Consequences of vacuum abortion
The consequences of a vacuum abortion for the female body are minimal in comparison with other methods of terminating a pregnancy.
This method allows you to get rid of an unwanted pregnancy with minimal damage to the body. But still, like any intervention in the body, vacuum abortion does not always go smoothly. The most common consequences of a vacuum abortion are incomplete termination of pregnancy and the need to repeat the abortion using the classical method - the curettage method.
How to Prepare for Vacuum Aspiration
Removing a fetus using a vacuum syringe is as serious a procedure as any surgical intervention.
Therefore, preparation must be taken with full responsibility. The gynecologist will definitely refer the woman to studies such as:
- general blood test, general urinalysis;
- coagulogram;
- establishing accurate information about blood group and rhesus;
- blood for syphilis, HIV, gonorrhea, hepatitis, and other internal infections.
The gynecologist will also examine the patient in a gynecological chair, take smears from the vagina and cervix for microbiological examination and culture. An electrocardiogram may be required, as well as a thyroid hormone test.
This should be done for those who have problems with the heart or endocrine system.
The woman should also visit an ultrasound diagnostic room, where a specialist will verify the presence of pregnancy, set the exact timing, and make sure that there are no inflammatory processes in the pelvic organs or ectopic pregnancy. It is also important to determine the site of attachment of the fetus. All studies are aimed at excluding possible pathologies and contraindications.
On the day of surgery, you should take a light breakfast, do not pass it on. We need to take care of the way back home. If a woman is prone to fainting, she may need to arrange for someone to meet her and accompany her home.
It is also worth taking mental preparation seriously. Termination of pregnancy, as a rule. accompanied by the woman's mental suffering. Therefore, it is necessary to weigh everything and make a decision. And if this decision is final, tune in to a successful outcome.
Curettage of the uterine cavity
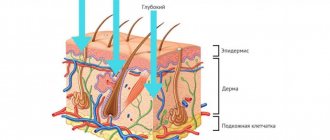
Endometrium
– the inner mucous membrane of the uterus, which is necessary so that the fertilized egg can attach to the wall. If fertilization does not occur, during the menstrual cycle the endometrium is shed and comes out as monthly discharge.
Curettage procedure
- cleansing - the uterine cavity, which is also called curettage, is carried out to remove the mucous membrane. During the process, the top layer is removed, and the sprout layer is preserved. This procedure is indicated for therapeutic and diagnostic purposes.
In what cases is curettage performed?
Intervention is necessary if:
- polyps were discovered - neoplasms in the uterine cavity;
- treatment of complications after abortion is required;
- the pregnancy was terminated as a result of natural causes or when fetal developmental arrest or death was diagnosed;
- diagnosed with endometriosis;
- it is necessary to clarify what type of structural disorders are observed (fibroids, hyperplasia, etc.);
- synechiae have formed - adhesions, the intrauterine walls are fused;
- a violation of placental discharge after labor was detected;
- diseases of the cervix, including oncological processes, were detected;
- the menstrual cycle is disrupted, bleeding is observed;
- during menopause, discharge containing blood clots appears;
- it is necessary to identify the causes of infertility.
If the pregnancy is terminated spontaneously, or a frozen pregnancy is diagnosed, it is necessary to remove the remnants of the placental tissue, otherwise an inflammatory process may occur. After an abortion, fetal membranes and embryonic tissue may remain in the uterine cavity, which is an indication for curettage.
Cleaning is also necessary before surgery to remove fibroids while preserving the uterus.
Contraindications
Curettage is not performed if:
- an active inflammatory process occurs in the genitals;
- the patient has severe diseases of the internal organs;
- the vagina requires sanitation.
If pathogenic flora is found in the vagina, it must first be eliminated, otherwise complications may arise during curettage or the pathological process will spread.
How is the procedure performed?
Scraping can take place as follows:
- blindly;
- under the control of special equipment - a hysteroscope.
The first option is fraught with complications. If the damaged mucosa was not completely removed, or the structure of the germ layer was damaged, bleeding may occur.
The hysteroscope allows you to closely monitor the progress
surgical intervention. Our clinic uses modern equipment, which eliminates the risks associated with blind cleansing and also increases the effectiveness of curettage.
Diagnostic curettage is performed to obtain endometrial samples
for subsequent histological examination. This procedure allows us to identify pathology, including the onset of the oncological process.
How to prepare for the procedure
Before the procedure, the patient is required to undergo a series of tests.
, including determination of blood clotting, the presence of infectious diseases,
ECG and ultrasound
. In addition, it is necessary to report medications that are taken on an ongoing basis.
For two weeks
Before the date of curettage
medications
that affect blood clotting
are discontinued
.
For three days you need to abstain from sexual contact, and also refuse to insert tampons or douching. Six hours
before the intervention
you should not eat or drink
.
The period of curettage depends on the purpose of curettage and the patient’s condition:
- The procedure is carried out as planned one to two days before menstruation
to relieve the unpleasant symptoms characteristic of the postoperative period. In this case, the effect on the menstrual cycle will be minimal.
- If the procedure is required urgently
, then it is performed
on any day
of the menstrual cycle. In this case, pain and bleeding may occur. The endometrial layer will take longer to recover. - Diagnostic curettage can be performed at different times of the cycle depending on indications
, on the basis of which this type of procedure is proposed. If menstrual function is impaired, it is necessary to obtain tissue for analysis from the fifth to the tenth day of the cycle; if there is a suspicion that menstruation occurs without ovulation, curettage is carried out two to three days before the start of menstruation.
How is curettage performed?
The intervention is quite painful, so our medical center uses general or spinal anesthesia
depending on the patient’s wishes and accompanying indications.
A woman sits on a gynecological chair in the operating room. First, treatment is carried out with an antiseptic composition
.
Then, using a gynecological speculum, the position of the cervix is revealed
. It is fixed with special tools and expanded.
To provide visual control, a hysteroscope tube is inserted
.
is done using curettes.
The endometrium is removed from the cervical canal, curettes are used to clean the anterior and posterior walls, and the lateral walls are scraped off last. If neoplasms are found that cannot be removed with a curette, other instruments are used.
After the procedure, antiseptic treatment
external genitalia.
Tissues must be examined for histology to exclude pathological changes.
Rehabilitation
During the rehabilitation period, discharge containing blood clots may appear for about a month. Minor discharge may bother you for ten days. To avoid spasms and accumulation of blood in the uterine cavity, a course of antispasmodics
, which are prescribed by a gynecologist on an individual basis.
The rehabilitation period after a planned procedure reaches four to five weeks. In the first 14 days you need to follow these recommendations:
- refrain from visiting a bathhouse or sauna, avoid possible hypothermia;
- refuse tampons and other measures affecting the vagina;
- reduce physical activity and temporarily interrupt sports activities;
- do not take a bath or swim in open water or pools;
- abstain from sexual contact.
On the first day after surgery, you need to be especially careful about maintaining intimate hygiene
.
Possible complications in case of unqualified intervention
The curettage procedure sometimes causes certain complications:
- blood may begin to accumulate (hematometra will appear);
- if cleaning was carried out blindly, the basal (germ) layer of the mucosa may be damaged, which can subsequently lead to infertility and is almost impossible to treat;
- an inflammatory process may occur in the uterine cavity;
- If the procedure was performed by unqualified specialists, perforation (breakthrough) of the uterine wall or tear of the cervix may occur.
Do not risk your own health - contact experienced gynecologists, and you will not encounter any of the possible complications!
Sign up for a consultation at the Dialine clinic!
We guarantee that the procedure, under the control of special equipment, will go quickly and cause a minimum of discomfort! Recommended reading:
- REMOVAL OF CERVICAL POLYPS
- MENSTRUAL CYCLE DISORDERS, HOW TO TREAT?
Vacuum aspiration after medical abortion
Medical abortion and vacuum aspiration are minimally invasive methods of terminating pregnancy. However, the medicinal version is more effective for up to 4 weeks, and the vacuum version is more effective for up to 5 weeks.
In approximately 3% of cases, pharmaceutical abortion ends unsuccessfully - the fertilized egg remains inside. In this case, in order not to injure the uterus with surgical instruments, vacuum aspiration is used.
This must be done because the fetus exposed to abortifacient drugs is damaged. There is a high risk that the child will be born very sick and even non-viable.
If time permits, then vacuum cleaning is the best way out, especially for nulliparous women. Vacuum aspiration in this case also, as a rule, preserves the woman’s ability to become a mother in the future. Restoring health after it occurs faster than after a surgical abortion.
Diagnosis of diseases using vacuum aspiration
Some diseases require analysis of a fragment of the endometrium of the uterus. For example, if endometrial hyperplasia is suspected, it is necessary to obtain material for analysis. Since mechanical intervention in the uterus is very traumatic, in this case a vacuum is used. This procedure is called aspiration biopsy. Through vacuum aspiration, the doctor obtains a fragment of the endometrium, while the operation itself does not require anesthesia for the patient; local anesthesia with a lidocaine solution is often sufficient, as well as taking conventional antispasmodics.
In our clinic, patients can receive vacuum aspiration services using the latest modern devices. Competent doctors provide a full range of services, from vacuum abortion to aspiration biopsy. Only here women can be sure that the medical services provided are performed at the highest level.
What tests need to be taken before the procedure?
The vacuum termination procedure involves preparatory measures, which necessarily include a visit to the gynecologist and testing. Let's explain why.
When giving a referral for an abortion, the doctor must be sure that the pregnancy really exists and is not ectopic. Since during a vacuum abortion, the embryo is detached from the walls of the uterus and subsequently absorbed into the catheter tube, it is important to follow the recommended timing for such an operation.
The fact is that at a period of 4-6 weeks, the connections between the fetus and the walls of the uterus are not yet very strong, and the egg is easily separated from the walls of the uterus and absorbed into the catheter. In the 7th week and later, this will be much more difficult, so the risk that part of the egg will remain in the uterus increases. It is no coincidence that when the time is prolonged, the doctor resorts to using a curette.
Vacuum abortion is not very good for a fetus up to 3 weeks - a small embryo is difficult to absorb, and during this period the medical method of terminating pregnancy works well. Therefore, when writing a referral for vacuum aspiration, the doctor will definitely prescribe a number of procedures.
Before vacuum aspiration, to clarify the diagnosis, gestational age and position of the uterus in the pelvis, a gynecologist is examined and a vaginal ultrasound is prescribed. The woman gives:
- general analysis of urine and blood;
- blood for clotting, group, Rh factor;
- hCG tests to more accurately determine the duration of pregnancy;
- tests for HIV, hepatitis B and C.
Since a mini-abortion has a number of contraindications (any viral and infectious diseases, including those of the reproductive system), the woman will also have to undergo a smear test. This is done in the interests of the patient herself: any virus that enters the uterus during aspiration can provoke serious inflammatory processes and complications. If necessary, the gynecologist prescribes additional examinations or a consultation with another doctor (therapist, surgeon).
Preparing for a mini-abortion
When performing aspiration under general anesthesia, you should not eat food 8 hours before the intervention. Intimate relationships should be avoided 3 days before the procedure.
Otherwise, the preparation is the same as for an appointment with a gynecologist. Gynecologist appointment
Women often ask what can replace a vacuum abortion; an alternative to vacuum aspiration is medical abortion. Medical abortion - termination of pregnancy without serious consequences?
Why is vacuum aspiration dangerous?
The vacuum method of abortion is one of the most reliable and gentle. However, there is no safe abortion. And this method is fraught with a number of complications. The dangers are:
- disruption of hormonal levels, leading to serious consequences in the form of weight changes, tumor formation, metabolic disorders, and so on;
- psychological trauma that risks developing into depression;
- intrauterine bleeding;
- pain in the lower abdomen;
- inflammatory processes in the pelvic organs;
- incomplete abortion, when particles of the fertilized egg remain;
- menstrual disorder;
- infection;
- air embolism, when air enters the blood vessels and the woman dies (this is extremely rare);
- perforation of the uterine wall while measuring its depth with a probe;
- damage to the cervix with the need for suturing;
- Infertility is a rare complication, but can also occur due to improperly performed surgery.
Complications can occur early, that is, immediately after surgery. And also late - they are revealed months later in the form of hormonal problems, disruption of the menstrual cycle, and infertility.
Postoperative period
In general, discharge occurs on the same day. During the recovery period after anesthesia, dizziness, weakness, and discomfort in the lower abdomen may be observed. The first few hours after surgery there is moderate bleeding with clots. If there is no discharge, this may be an alarming sign; you need to inform your doctor about it. Normally, bleeding should be light and last from a week to two. This is normal, as is nagging pain in the lower abdomen.
In the postoperative period you should refrain from:
- douching;
- intimate contacts;
- use of sanitary tampons;
- taking medications not prescribed by a gynecologist;
- bathing and swimming in bodies of water;
- increased physical activity;
- alcohol;
- heavy food;
- bath, baths, saunas.
A calm lifestyle and avoidance of stressful situations are recommended. It is necessary to drink herbal teas and eat light, low-fat foods, and also use the shower without aggressive hygiene products. After two weeks, you must come for an examination with your doctor. If you begin to have yellow or brown discharge with an unpleasant odor, or if the strong discharge does not stop, you should immediately consult a doctor.
Prevention of complications after vacuum aspiration
Even if the operation was successful, safety precautions should be followed to avoid complications. What is being done for this:
- after the procedure, the woman lies on her stomach for about 30 minutes in the presence and under the supervision of medical workers;
- if everything is in order, the woman can go home, but remember the restrictions;
- in the first 4 weeks you should not have sex, as this can lead to infection and bleeding;
- You should not take baths, saunas, or get too cold;
- visiting open and closed bodies of water is prohibited for a month;
- you cannot lift weights;
- It is contraindicated to use tampons in the first month after surgery;
- You should be careful and serious about genital hygiene, wash them with warm water, possibly with baby soap.
To prevent infectious inflammation. The doctor may prescribe antibiotics and antifungal medications. Taking special herbal teas will be useful. Their choice should be discussed with a gynecologist.
As a rule, oral contraceptives are prescribed in the first months, which will protect against re-conception, which is dangerous in the first 6 months after an abortion. These contraceptives will also help restore hormonal levels.
After 2 weeks, you should visit the gynecologist again to do a control ultrasound and make sure. that everything went well, there was no inflammation or bleeding. Fusion of the walls of the uterus.
What you should be wary of in the first days after an abortion:
- absence of discharge or very scanty bleeding (this may indicate cervical spasm);
- discharge in the form of blood clots for more than 3-4 days (possible intrauterine bleeding);
- excessive bleeding for several days after the abortion;
- purulent vaginal discharge;
- increased body temperature;
- nagging, aching pain in the lower abdomen.
After termination of pregnancy, a woman is required to be more attentive to her health and promptly seek medical help for any suspicious manifestations.
Is sex possible after a mini-abortion?
For about 3 weeks after vacuum aspiration, and preferably until the end of the first menstruation, sexual intercourse should be avoided. The reason is trauma to the genital organs, although not as severe as with a classic abortion.
You should also know that the discharge observed in the first days after the operation is not menstrual, and already 2 weeks after the abortion, a woman can become pregnant. This means that the use of contraceptives becomes mandatory from the first sexual intercourse after an abortion. It is also recommended to use a condom in the first months - it will protect the woman’s vulnerable genital organs from infection.
Pregnancy after vacuum aspiration
Many women are concerned about the issue of future pregnancy: when it is possible to afford to become pregnant again and how quickly conception can occur.
It all depends on the individual characteristics of the woman’s body and on the correct operation to terminate the pregnancy.
Reconception may not occur for some time due to:
- hormonal disorders;
- pathologies in the endocrine system;
- due to inflammation in the pelvic organs, the formation of adhesions that impede the advancement of the egg, disruption of the patency of the fallopian tubes;
- due to trauma to the cervix and its inability to hold the fetus (risk of miscarriage).
After any type of abortion, even such a gentle one as vacuum aspiration, you should plan for a future pregnancy. A consultation with a gynecologist will be required. If you become pregnant without a preliminary examination, there is a high probability of miscarriage, missed abortion, or the birth of a child with health pathologies.
In the first six months, at least 3 months, repeated pregnancy is not recommended.
| Termination of pregnancy in early and late stages | Reception is strictly by appointment, make an appointment by phone: +7 | Prices for services | Reviews about the clinic |
Possible consequences: is vacuum mini abortion safe?
As a rule, vacuum aspiration does not cause problems for either the doctor or the woman. However, sometimes negative consequences can still occur.
- Incomplete abortion or continued pregnancy. It happens that parts of the fetus, and sometimes the entire fetus, remain in the uterus. The first condition is indicated by severe pain, discharge with blood clots and an unpleasant odor, the second – by signs of toxicosis.
- Damage to the genital organs: cervix and uterine walls. This happens when using metal dilators and curettes and requires immediate surgical intervention.
- Inflammatory processes. The reason is infection in the female genital organs. Untimely treatment is fraught with serious consequences, including the development of secondary infertility.
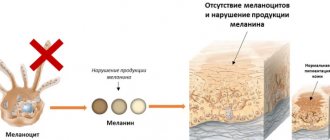
- Disorders in the endocrine system and menstrual cycle. After an abortion, a woman’s body, which is primed for pregnancy, experiences a hormonal imbalance, which can affect the functioning of all organs.
- Miscarriage. Dilation of the cervix can weaken it and cause miscarriages in the future.
Therefore, it is very important to undergo a control ultrasound - it is prescribed 1-2 weeks after vacuum aspiration. Moreover, not only if one of the listed symptoms appears, but also if after the operation everything goes well and the woman feels normal.
Ultrasound after vacuum aspiration
After any method of abortion, it is recommended to undergo an ultrasound to ensure a successful result.
A vacuum mini-abortion is performed under the control of an ultrasound machine. But even in this case, after two weeks you need to do a repeat ultrasound examination.
This is done to ensure that:
- the entire fertilized egg has been removed;
- there is no internal bleeding and no delay in the removal of blood to the outside;
- no inflammatory processes, formation of polyps;
- the epidermis at the site of fetal separation heals well.
If the operation was performed without the control of an ultrasound machine, then an ultrasound examination is prescribed 2-3 days after the vacuum abortion.
A pelvic ultrasound after an abortion also gives an idea of the health of the organs in this area.
Can there be abnormalities in menstruation after an abortion?
The first menstruation after an abortion may have some deviations. In particular, the first discharge often has a rather unpleasant odor. In some cases, their consistency also changes: if a woman has always had liquid discharge, it may become thicker and vice versa. During the first post-abortion menstruation, some atypical pain in the lower abdomen may appear.
An unusual onset of menstruation should be a reason to seek advice from your treating gynecologist, because if the problem turns out to be serious, it can often lead to further infertility and various intimate problems
What anesthesia is used for vacuum aspiration?
Vacuum cleaning, although a minimally invasive procedure, still requires anesthesia, as it involves pain. The anesthetic agents in our clinic are modern, more gentle and do not cause allergic reactions.
What types of anesthesia are there:
- Local anesthesia is most often used. It completely removes pain, but the woman is conscious, understands what is happening, and answers questions.
- The half-sleep method is also used, when an anesthetic drug is injected intravenously, reducing the ability to perceive reality. In this case, the woman is almost in a sleeping position, does not understand what is happening to her, does not feel pain, but can hear distant sounds. She breathes on her own and quickly recovers from anesthesia.
- At the woman's request, general anesthesia can be used. It requires an equipped operating room and the presence of an anesthesiologist. The woman is completely asleep, the artificial respiration machine supports vital systems. The woman doesn’t remember anything, but wakes up in the ward.
There are many drugs for anesthesia. The doctor chooses the one that is safest for a particular woman, taking into account her physiology and health status.
How much does a vacuum abortion cost?
Each clinic sets prices for vacuum aspiration at its own discretion. When choosing a medical center, be careful. The price list often indicates the cost of the procedure itself without tests, ultrasound and anesthesia. In our clinic, the cost of the procedure at the all-inclusive rate is 15 thousand rubles. This includes absolutely all tests, examination and pain relief!
Benefits of Vacuum Aspiration
Despite the possible consequences, mini-abortion is considered gentle and therefore the more preferable method of surgical termination of pregnancy. And this is quite understandable.
- Damage to the mucous membrane and cervix, except in rare cases, is minimal, so the woman recovers faster after surgery.
- In the first weeks of pregnancy, the psychological connection with the life born inside is not yet so strong, and abortion becomes less stressful for the woman than in later stages.
- The patient can go home a few hours after aspiration and return to her normal life the very next day.
But be that as it may, a woman should remember that even a tiny embryo is already a new person. Therefore, you should foresee possible methods of contraception in advance and thereby save yourself in the future from the awareness of guilt in front of your unborn child.
CLICK TO MAKE AN APPOINTMENT, TEST OR ULTRASOUND
Which doctor performs vacuum aspiration?
Vacuum cleaning is performed by a gynecologist. It is within his competence to establish pregnancy, determine indications and contraindications for any type of abortion, and help to rehabilitate after an artificial termination of pregnancy. He also performs abortions provided he has completed additional training.
Our clinic employs a gynecologist who has certificates for all types of services. He has gained extensive experience and an impeccable reputation.
Where to do vacuum aspiration
Vacuum abortion, like any other type of abortion, is performed only in a medical institution.
Our clinic has a fully equipped gynecologist's office, as well as an operating room for more complex surgical interventions.
Advantages of choosing our clinic to receive vacuum cleaning services:
- our own laboratory makes it possible to quickly pass all the necessary tests before an abortion within the walls of one institution and obtain accurate results;
- all medical personnel work in one team, so any specialist can be involved in solving problems with abortion;
- extensive experience in vacuum aspiration has been gained;
- medical confidentiality is guaranteed;
- attentive and polite attitude, help from a psychologist.
Abortion of any kind causes damage to a woman’s body. Choosing a clinic and doctor is very important to minimize risks and give birth to a healthy child in the future.
Publication date 2019-12-03
Answers to frequently asked questions:
- How to get tested for gynecological diseases?
- What diseases does a gynecologist treat?
- What tests can be done by a gynecologist?
- How to prepare for an appointment with a gynecologist?
- Where to go with a gynecological problem?
- What symptoms should you consult a gynecologist for?
- How often should you visit a gynecologist?
- What diagnostics can a gynecologist perform in your clinic?
- What gynecological equipment do you have in your clinic?
- Gynecological care in the clinic
- Gynecological care at home
- How to call a gynecologist at home?
- How to make an appointment with a gynecologist?
Frozen pregnancy
Frozen pregnancy - what to do?
This situation is considered an emergency for a woman. Therefore, the main task is to quickly get rid of the dead fetus and protect your own body from possible complications caused by intrauterine intoxication: endometritis, retrochorial hematoma, bleeding, etc.
How to determine a frozen pregnancy? Could there be an error in diagnosis?
An error is excluded if such a diagnosis is confirmed by the following three indicators:
- Lack of fetal heartbeat.
- The difference in terms determined by the size of the ovum on ultrasound and the estimated obstetric period is recorded. The size according to ultrasound corresponds to the stage of pregnancy.
- The amount of the hormone human chorionic gonadotropin hCG - the pregnancy hormone - does not correspond to the real period and sharply decreases in dynamics. During normal pregnancy, it doubles daily.
__________________________________________________________________________________________________________________________________________________
Cleaning a frozen pregnancy
Cleaning the uterus during a frozen pregnancy or medicinal termination of a frozen pregnancy are the only possible solutions to the problem, and you must trust your doctors in choosing the termination method. The method of termination with vacuum and tablets is outlined in the relevant sections and does not differ from the termination of a normal pregnancy, with the exception of special monitoring of possible complications associated with fetal death.
__________________________________________________________________________________________________________________________________________________
Genetic risks of miscarriage
If a woman wants to find out whether the death of the fetus is associated with genetic factors, then she should know that only with vacuum aspiration or curettage of a frozen pregnancy is it possible to fully take biomaterial for cytogenetic or molecular research. In the case of medical abortion, it is possible to collect abortion material (clots), but it is not always possible to guarantee the presence of chorionic villi in it, by which genetic pathology is determined. In the absence of chorionic villi in the material, genetic research is impossible. The material should be collected in a sterile vial, filled with saline solution and stored in the refrigerator away from the freezer.
Genetic research should begin no later than 24 hours after taking the abortion material.
Scheme of examination and treatment of patients diagnosed with “frozen pregnancy”
Frozen pregnancy. Confirmed diagnosis - collection of anamnesis, ultrasound and HCCG is the evidence base for making a diagnosis.
Medical termination of a frozen pregnancy – it is possible to terminate a frozen pregnancy at the request of the patient if the diameter of the ovum is up to 18 mm. Read more…
Vacuum cleaning during a frozen pregnancy is the preferred method for removing a frozen fertilized egg. Read more... With this type, it is possible to select chorionic villi for histological and cytogenetic studies.
Genetic research in case of a missed pregnancy - allows you to exclude the genetic nature of a missed pregnancy. Read more…
Chorion histology confirms the diagnosis of frozen pregnancy and excludes hydatidiform mole. Read more…
Identification of the causes of frozen pregnancy is a set of studies to exclude possible causes of fetal miscarriage. Read more…
Planning a future pregnancy is a set of measures that ensure the birth of a healthy child.
Where to clean a frozen pregnancy?
The comprehensive methodology for managing patients with this pathology by doctors at the Medservice clinic minimizes the risks of complications. Unfortunately, the clinic’s doctors note an increased number of requests for undeveloped pregnancies, especially in the early stages. Our task is not only to provide primary care to patients, but also to identify the causes of miscarriage and bring our patients to a successful pregnancy.
Answers to questions that interest our patients with frozen pregnancy are presented in the section “Frozen pregnancy. Answers on questions".
The cost of cleaning a frozen pregnancy at the Medservice clinic for up to 8 weeks
| Service | Cost, rub. | What is included |
| 1 cat. difficulties * | 15 000 – 17 000 |
|
| 2 cat. difficulties * | 18 000 – 20 000 | |
| 3 cat. difficulties * | 22 000 – 24 000 | |
| Recommended studies of abortion material | ||
| Cytogenetic karyotyping during surgery at Medservice/in a third-party clinic | 7 000/10 000 | Collection and research |
| or | ||
| Molecular karyotyping | 17 000 | Collection and research |
* the category of complexity depends on the time the deceased fetus was in utero and possible complications in connection with this.
Call online Make an appointment
SEE ALSO:
- Frozen pregnancy. Answers to basic questions
- HCG during frozen pregnancy
- Causes of pregnancy fading
- Signs and symptoms of frozen pregnancy
- Does the belly grow during a frozen pregnancy?
- Tests after a frozen pregnancy
- Cytogenetic study and molecular karyotyping