, which tends to spread rapidly. Due to the good blood supply to the penis, a hematoma can reach significant sizes, lead to swelling of the foreskin, make urination difficult, and even require drainage of the bladder.
The distinction between true penile fracture and injury to the non-erect penis has important implications for clinical practice. When a penis is fractured, the tunica albuginea and sometimes the corpora cavernosa of the penis are always damaged. When the penis is bruised, the vessels are predominantly damaged, sometimes the tunica albuginea, but the corpora cavernosa are always intact (of course, unless the organ is completely crushed) [2].
The diagnosis of a penile fracture in the vast majority of cases is purely clinical, that is, based on the results of questioning and physical examination of the patient. Instrumental examination methods are used for differential diagnosis in case of an ambiguous clinical picture, as well as to clarify the location and size of the defect in the tunica albuginea.
At the time of injury, the patient notes a crunching sound. Previously, this was considered pathognomonic for a fracture of the penis, but recent studies have shown that similar phenomena occur with isolated subcutaneous rupture of the vessels of the penis, and with a “false” fracture of the penis, consisting of a rupture of the inner layer of the tunica albuginea. Almost immediately, detumescence occurs, acute swelling of the organ and a change in the color of its skin develop. Pain syndrome is natural in any acute injury, but there is no relationship between the severity of pain syndrome and the size of the defect in the tunica albuginea. Upon examination, the penis is deformed with a deviation in the direction opposite to the localization of the defect in the tunica albuginea.
The rapid, sometimes immediate, onset of detumescence has a high diagnostic value as a marker of rupture of the tunica albuginea. Smooth, gradual development of detumescence is characteristic of other types of trauma to the penis - “false” fracture, rupture of the ligament supporting the penis, rupture of the saphenous vein of the penis.
Buck's fascia usually retains its integrity during fractures of the penis; a dense, tense hematoma, well demarcated from the surrounding tissues, is formed over the site of the defect in the tunica albuginea, which is called the “indicating mound” symptom. In the event of a rupture of Buck's fascia, which happens quite rarely, the hematoma gradually spreads into the scrotum, perineum and lower abdominal wall.
Currently, for true fractures of the penis, the most active surgical tactics are recommended, consisting of revision of the penis, suturing of traumatic defects, and evacuation of hematomas [3,4,5]. In case of damage to the cavernous bodies, the natural course of interstitial hematoma ends with segmental cavernous fibrosis, which results in the development of persistent, irreversible erectile dysfunction that is not subject to conservative treatment.
Various options for surgical access to the corpora cavernosa of the penis are described. In our opinion, it is advisable to give preference to a circular subcoronal incision followed by deglovation of the skin of the penis. Unlike other (cosmetic) access options, the above approach allows complete bilateral exposure of the corpora cavernosa. If a rupture of the tunica albuginea is detected, it does not make sense to perform tissue separation below the rupture site, because The defect of the tunica albuginea is almost always single.
According to the urgent andrological service in Moscow, the incidence of complications with this access is less than 5%. The structure of complications is dominated by necrosis of the skin of the penis; suppuration of the postoperative wound and the formation of an abscess are also possible. Acute cavernitis is not typical for this clinical situation - we have not observed a single case of cavernitis complicating a penile fracture.
Absorbable suture material should be used to close a tunica albuginea tear. When using non-absorbable suture material, remaining nodes can be a source of pain for the patient and make sexual intercourse difficult.
An obligatory stage of surgical intervention is performing the Gittes test: applying a tourniquet to the base of the penis, followed by puncturing the intact corpus cavernosum with a butterfly needle and subsequent instillation of an isotonic sodium chloride solution. This test allows not only to identify previously undiagnosed defects in the membrane, but also to check the tightness of the applied ligatures [6].
A penile fracture is a situation requiring emergency care, so such patients can be admitted to all urology departments. Due to the relatively low incidence of penile fractures, a significant part of urologists experience difficulties in providing assistance to this specific category of patients. Rarely, but there are still cases of untimely surgical intervention, inadequate access to the cavernous bodies, etc. All this dictates the need to focus the attention of practicing urologists and organizers of urological care on a clinical case of total necrosis of the skin of the penis in a patient operated on for a fracture of the penis.
Clinical case:
Patient N., 34 years old, independently applied to the emergency department of the City Clinical Hospital named after. D.D. Pletnev with complaints of severe pain in the penis area, blackening and partial detachment of his skin.
From the anamnesis it is known that two weeks before going to the clinic in one of the hospitals in Moscow, the patient, due to a traumatic rupture of the tunica albuginea of the penis (“fracture” of the penis), urgently underwent revision of the penis, evacuation of the hematoma and suturing of the tunica albuginea. sheath of the penis. Antibacterial prophylaxis was carried out with ceftriaxone. On the third day after surgery, the patient was discharged for outpatient treatment by a urologist at his place of residence with recommendations for treating postoperative sutures with a solution of brilliant green and elastic bandaging of the penis.
However, several days after discharge, the patient began to notice a progressively spreading area of change in the color and consistency of the skin distal to the suture line, which in turn was located near the root of the penis. Over time, the skin acquired a brown, sometimes almost black color with the formation of areas of ulceration (Fig. 1). These changes were accompanied by intense pain, which required seeking emergency urological help at the City Clinical Hospital named after. D.D. Pletneva.
Fig.1. Patient N. General view of the penis before surgery. Areas of skin necrosis and a skin defect in the area of postoperative suture dehiscence are visible.
On examination, the penis is in a state of detumescence. The line of the circular postoperative suture is visible, 2 cm from the root of the penis. Distal to the suture line there are areas of skin necrosis with the formation of trophic ulcerations. There were no signs of an infectious-inflammatory process (penile phlegmon, cavernitis, etc.).
After a general clinical examination, which did not reveal any concomitant diseases in the patient, surgical revision of the penis, necrectomy (Fig. 2) and the first stage of the Sapozhkov-Reich operation - immersion of the penis into the scrotum (Fig. 3,4,5) were performed.
Fig.2. Patient N. A revision of the penis and necrectomy was performed. A subcutaneous canal has been formed in the scrotum along the midline. A hole is marked for the removal of the glans penis
Fig.3. Patient N. Formed subcutaneous canal on the scrotum
Fig.4. Patient N. The penis is passed through the subcutaneous canal of the scrotum, the head is brought out
Fig.5. Patient N. The postoperative wound is sutured with an interrupted suture
Antibacterial prophylaxis was carried out with amoxicillin/clavulanate. No infectious and inflammatory complications were observed. On the third day of the postoperative period, the patient was discharged in satisfactory condition under observation by a urologist at his place of residence. The sutures were removed on an outpatient basis on the tenth day of the postoperative period.
After 3 months, patient N. was re-hospitalized at the City Clinical Hospital named after. D.D. Pletnev in a planned manner to carry out the second stage of the Sapozhkov-Reich operation.
At the time of hospitalization, the patient complained of a cosmetic defect and the inability to have sexual intercourse. Upon examination, it was noted that the skin of the scrotum was stretched, and there was a sufficient supply of tissue for plastic surgery. The patient underwent the second stage of the Sapozhkov-Reich operation. Antibacterial prophylaxis was carried out with amoxicillin/clavulanate. No infectious and inflammatory complications were observed. On the fifth day, the patient was discharged in satisfactory condition under observation by a urologist at the place of residence with recommendations for sexual rest for one month.
DISCUSSION
In terms of discussion, it is advisable to analyze each stage of the diagnostic and treatment process from the position of reasonable sufficiency.
A patient with an obvious clinical picture of a traumatic rupture of the tunica albuginea (“fracture”) of the penis is urgently admitted to the urology department of one of the city hospitals, where he is immediately operated on. At this stage, everything is correct: modern urology recommends the most active surgical tactics for this type of injury. Even if a complete rupture of the tunica albuginea had not been confirmed (that is, the “fracture” would have been recognized as false), the choice in favor of immediate revision of the penis should be considered correct.
The surgeon accessed the tunica albuginea and cavernous bodies through a proximal circular approach. This decision seems doubtful to us due to failure to take into account the peculiarities of the blood supply to the penis. Axial longitudinal blood supply to the organ involves the use of a circular paraglandular approach, in which the risk of crossing large vessels, and therefore ischemic complications, is minimal. On the contrary, incisions made near the root of the penis carry the risk of developing ischemia of the distal part of the organ. This risk was realized.
When re-applying for urological help, the patient had indications for revision of the penis with necrectomy. However, it was apparent that there was not enough intact skin to cover the penis after necrectomy. There were two alternatives: open management of the postoperative wound in the hope of spontaneous closure of the skin defect and replacement of the skin defect with a heterotopic skin flap.
Open management of an extensive wound of the penis is associated with significant recovery time for the patient, a high risk of the formation of rough scars and deformation of the penis. In this case, the patient may experience significant discomfort during erection. In our opinion, open management in modern conditions is indicated only in the presence of an infectious process in the wound of the penis.
Replacement of a skin defect with a heterotopic skin flap using the Sapozhkov-Reich method is carried out in two stages, the first of which is immersion of the penis into the scrotum. This prevents both infectious and inflammatory processes in the wound of the penis and cicatricial deformities. In the second stage, the skin of the penis is formed from the tissues of the scrotum. This technique is relatively simple to perform, does not require special microsurgical skills and equipment, and can be performed in any urological hospital. A significant contraindication to the Sapozhkov-Reich operation is an infectious process in the wound of the penis. In our observation, despite extensive foci of necrosis, there were no signs of wound infection, which determined the choice of this technique.
Subsequently, the patient was able to completely restore the functionality of the organ without deformations or cosmetic defects.
A few words about antibacterial prophylaxis. If there is no violation of the integrity of the urinary tract, then the goal of antibacterial prophylaxis is to prevent suppuration of the postoperative wound [7]. The most common causative agents of wound infections are gram-positive cocci - non-hospital strains of Staphylococcus spp., less commonly Streptococcus spp. Therefore, the drugs of choice are I-II generation cephalosporins and inhibitor-protected aminopenicillins. If the patient has an open wound that is more or less contaminated, then preference should be given to inhibitor-protected aminopenicillins, since they can prevent the proliferation of not only the gram-positive flora characteristic of this situation, but also anaerobic pathogens.
In the present patient, antibacterial prophylaxis was initially administered with a third generation cephalosporin. The drug has high activity against non-hospital gram-negative bacilli - characteristic pathogens of nonspecific infectious and inflammatory diseases of the genitourinary system [8]. But in the situation under study, these pathogens are of little relevance, since the urinary tract was not directly injured. Staphylococcus is relevant. The antistaphylococcal activity of ceftriaxone is low, although it is considered clinically significant. The choice of this drug cannot be considered completely erroneous; it would be more correct to say that it is not the best in the situation under study.
Subsequently, amoxicillin/clavulanate was prescribed, which demonstrated the highest effectiveness in the regimen of antibacterial prophylaxis during surgical interventions on the penis [9].
CONCLUSION
The described case, in our opinion, is not a consequence of a combination of unfavorable circumstances. This is a purely iatrogenic complication, obviously preventable with technically correct surgical access to the corpora cavernosa. This is a consequence of insufficient training of the surgeon, and theoretical training at that.
In modern conditions, such complications are fraught with complaints to supervisory organizations, financial claims from insurance companies, as well as lawsuits. In this case, the patient was able to completely regain erectile function, and there were no complaints on his part.
But not all risks were realized. In conditions of a significant volume of ischemic and necrotic tissue, an infectious process can occur at any time. In the absence of timely assistance, this is almost inevitable. Considering the severity and prevalence of the lesion, it can be assumed that the patient managed to apply 1-2 days before the development of the infectious-inflammatory process. What if he had turned out to be more patient and showed up at the urology clinic with penile phlegmon, or, even worse, with signs of bacteriotoxic shock? (Acute cavernitis and phlegmon of the penis have an extremely aggressive course and are often complicated by bacteriotoxic shock). Then there would be no talk of any preservation of erectile function. The level of organ amputation would be discussed. Administrative and/or financial costs for healthcare facilities in this turn of events are highly likely.
In conclusion, we emphasize once again: access to the corpora cavernosa is paraglandular with subsequent deglovation of the penis; the need to refuse such access must be clearly justified. For example, with very proximal defects of the tunica albuginea, the above described access may be inconvenient, then there are two options: a longitudinal incision in the projection of the defect (the surgeon must clearly understand the location of the damage, which is not always possible) or transscrotal with dislocation of the penis into the wound, which is more traumatic, but allows for an audit of the organ.
LITERATURE
1. Maksimov V.A., Yarovoy S.K., Khromov R.A., Prokhorov A.V., Stranadko M.V. State and prospects for the development of emergency andrological care services in Moscow. Urology 2012;(1):72-76.
2. Yarovoy S.K., Khromov R.A., Dzidzaria A.G., Prokhorov A.V. Issues of urgent andrology. Moscow. Uromedia. 2016. 120 p.
3. Urology. National leadership [Edited by Lopatkin N.A.]. Moscow. GEOTAR-Media. 2009. 1021 p.
4. Muentener M, Suter S, Hauri D, Sulser T. Long-term experience with surgical and conservative treatment of penile fracture. J Urol 2004;172(2):576-579.
5. Athar Z, Chalise PR, Sharma UK, Gyawali PR, Shrestha GK, Joshi BR. Penile fracture at Tribhuvan University Teaching Hospital: a retrospective analysis. Nepal Med Coll J 2010 Jun;12(2):66-8.
6. Mydlo JH. Surgeon experience with penile fracture. J Urol 2001;166:526-529.
7. Maksimov V.A., Yarovoy S.K., Stranadko M.V., Misyakova O.A. Empirical antibacterial prophylaxis in urology. Experimental and Clinical Urology 2012;(1):76-84.
8. Handbook of antimicrobial therapy [Edited by Kozlov R.S., Dekhnich A.V.]. Smolensk MACMAH. 2010. 416 p.
9. Yarovoy S.K., Khromov R.A. Tactics of emergency urological care for ischemic priapism. Attending Physician 2014;(1):46-49.
| Attachment | Size |
| 540.36 KB |
‹ Neurological disorders in chronic kidney disease Oxidative stress and pathozoospermia ›
6.5. Congenital varus position of the femoral neck
Congenital varus position of the femoral neck is also called varus position of the femoral neck due to developmental delay. In this case, the gait resembles the walking of a person with a congenital dislocation of the hip. The x-ray shows that the characteristic signs of this disease are: a decrease in the neck-shaft angle, a lack of calcium in the lower part of the femoral neck and the formation of a triangular bone.
The mechanism and causes of this disease are unclear. They are thought to be associated with congenital abnormal development of the epiphyseal plate and interference with the calcification process within the femoral neck.
6.6. lupus erythematosus
Hebra (1854) described lupus erythematosus, which was mainly located on the face, cheeks and nose in a butterfly pattern. Cazenave (1851) proposed to call this disease lupus erythematosus, perhaps it was discoid lupus erythematosus. Kaposi (1872) used this name to distinguish only manifestations of skin damage, but not damage to internal organs. Osler (1895-1904), calling this disease exudative erythema, described various manifestations of systemic lupus erythematosus in the internal organs. Libman and Sack (1924) called this disease non-rheumatic warty endocarditis. Baehr (1935) presented autopsy materials on 23 patients, putting forward the idea of the dangers of solar radiation in this disease, and also described glomerulonephritis, which had the appearance of “golden turns of threads.”
Haggare (1948) was the first to prove the cellular nature of lupus using bone marrow extraction. Miescher and Fauconnet (1956), observing growth factors of lupus erythematosus cells that were absorbed by blood serum when they came into contact with isolated cell nuclei, suggested that lupus cell factors were antinuclear antibodies. Friou (1958) reported the use of fluorescent anti-human globulins for the detection of antinuclear antibodies. Klemperer (1942), having studied systemic lupus erythematosus and dermatosclerosis, proposed calling them diffuse colloid disease. Despite the fact that there is still debate in scientific circles about the nature of these diseases, the concept of “colloid disease” was accepted by everyone very quickly. In 1952, Ehrlich proposed the term “connective tissue diseases,” which gradually replaced the previous name.
Systemic lupus erythematosus is a multiple autogenous autoimmune disease affecting many systems and organs. The mechanism of this disease mainly consists of the deposition of immune complexes in all internal organs, but the exact causes of the disease have not yet been fully explained.
Systemic lupus erythematosus causes ANFH due to the deposition of immune complexes. It activates complements and generates active mediators that penetrate bone tissue (trabeculae, mesh structures of bone marrow, microcapillaries inside the bone) and destroys them, changing the viscosity and rheology of the blood, forming blood clots. As a result of this, osteolytic necrosis occurs in the head of the femur, also affecting the acetabulum and branches of the ischium.
The main pathological changes in lupus erythematosus are the occurrence of mucus-like edema and fibrinoid degeneration of connective tissue, as well as necrotizing vasculitis. It should be especially noted that when patients with lupus erythematosus take steroid hormones, the incidence of ANFH increases sharply after such treatment.
Systemic lupus erythematosus in combination with necrosis of the femoral head occurs, firstly, due to the fact that it directly causes this necrosis; secondly, because after taking steroid hormones, degeneration occurs in the structure of the femoral head, the mesh structure of the trabeculae, bone marrow and microcapillaries inside the bone are damaged, fat cells inside the bone hypertrophy, intraosseous microcapillaries are compressed in the area of greatest load of the femoral head, and the flow stops supply into the bone, and eventually the femoral head collapses.
Local complications
The following troubles may occur in the area of the surgical wound:
- bleeding due to a blood clotting disorder, slipping of the suture material from the vessel or insufficient restoration of hemostasis during surgery. To eliminate bleeding, stitches are placed, re-ligation is done, cold is applied to the wound, or hemostatic drugs are administered;
- hematoma due to a bleeding vessel. The hematoma is opened and removed by puncture. If it is small in size, it dissolves with ultraviolet irradiation or application of a compress;
- infiltrate - swelling of tissue within 10 cm from the edges of the suture due to infection of the wound or the formation of necrosis in the subcutaneous fat. Depending on the cause, physiotherapeutic procedures or surgical treatment are used to resolve it;
- suppuration - infiltrate with severe inflammation. To eliminate it, the sutures are removed, the edges of the wound are exposed, washed and drainage is installed;
- eventration - prolapse of internal organs outward due to suppuration, weak suturing of wound edges, increased intra-abdominal pressure during coughing or flatulence, or reduced tissue regeneration (healing). It is necessary to reposition the organs with aseptic technique, strict bed rest and wearing a tight bandage.
- Ligature fistula - occurs when an abscess forms around the suture material. It requires excision along with suture material.
6.7. Metabolic bone diseases
The skeleton, being not only an important support for the human body, but also the largest bone depot of minerals on which the human body rests, protects the heart, brain, lungs and circulatory system. It plays an important role in regulating mineral balance in the human body and metabolism. Bone tissue cells are very active, they are constantly renewed, and metabolism constantly occurs in them. The activity of bone tissue is influenced by numerous hormones, the most important of which are the parathyroid hormones: parahormone and calcitonin.
Metabolic bone diseases typically present with bone pain, deformity, pathological fracture, and muscle abnormalities.
Metabolic bone diseases mainly include: abnormal bone absorption, abnormal osteogenesis and abnormal bone mineral deposition. In general, metabolic bone diseases mean a disorder not only of mineral metabolism or metabolism in the bone matrix, caused by various reasons, but also biochemical and morphological changes in bone tissue, expressed in a number of painful and physical symptoms. There are many causes of metabolic bone diseases, but scientists do not have a consensus on this issue. Below are some of the metabolic diseases associated with ANFH:
• bone diseases caused by dysfunction of the endocrine glands; • bone diseases caused by malnutrition; • renal bone diseases; • bone conversion diseases (eg, osteitis deformans, hyperphosphatase disease); • bone diseases caused by medications and chemicals; • calcium deposition on bones; • bone tumor as a result of complications of metabolic bone disease; • osteogenesis imperfecta, osteosclerosis; • achondroplasia, osteodysplasia; • primary and secondary hyperfunction of the thyroid gland; • senile bone atrophy as a result of amenorrhea. The above diseases can, to varying degrees, create destruction of the femoral head, leading to ANFH.
6.8. Neurotrophic diseases of bones and joints
Neurotrophic diseases of bones and joints are also called Charcot's joint (neurogenic arthropathy). Neutrophic Charcot arthropathy is a kind of degenerative-dystrophic damage to joints caused by a violation of their innervation. This disease can be caused by the following reasons: • spinal cord lesions due to syringomyelia, tertiary syphilis (neurolues), B12 deficiency anemia (funicular myelosis), myelomeningocele, cauda equina tumors; • pathology of peripheral nerves in decompensated insulin-dependent diabetes mellitus, chronic alcoholism, vitamin B1 deficiency (beriberi), leprosy, familial amyloid neuropathy.
Charcot arthropathy is based on disturbances in the trophism and sensitivity of denervated articular tissues. Weakening of the trophically altered tendon-ligamentous apparatus leads to joint instability, which, in conditions of decreased deep (proprioceptive) and pain sensitivity, contributes to their increased trauma. Moreover, due to trophic disorders in bone tissue, even the usual load on the joints becomes excessive. Under the influence of these factors, pronounced destructive changes occur in the joints, in particular the development of osteolytic processes in the epiphyses with their fragmentation and the formation of intra-articular osteochondral sequestration. X-rays of the hip joint in this disease indicate the presence of osteoporosis and destruction of the bone structure, resorption of the femoral head, and in severe cases, resorption and disappearance of the head and neck of the femur. There is only a small amount of osteochondral formations (bone remains) in the joint, the damaged end of the femoral neck is dislocated upward, the acetabulum and the remains of the femoral neck look unclear, and bone density is reduced. In some images, the head of the femur is flat and the neck is shortened, bone density is increased, there are scattered sac-like light-transmitting zones and peripheral sclerosis between the head of the femur and the trochanter. The edges of the acetabulum are thickened and ossified, the distance between the head of the femur and the bottom of the acetabulum is widened, the head of the femur is shifted outward, the articular space is noticeably narrowed, under the greater trochanter there is a wide proliferation of periosteum in the form of onion peel, in the cartilage tissues at the upper end of the tibia there is a long band of calcification (fascia lata calcification), and in the lower part of the ischial tuberosity there is calcification in the form of a strip or circle.
Differential characteristics of Charcot's joint.
Charcot's joint differs from osteoarthropathy mainly in that it is manifested by the presence of osteoporosis, joint destruction, the presence of bone debris within the joint and its deformation. At the same time, the main thing is not so much osteoporosis, but the presence simultaneously with it of serious destruction of the joint, which is completely inconsistent with the patient’s subjective symptoms in the form of mild pain.
The severity of osteoporosis in osteoarthropathy is less than in Charcot's joint, and its main symptoms are joint pain and impaired movement.
Treatment of stages 3-4 necrosis
If the joint has already entered these stages, then the process of destruction of the femoral head has already begun. Exercise therapy and physiotherapy remain in the same vein as in the initial stages, but drug therapy undergoes changes. This is due to severe pain that patients can no longer tolerate. Stronger painkillers (diclofenac, tramadol) are prescribed.
The therapeutic effect is complemented by intra-articular injections of hyaluronic acid and the introduction of platelet-rich plasma.
Hyaluronic acid is an important component of synovial fluid. Such injections improve the shock absorption of congruent surfaces and facilitate their sliding relative to each other.
PRP.
PRP therapy (injection of platelet-rich plasma) activates the healing process. This is a young but promising direction. Under the influence of platelets, the production of collagen (the main “building material” of cartilage, connective and bone tissue) increases. Integration of osteoblasts occurs, helping to build new tissue, microcirculation improves due to the formation of new vessels.
Important: despite the breadth of possibilities of modern medicine, conservative treatment is effective only in the early stages. At the first signs of destruction of the head, the joint cannot be restored.
In this situation, a decision will be made regarding surgical intervention. Basic combinations of groups of surgical techniques [14]:
- intertrochanteric corrective osteotomy;
- modeling of the femoral head, including with intertrochanteric corrective osteotomy;
- modeling of the femoral head with autoplasty, including intertrochanteric corrective osteotomy;
- subchondral autoplasty of the femoral head, including intertrochanteric corrective osteotomy;
- segmental autoplasty of the femoral head, including intertrochanteric corrective osteotomy;
- reconstruction of the pelvic components, namely: pelvic osteotomy according to Chiari, including with intertrochanteric corrective osteotomy, supraacetabular acetabuloplasty, including with intertrochanteric corrective osteotomy.
No operation guarantees a full recovery. They reduce destructive processes inside the joint and reduce the risk of developing secondary coxarthrosis.